Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Galen described the spleen as the “organ of mystery,” with functions related to mood and good or ill humors. It was not until the 18th century that the spleen’s relationship to the immune and hematologic systems was appreciated. The complexities and multiplicity of splenic function continue to be the focus of research and observation. Although many of its functions overlap with, or can be assumed by other organs, it is an important regulator of immune response and hematologic homeostasis. The spleen efficiently phagocytoses erythrocytes, recycles iron, recognizes and destroys pathogens, and induces adaptive immune responses. An appreciation for the subtleties of its anatomy and function is important for the physician evaluating patients with many hematologic, immunologic, hepatic, and infectious diseases.
The spleen arises from the mesoderm and, by the ninth week of gestation, layers of the left dorsal mesogastrium condense with the appearance of blood vessels. Sheaths are formed around arterioles by reticular cells and fibers. Macrophages are present and develop phagocytic function by the end of the first trimester. Lymphocytes appear during the fourth month, and a formal delineation between red and white pulp can be identified by the sixth month. Germinal centers do not develop during fetal development, but primitive inactive follicles are evident at birth. In mice, the homeobox gene Tlx1 (formerly known as Hox11 ), which controls the genesis of the splanchnic mesodermal plate, is essential for development of the spleen. Both the basic helix-loop-helix transcription factor capsulin and the Wilms tumor suppressor 1 ( WT1 ) gene are necessary for formation of the spleen. The genetic basis for development of the human spleen is less well understood. The role of the ribosome in splenic development has recently risen to the forefront with discovery of isolated congenital asplenia (ICA) with variable penetrance amongst patients with mutations in ribosomal protein SA, a component of the small subunit of the ribosome. However, to date its exact role has not yet been elucidated. The spleen is capable of supporting hematopoiesis during fetal life and, in a variety of pathologic states, postnatally. The circulation of primitive hematopoietic stem cells in peripheral blood during prenatal life through birth makes it difficult to distinguish hematopoiesis arising from stem cells in the spleen as opposed to the incidental presence of hematopoietic cells within the circulation.
The spleen is the body’s largest filter of the blood. Located directly below the diaphragm and adjacent to the stomach, it is covered by a fibrous capsule with blood vessels, lymphatics, and nerves coated by peritoneal mesothelium. The splenic artery arises from the celiac axis, enters the capsule at the hilum, and branches into trabecular arteries. The trabecular arteries then branch into central arteries and enter the white pulp. The periarterial lymphatic sheath consists of a cuff of T lymphocytes, plasma cells, and macrophages around the central arteries. As the arteries branch, the sheath narrows. B-lymphocyte clusters appear in follicles along the periarterial lymphatic sheath at arterial branch points ( Fig. 156.1 ).
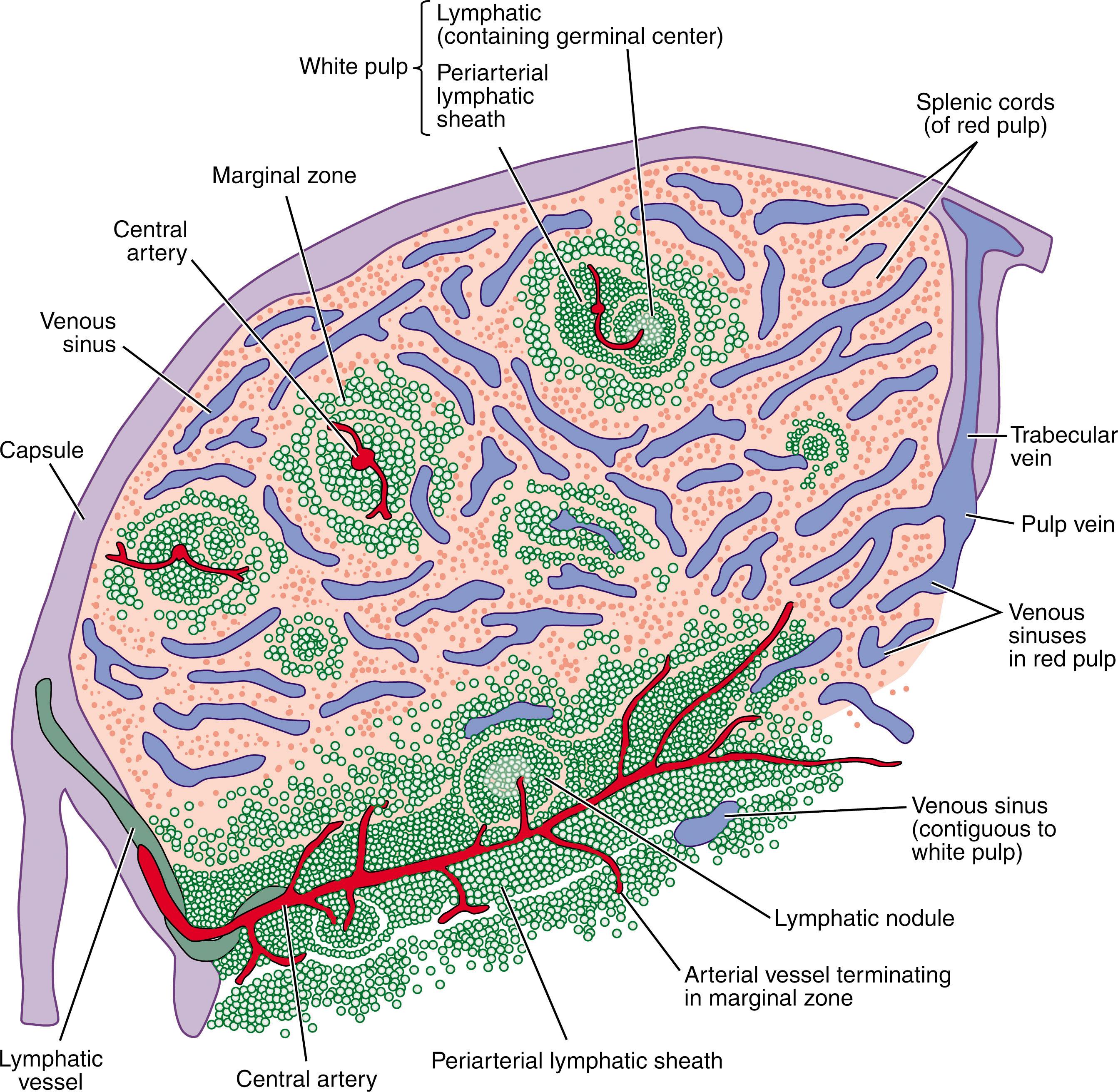
The components of the white pulp are connected by a reticular network and supporting stromal cells. On the cut surface of the normal spleen, white pulp is visible as white nodules approximately 1 to 2 mm in diameter, although their size varies with age and antigenic stimulation. The nodules are fully developed at birth, increase in size during childhood (especially following immunizations and infections), peak during puberty, and involute in adulthood. Uninfected adults with an intact immune system usually do not show evidence of germinal centers. The secondary germinal center comprises a mantle zone of B lymphocytes surrounding the follicle. Antigen trapping and processing take place in the marginal zone of the white pulp.
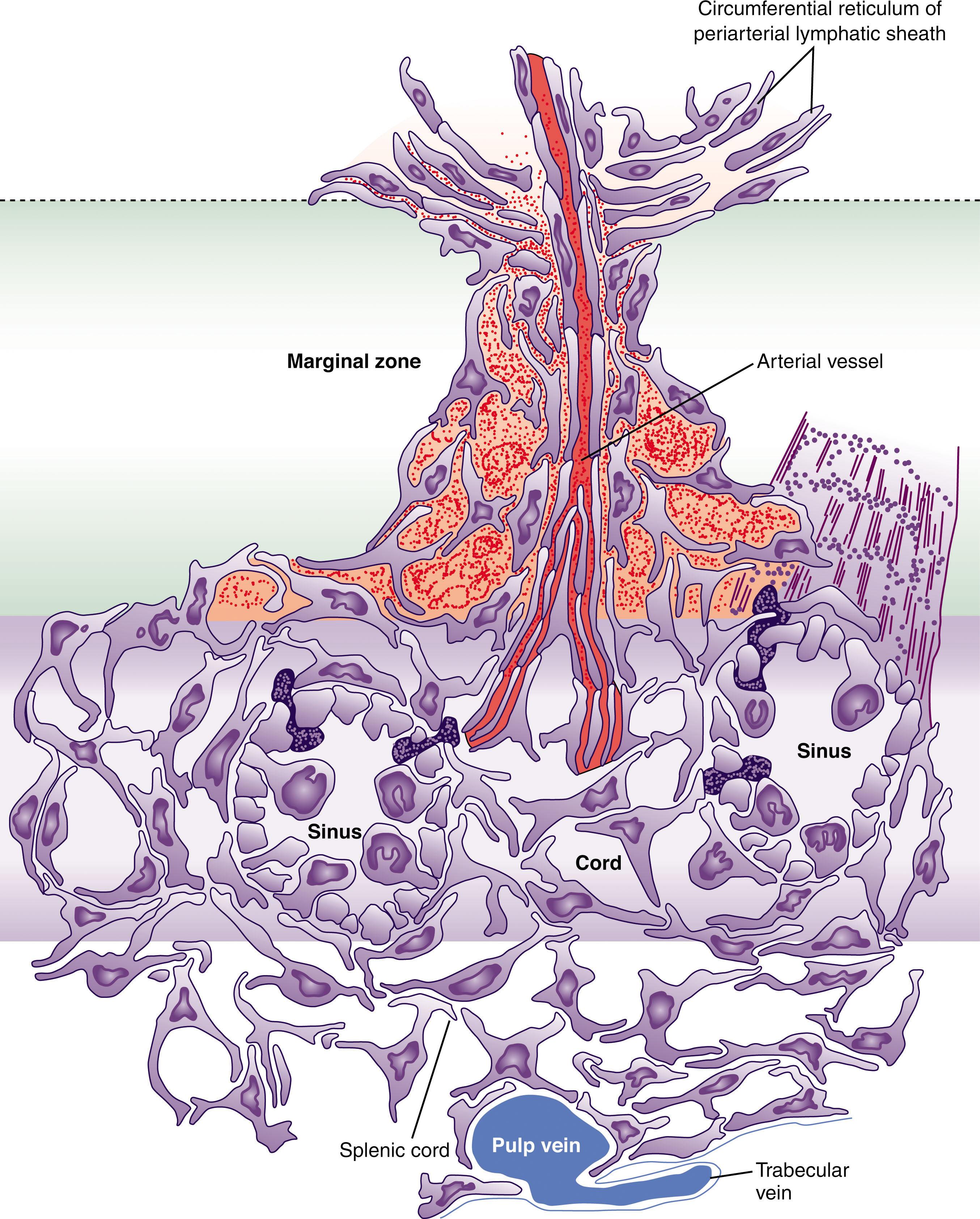
The red pulp of the spleen consists of vascular sinuses, the cords of Billroth, and the terminal branches of the penicilliary arteries ( Fig. 156.2 ). Vascular sinuses are lined with CD8 + littoral endothelial cells that resemble endothelial cells with long processes and a basement membrane with ring fibers that attach to macrophage-derived dendritic processes. No tight junctions or interdigitations connect the cytoplasmic processes. Intact leukocytes, erythrocytes, and platelets are able to squeeze through the potential spaces between these cells and between the ring fibers ( Fig. 156.3 ). Processes of the reticular cells of the cords of Billroth are outside the sinus walls. Endothelial cells line pulp veins but not the cords.
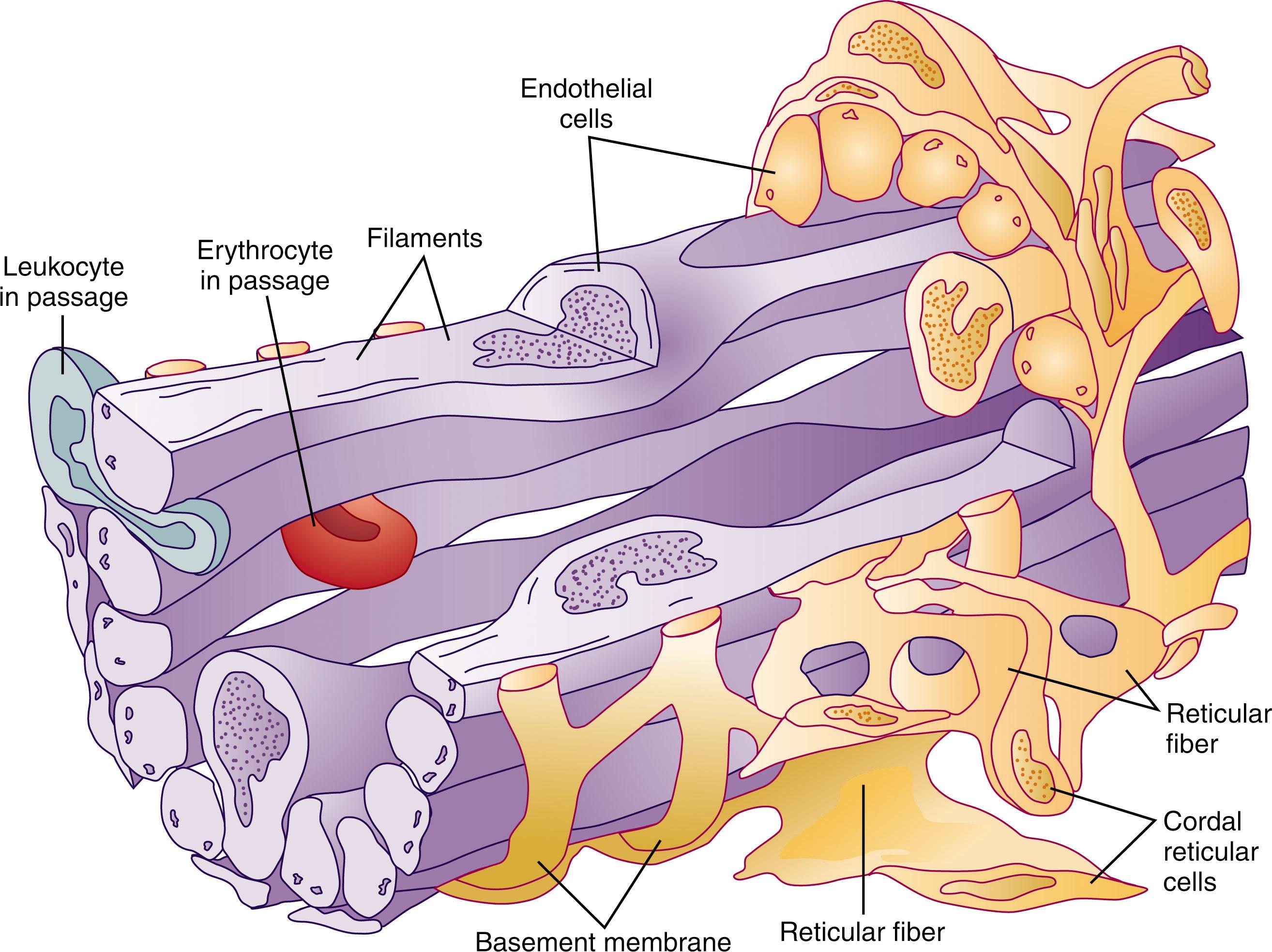
The reticular structure of the spleen facilitates its immune response. Venous sinus endothelial cells contain a plasma membrane-associated network of stress fibers composed of actin and myosin-like filaments. These filaments may cross the plasma membrane and insert into the mesh-like basement membrane. As the fibers tense, they create fenestrations through which erythrocytes must pass if they hope to continue their journey. With age, erythrocytes lose the ability to change their shape and navigate the pathways created by these fibers and are unable to continue into the circulation. The limitation is similar for erythrocytes containing parasitic infections. This mechanism, combined with mannose receptors and Toll-like receptors, helps the infrastructure of the spleen play a role in the host’s overall immune response.
Circulation of blood through red pulp lined with endothelial-like littoral cells represents a rapid and closed circulation. Circulation into the cords is slower and open, thereby permitting the macrophages lining the cord to remove damaged or aged cells.
Accessory spleens are present in up to a third of the population and result from failure of precursor cells to fuse during embryologic development. Usually, they receive blood flow from the splenic artery and are located near the spleen, but they can be distant and mistaken for a tumor when noted on imaging studies or physical examination. Accessory spleens may develop similar conditions as the spleen proper and should be considered within the differential diagnosis for patients who have continued abnormalities after splenectomy.
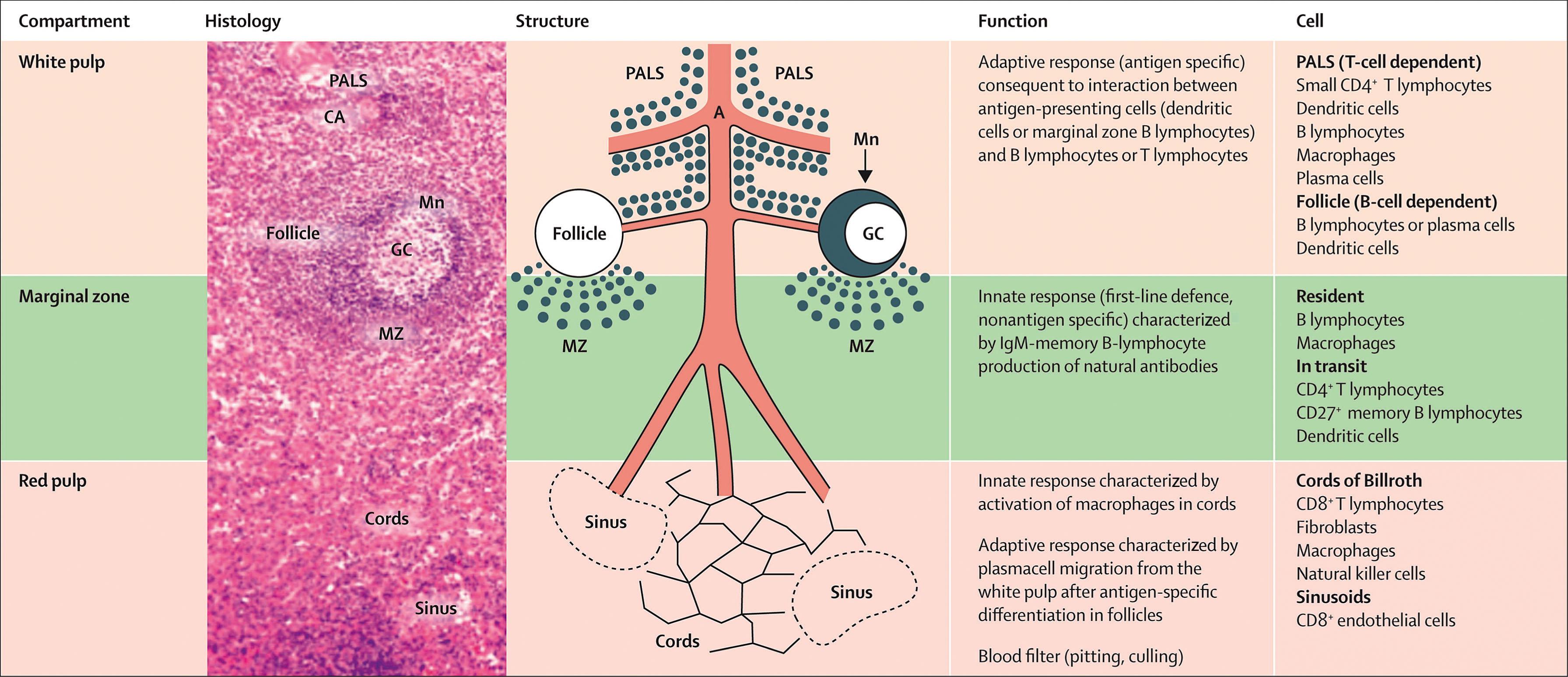
The functions of the spleen and their anatomic locations are summarized in Table 156.1 . Correlation with anatomy and histology are shown in Fig. 156.4 .
| Category | Function | Effector Cells/Areas |
|---|---|---|
| Clearance/Filtration |
|
|
| Immune Response | ||
| Marginal zone | Interaction of antigens with effector cells | Monocytes, lymphocytes |
| Antigen processing | Macrophages | |
| Immune recognition | T cells (periarteriolar sheath) | |
| White pulp | Immunoregulation, antibody production | B cells (lymphoid follicles) |
| Antigen processing, preservation | Macrophages | |
| Red pulp | Phagocytosis | Macrophages, monocytes, neutrophils |
| Hematologic | Hematopoiesis | Cords and sinuses |
| Storage of erythrocytes, platelets, leukocytes | Reticular meshwork, red pulp | |
| Finishing/polishing of erythrocytes | Reticular meshwork, macrophages | |
| Hemostasis | Production of factor VIII, von Willebrand factor | Endothelial cells |
Splenic macrophages dominate the function of the red pulp and are responsible for filtering blood, removing bacteria, and recycling iron. The macrophages in the spleen have distinct features, including distinct Fc-γ receptors, than those derived from blood monocytes.
The venous system of the red pulp enables it to filter whole blood, removing senescent erythrocytes and other blood cells. Arterial blood is delivered to the cords of the red pulp through an open system of reticular fibers, fibroblasts, and macrophages without an endothelial lining. Blood then passes from the cords into the efferent venous sinuses, which are lined with endothelial-like littoral cells with a discontinuous structure. Stress fibers extend beneath the basal plasma membrane and run parallel to the axis of the littoral cells. These cords direct the blood into sinuses through slits modulated in size by the stress fibers. In many animals, the stress fibers and splenic capsule are contractile, giving the spleen the ability to serve as a reservoir of red cells while reducing blood viscosity at rest. In humans, however, there is no evidence that the spleen serves such a function or is capable of significant changes in volume with rest and exercise. To return to the circulation, cells must pass through the slits between venous sinus littoral cells (see Fig. 156.3 ), the size of which may be controlled in part by actin and myosin filaments within the stress fibers in the basal portion of endothelial cells. This surface is believed to be an important site for the culling and pitting of aged or damaged cells.
Compared with when they are young and have a healthy metabolic reserve, older erythrocytes and platelets are unable to tolerate the hostile splenic environment. The spleen has a pH between 6.8 and 7.2, is hypoxic (partial pressure of oxygen [PO 2 ]: 54 mm Hg), and hypoglycemic (glucose concentration approximately 60% of that in venous blood). With age, damaged enucleated cells undergo changes in complex membrane carbohydrates, which facilitate recognition by splenic macrophages and removal from the circulation. Culling describes the destruction of erythrocytes: the normal removal of aging cells or the removal of damaged cells in pathologic states. Most platelets and leukocytes are not removed by the spleen as they age but adhere to vessel walls and migrate into tissues where they die. Pitting refers to the removal of inclusions from within erythrocytes, which are then released back into the circulation. The erythrocyte membrane is in close apposition to the macrophage membrane so that aged or damaged glycoproteins, antibody, or complement on the surface of the cell are easily recognized and activate phagocytosis. Particulate matter—Howell-Jolly bodies (basophilic nuclear remnants), Heinz bodies (clumps of damaged hemoglobin), Pappenheimer bodies (abnormal iron granules), and malarial and other parasites—are removed and the cell is returned to the bloodstream. If membrane-containing adsorbed antibody is present, it is removed and the remainder of the cell is released with changes in shape and volume. Internal vesicles near the erythrocyte membrane appear as if they were on the surface of the cell and are termed pits or pocks . The spleen also normally removes these, with the polished erythrocyte returned to the circulation. The lack of this polishing function can be used to assess splenic dysfunction as the number of pits or pocks per erythrocyte is increased when the spleen fails to remove them.
Macrophages in the liver and spleen are important for recycling iron as erythrocytes are phagocytized and hydrolyzed in the phagolysosome ( Chapter 36, Chapter 37 ). Degradation of hemoglobin releases heme, which is catabolized into biliverdin, carbon monoxide, and ferrous iron (Fe 2+ ). Iron is then either released as a low-molecular-weight species for rapid reuse or stored as ferritin. As ferritin accumulates, it aggregates into hemosiderin. Iron-laden macrophages are a feature of iron overload states in both the liver and spleen. Erythrocytes that are destroyed intravascularly release hemoglobin that binds to haptoglobin. CD163 on the surface of splenic macrophages mediates endocytosis of circulating hemoglobin and haptoglobin-bound hemoglobin.
Iron is released from stores in splenic macrophages in response to the erythropoietic drive expressed by the bone marrow. The precise mechanisms are not well understood. Uptake of iron is mediated in most cells by a divalent cation transporter, the natural resistance-associated macrophage protein 2 (NRAMP2), in recycling endosomes that express the transferrin receptor. NRAMP2 transports ferritin into the cytoplasm across the endosomal membrane. In addition to the more widely expressed NRAMP2, macrophages and monocytes express NRAMP1, which was initially described as an iron-transporting protein affecting resistance to intracellular pathogens. A third molecule involved in iron metabolism in the spleen is lipocalin-2, which is secreted by macrophages and other myeloid cells when activated by exposure to bacterial metabolites. Lipocalin-2 binds to bacterial siderophores and sequesters iron from microorganisms. These and other related molecules tightly link the iron-recycling and host-resistance functions of the red pulp of the spleen.
After stimulation and differentiating in the follicles of the white pulp, antigen-specific plasmablasts and plasma cells lodge in the red pulp, where they are closer to macrophages. A similar translocation occurs in lymph nodes, where plasmablasts migrate to the medullary cords. This translocation occurs after upregulation of expression of CXC-chemokine receptor 4 (CXCR4), which binds CXC-chemokine ligand 12 (CXCL12) expressed in red pulp.
The lymphoid region of the spleen incorporates multiple components of the immune system that are organized to enhance recognition and/or response to pathogens. The white pulp contains lymphoid sheaths around branching arterial vessels, similar to the structure of lymph nodes. Specific chemokines attract B and T cells to their appropriate domains. The periarteriolar lymphatic sheath contains T cells that interact with dendritic cells and circulating B cells. T cells and dendritic cells are attracted to the periarteriolar lymphatic sheath through CC-chemokine ligands 19 and 21. Clonal expansion of activated B cells occurs in follicles. B-cell migration to follicles requires CXCL13. Expression of all these homeostatic chemokines is reduced when signaling through the lymphotoxin receptor or tumor necrosis factor (TNF)-α receptor 1 is absent, which results in disorganization of the domains of the white pulp.
Similar to the migration of leukocytes across endothelial barriers in inflammation, leukocytes leave the bloodstream and enter the white pulp in the marginal zone of the spleen due to the function of G protein-coupled receptors. The marginal zone is an area for cells in transit and home to resident cells with complex interactions. Marginal zone metallophilic macrophages form an inner ring close to the white pulp, marginal zone macrophages form an outer ring, and dendritic cells and B cells are located between the two sets of macrophages. Both trafficking and retention of dendritic cells and B cells involve complex interactions with integrins and other adhesion molecules.
The spleen is important in the recognition of antigens, in the production of antibodies, and in the clearance of opsonized and nonopsonized particles from the bloodstream (see Table 156.1 ). The spleen structure facilitates monitoring of the contents of the blood, with blood flowing through the marginal zone directly along the white pulp. The white pulp is involved in adaptive immunity, whereas the marginal zone is involved in both innate and adaptive immunity ( Table 156.2 ).
| Name | Abbreviation | Function | Splenic Cells Expressing | Recognizes or Affects | Pathogens Recognized |
|---|---|---|---|---|---|
| Toll-like receptor networks | TLR | Pattern recognition of pathogen-associated molecular patterns |
|
|
Multiple bacteria, especially gram negative |
| Natural resistance–associated macrophage protein-1 | NRAMP1 | Solute carrier family 11 (proton-coupled divalent metal ion transporters); phagolysosomal function | Macrophages | Lysosomal targeting |
|
| Natural resistance–associated macrophage protein-2 | NRAMP2 | Proton-dependent cation transporter; iron absorption | Macrophages (apical duodenal cells, erythroid cells) | Impairs bacterial gene expression, protein synthesis | Brucella spp. |
| Sialic acid–binding Ig-like lectin-1; sialoadhesin | SIGLEC1, CD169 | Immunoglobulin superfamily |
|
Mannose | Streptococcus pneumoniae |
| Specific intercellular adhesion molecule 3–grabbing nonintegrin related 1 | SIGNR1, CD209b | ICAM3-binding nonintegrin homologue, mannose receptor | Dendritic cells | Polysaccharide antigens, ManLAM | Fungi, other pathogens |
| Macrophage receptor with collagenous structure | MARCO | Type 1 scavenger | Marginal zone macrophages | Lipopolysaccharide |
|
a These receptors contribute to resistance to infection with pathogens in the absence of prior exposure, specific immune responses, or surface opsonic immunoglobulin or complement.
Trapping and processing antigens is a major function of the marginal zone. Macrophages are abundant here, and the spleen captures more than 5% of the cardiac output (> 250 mL/min), which allows a large volume of blood to be immunologically scrutinized. Antigens penetrate the germinal center where T lymphocytes predominate. Processing carbohydrate antigens is a special function of splenic marginal zone lymphocytes. Marginal zone macrophages express lectin receptors and scavenger molecules.
Splenic macrophages are more sensitive to small amounts of opsonic antibody or complement present on the surface of particles than are macrophages in the liver, lung, or bone marrow. In the absence of a spleen, individuals may fail to remove bacteria with limited opsonic coating, and the production of antigen-specific immunoglobulin (Ig) M is impaired. An asplenic individual has defective recognition of carbohydrate antigens, defective production of IgM early during infection, and defective removal of lightly opsonized particles—all crucial components of response to an invasive infection with encapsulated organisms.
Marginal zone B lymphocytes are sensitive to detection of blood-borne pathogens and rapidly differentiate into either antigen-presenting cells (APCs) or IgM-producing plasma cells. After activation in the marginal zone, some B cells migrate into the white pulp, where they function to activate naive CD4 + T cells.
Similarly, blood-borne dendritic cells activated in the marginal zone migrate into the white pulp. This process appears to be important in control of certain parasitic infections. For example, in Leishmania donovani infection, the spread of infection is inversely proportional to the upregulation or downregulation of CCR7 expression on activated dendritic cells and migration of APCs into the white pulp. In human immunodeficiency virus (HIV)-positive patients with low CD4 T-cell counts (less than 300 cells/μL), there is evidence that IgM memory B-cell depletion might be a risk factor for pneumococcal disease. Effective antiretroviral therapy appears to reverse this depletion, in turn decreasing the risk for pneumococcal infection.
Although the white pulp is both anatomically and functionally similar to lymph nodes, all cells enter the white pulp via the marginal zone rather than through high endothelial venules and afferent lymphatic vessels, exposing them to an environment highly sensitive to detection of blood-borne pathogens. Circulating dendritic cells capture bacteria from the blood and transport them to the spleen, where they mediate the initial differentiation of B cells to plasmablasts or APCs. Activated APCs entering the white pulp activate T cells, resulting in changes in receptor expression that enable them to migrate to the edge of B-cell follicles. Contact with activated T cells induces an isotype switch in follicular B cells, which then migrate to the red pulp and marginal zones or remain in splenic germinal centers. The white pulp of the spleen is the largest mass of lymphoid tissue in the body. The B lymphocytes, which ultimately produce antibodies, predominate in the nearby germinal centers and mantle zones. These areas all increase in size and activity with immunization or infection. The complex interaction between the cells in close apposition, autocrine, and paracrine signaling, and migration of cells into, within, and ultimately out of the spleen, contributes to the extraordinary repertoire of innate and adaptive immunity within the organ. Changes in splenic architecture are quite dramatic with septicemia, the most marked being depletion of splenic B-cell areas that occurs during overwhelming enterococcemia. Bacterial virulence factors appear to contribute to depletion of B- and T-cell areas.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here