Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Children who are victims of severe trauma often sustain musculoskeletal injuries but may also have injuries to other body areas that can be severe and even life-threatening. Early morbidity and mortality are related to injuries to the nervous system, genitourinary system, abdomen, and thorax, whereas long-term morbidity or disability is caused predominantly by injuries to the central nervous system (CNS) and musculoskeletal system. Therefore, careful, coordinated, and integrated management of all injuries is mandatory for minimizing morbidity and mortality. This chapter deals with the assessment of children who have sustained injuries to the musculoskeletal system and other body areas or organ systems. It is not our intent to discuss in detail specific isolated musculoskeletal injuries or their treatment, which are presented in other chapters. Our focus is the evaluation and ranking of treatment options for a multiply injured child who has sustained musculoskeletal trauma; special consideration is given to the aspects of care that may differ as a result of multiple rather than isolated injuries. Much of the material in this chapter is adapted from the American College of Surgeons (ACS) Committee on Trauma, Advanced Trauma Life Support for Doctors (ATLS), Ninth Edition.
The multiply injured child must be approached with a different mindset than an adult.
Early resuscitation is essential.
Falls and motor vehicle accidents account for the majority of polytrauma in children.
Surgical treatment is more often employed to facilitate overall care of the child.
It has been well documented in both adult and pediatric literature that an individual with multiple injuries must be treated differently from individuals in whom similar injuries have occurred in isolation. Assessment and treatment of a multiply injured child may also differ from that of an adult. The anatomic, biomechanical, and physiologic differences in the musculoskeletal systems of adults and children have an important influence on orthopedic treatment, as well as injuries to other body areas and organ systems.
Anatomic differences in the pediatric skeleton are multiple and vary with age and maturity. These differences include the presence of preosseous cartilage, physes, and thicker, stronger periosteum that produces callus more rapidly and in greater amounts than in adults. Because of the effects of age and growth, children vary in body size and proportions.
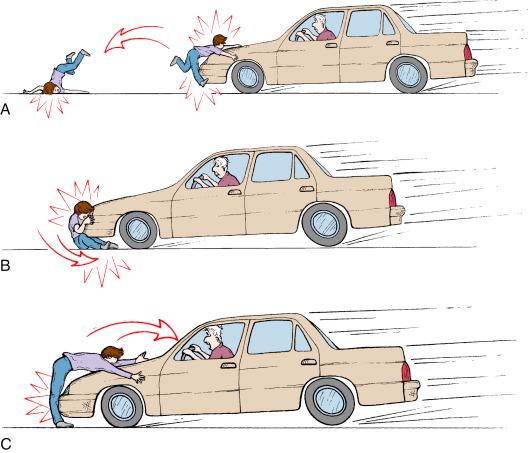
The size of the child is important not only in the response to trauma but also in the severity and constellation of injuries. Being variably smaller, children sustain a different complex of injuries than adults in a similar traumatic situation as well as a higher frequency of polytrauma. An adult pedestrian struck by a motor vehicle is likely to sustain an injury to the tibia or knee because these structures are at the level of the automobile’s bumper. In children, depending on their height, the bumper can cause a fracture of the femur or pelvis or, in toddlers, a chest or head injury. Because the mass of a child’s body is proportionately less, a child is much more likely to become a projectile when struck and may sustain further injuries caused by secondary contact with the ground or another object. A classic example is the Waddell triad, which consists of an ipsilateral femoral shaft fracture, chest contusion, and contralateral head injury ( Fig. 5.1 ). Because of their smaller size, children are also more likely to be trapped beneath a moving object such as a motor vehicle and sustain crush injuries, fractures, and soft tissue damage. Crush injuries are relatively common in children, and such injuries often result in severe soft tissue loss, which can produce a poorer prognosis.
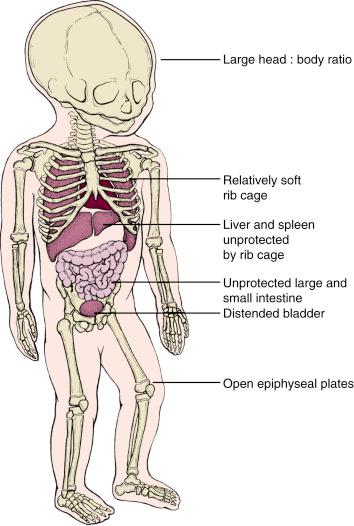
A child’s body proportions, being quite different from those of an adult, can produce a different spectrum of injuries. A child’s head is larger in proportion to the body, and the younger the child, the more extreme this disproportion. This comparatively larger head size makes the head and neck much more vulnerable to injury, especially with falls from a height, because the weight of the head often causes it to strike the ground first. In contrast, adults are more likely to protect themselves with their extremities or try to land on their feet. The relative shortness of children’s extremities and a lack of strength often prevent them from adequately protecting themselves during a fall. This theory is supported by the high incidence of head injuries sustained by young children as a result of falls ( Fig. 5.2 ). Demetriades and colleagues studied pedestrians injured by automobiles and determined that the incidence of severe head and chest trauma increased with age and that femur fractures were more common in the pediatric age groups.
The composition of bone in children is quite different from adult bone. Children, including those who are victims of multiple traumatic injuries, demonstrate unique fracture patterns. These patterns include compression (torus), incomplete tension-compression (greenstick), plastic deformation, complete, and both physeal and epiphyseal fractures. These fracture patterns result from the presence of the physes, the thicker periosteum, and the material properties of the bone itself. Complete fractures occur more commonly in children with multiple injuries because trauma is associated with high-velocity injuries. Biomechanically, the pediatric skeletal system responds differently to an applied force than the adult skeleton does. Pediatric bone has a lower ash content and increased porosity, which are properties indicative of less mineralization. Such bone composition results in increased plasticity and less energy needed for bone failure. This decreases with skeletal maturity.
Bending is the most common mode of failure in long bones. Stress on the tension side of a bone with a low-yield strength initiates a fracture that is followed by compression on the opposite side. As bending continues, the fracture line eventually travels the entire width of the bone. Although pediatric bone is biomechanically weaker, it has a greater capacity to undergo plastic deformation than adult bone. Because pediatric bone yields at a lower force, the stress in the bone is less, and the energy to propagate the fracture is less. These factors account for the compression, greenstick, and plastic deformation fracture patterns. The increased porosity of pediatric bone, which was previously thought to play a major role in the different fracture patterns, is no longer considered a reason for deformation.
Ligaments frequently insert into the epiphyses. As a consequence, traumatic forces applied to an extremity may be transmitted to the physis. The strength of the physis is enhanced by the perichondrial ring and, in some cases, by interdigitating mammillary bodies. In spite of this enhanced strength, however, the physis is not as strong biomechanically as the ligaments or metaphyseal or diaphyseal bone. Consequently, physeal fractures are relatively common in multiply injured children, and ligamentous injuries are less common than in adults. Ligamentous injuries, however, do occur and are probably more frequent than previously reported.
Because pediatric bone is more deformable and fractures with less force, it also affords less protection to the internal organs and other structures. The plasticity of bones can allow internal injuries without obvious external trauma, as reflected in the increased incidence of cardiac and pulmonary injuries without apparent damage to the thoracic cage and a high incidence of abdominal injuries without significant injury to the pelvis, abdomen, or lower ribs. Injuries to the liver and spleen are more common in children because of less rib coverage of these structures, as well as the greater pliability of the ribs. Children also have less soft tissue coverage, including muscle mass and strength, to protect their bodies from trauma. The lower mass of soft tissue may contribute to injury to the internal organs.
Children respond differently than adults to the metabolic and physiologic stress of trauma. Total blood volume is smaller, depending on the size of the child, so less blood loss can be tolerated; hypovolemia develops more rapidly because the smaller volumes lost represent a larger percentage of the total. Comparison of pediatric versus adult patients in the National Trauma Data Bank (NTDB) found that children have earlier mortality than adults, stressing the importance of early resuscitation. The higher ratio of surface area to volume also makes children more vulnerable to hypothermia. Multisystem organ failure tends to occur early during hospitalization and resuscitation, affecting all organ systems at once. In adults, multisystem organ failure usually happens 48 hours after injury and occurs in a sequential order starting with the lungs. The metabolic response is also significantly different between adults and children. Whereas adults have a significant increase in their metabolic rate from the stress of trauma, children have minimal or no change. This minimal response to stress is believed to be caused by the significantly higher baseline metabolic rate of children, which needs to be increased only a small amount to accommodate the increased metabolic demands. The accelerated metabolic rate, together with the ability to metabolize lipid stores, provides a possible explanation for the increased survival rates in children after severe trauma. Adults also appear to have a significant systemic inflammatory response to trauma that does not occur as severely in children. Conversely, children have a robust local inflammatory response at the tissue level that helps not only with accelerated healing but also with minimizing the systemic insult.
Physiologically, pediatric fractures have the capacity to heal rapidly, remodel, and overgrow if the physis is uninjured, and become progressively deformed or shortened if the physis is injured. For these reasons, pediatric fractures secondary to severe trauma require careful management. Musculoskeletal morbidity is a common sequela of multiple traumatic injuries. The ultimate consequences of injury are often not known for many years, and long-term follow-up is recommended.
Trauma is the leading cause of death and disability in childhood. It accounts for more than 50% of all deaths in children compared with 10% in the overall population of the United States. More than 10,000 children die in the United States each year from serious injury, and almost one in every four children requires treatment in the emergency department each year for injuries. An epidemiological study investigating from 2000 to 2011 found decreasing mortality rates, decreasing inpatient discharge rates, and increasing injury severity rates with time. Fortunately, most injuries in children are minor; the most common are caused by falls resulting in injury to a single extremity, usually the upper extremity. Chan and associates showed that approximately 13% of the children being evaluated in the emergency department of an urban teaching hospital had serious injuries. There is a bimodal age distribution of traumatic injuries in children: in the first year of life and later through the adolescent years. Although this bimodal distribution holds true for both genders, males have a higher overall incidence of trauma as well as a more dramatic increase in traumatic incidents during adolescence, with motor vehicle accidents a common mechanism in adolescents. The majority of injuries in the earlier years occur where younger children spend the most time, usually in or about the home. It is important to remember that child abuse is also a cause of multiple injuries, particularly in very young children.
According to the ACS NTDB Report for Pediatrics in 2012, falls and motor vehicle accidents remain the two most common mechanisms of injury in children. Motor vehicle–related deaths are the most common causes of fatality in pediatric trauma. When separated by age group, falls are the most common cause of trauma in children younger than 10 years, whereas at 10 years and older, motor vehicle accidents are much more frequent as a mechanism of injury.
Most pediatric injuries are caused by simple falls, which account for approximately half of all injuries. According to 2010 data from the Centers for Disease Control and Prevention, unintentional falls were the leading cause of nonfatal injury in all children younger than 15 years. However, they are not frequently the cause of fatality. Musemeche and associates showed that falls occur predominantly in the younger population; the mean age was 5 years, and there was a 68% male preponderance. Of the falls, 78% occurred from a height of two stories or less at or near the home. Most patients sustained a single major injury that usually involved the head or skeletal system, although the incidence and spectrum of injury may vary with age. Long bone fractures predominate in children, whereas the incidence of spinal injuries and the total number of fractures are increased in adolescents. Fortunately, children can survive falls from significant heights, although serious injuries do occur. As would be expected, morbidity and mortality rates increase with the height of the fall. Mortality is usually related to falls of a distance exceeding 10 feet. Pitone and Attia showed that in routine falls, children 2 years or younger fell from a bed or chair and sustained head injuries, whereas those 5 to 12 years of age were likely to fall from playground equipment and fracture an upper extremity.
In the past, falls from windows were noted to be a particular problem in urban areas. Recently, Harris and colleagues demonstrated that there was a decrease in the overall national incidence of falls from windows since 1990, especially in those urban areas in which a prevention program such as “Children Can’t Fly” or “Kids Can’t Fly” had been implemented. Window-related falls are much more common in children younger than 4 years, who are also more likely to sustain serious injuries as a result of the fall.
By far, the most common cause of multiple injuries in children is motor vehicle accidents—accidents in which they are motor vehicle occupants, pedestrians, or cyclists. In a 1989 series of 376 multiply injured children, Kaufmann and colleagues reported that motor vehicle–related accidents accounted for 58% of the overall injuries and 76% of the severely injured children. Marcus and associates reported a 91% incidence of motor vehicle–related mechanisms of injury in their series. Although the mechanism of injury was not analyzed by age, the incidence of motor vehicle–related injuries increases with age. According to the Centers for Disease Control and prevention data from 1999 to 2005, deaths from motor vehicle accidents are lowest from birth to 14 years (3.6–4.4 per 100,000 population), and a peak occurs in the 15- to 24-year-old age group (25.9–28.2 per 100,000). Males in this age group have twice the mortality rate of females. Scheidler and colleagues demonstrated that being an unrestrained child or adolescent and being ejected from the vehicle tripled the risk of mortality and significantly increased injury severity scores. Brown and associates recently demonstrated differences in injury patterns based on the direction at the impact (frontal or lateral) and the position of the patient in the automobile. Lateral impact accidents are characterized by head and chest injuries, whereas front seat passengers had higher trauma scores.
By definition, a multiply injured child has injuries involving more than one organ system. It is critical to recognize, evaluate, and treat all injuries sustained. Although many injuries occur in isolation or in random combination, numerous others have been shown to occur in an associated pattern. One of the more common groups of associated injuries is that described as the Waddell triad—a history of a child being struck by a car and a diagnosis of any one of the triad of injuries (ipsilateral femur and chest injury, contralateral head injury) should alert the physician to evaluate the other associated areas ( Fig. 5.1 ). This admonition holds true for all known injury patterns.
A study utilizing the Kid’s Inpatient Database from 1997 to 2009 found that the rate of spinal injuries increased, with the majority in the 15- to 19-year-old group and secondary to motor vehicle accidents. The presence of facial injuries, including lacerations, contusions, and fractures, has been shown to be associated with an increased incidence of cervical spine injury in both children and adults. The presence of a cervical spine fracture in a multiply injured patient is associated with a 10% increased incidence of a noncontiguous fracture at another level of the spine. Because children are more elastic than adults, the force of injury can be transmitted over multiple segments and result in multiple fractures. In addition, certain anatomic differences have an effect on the type of injury, such as the increased cartilage-to-bone ratio, the presence of secondary ossification centers, variations in the normal planes of the articular facet, and increased laxity. Thus, any child seen with head, facial, or spinal injuries at any level should have a careful evaluation of the entire spinal column, especially a head-injured child who is either comatose or unable to cooperate in the examination. In a multiply injured child, a spinal injury must be assumed to be present until proven otherwise by physical examination and radiographic evaluation. Stabilization of the head and neck should account for the larger head diameter and take care not to place the neck in flexion ( Fig. 5.2 ).
In an automobile accident, the use of a lap belt without shoulder restraint may produce a constellation of injuries referred to as the seat belt syndrome. These injuries in children include flexion-distraction injury to the lumbar spine (Chance fracture), small-bowel rupture, and traumatic pancreatitis. Ecchymosis anywhere along the lap belt distribution should alert the physician to search for these injuries. Head and extremity injuries in this circumstance are unusual. Age is a predictor of elevated risk of abdominal injury in seat belt–restrained children. Children ages 4 to 8 years old are at the highest risk of severe abdominal trauma because they are transitioning from child seats to adult seat belts. As a result, the American Academy of Pediatrics and the National Highway Traffic Safety Administration recommend that these children be restrained in a booster seat until they are taller than 4 feet 9 inches. This provides a better fit of the adult seat belt lower on the child’s pelvis to help prevent these injuries. Booster seat legislation appears to be associated with a decrease in the mortality rate in children ages 4 to 7 years old involved in motor vehicle accidents. The unrestrained passenger, however, is subjected to devastating amounts of energy in the absence of the “ride down” effect afforded by restraints. A recent study reported that two-point and three-point restrained children have an increased likelihood of thoracolumbar and flexion-distraction injuries, whereas car seat, booster, and unrestrained children have an increased likelihood of cervical spine injuries.
The pediatric thorax has a greater cartilage content and incomplete ossification, which makes fractures of the ribs and sternum uncommon. Severe thoracic injury to the heart, lungs, and great vessels can be present with little external sign of injury or apparent fractures on chest radiographs. Fractures of the first and second ribs are a marker for severe trauma in children. Given the increased energy that is theoretically required to fracture the ribs in children, it is not surprising that a study of the National Trauma Registry found that pediatric patients with rib fractures had higher rates of associated brain injury, hemothorax, pneumothorax, spleen injury, and liver injury as compared with adults.
Multiple rib fractures are also a marker of severe trauma in pediatric patients. Garcia and associates reported a 42% mortality rate in pediatric patients with multiple rib fractures; the risk of mortality increases with the number of ribs fractured. They found that a head injury with multiple rib fractures signified an even worse prognosis: the mortality rate was 71%. Similar results were reported by Peclet and colleagues. Because head injuries are associated with a higher incidence of mortality and long-term disability, it is critical to recognize this relationship. Multiple rib fractures in a child younger than 3 years should also alert the physician to the possibility of child abuse; 63% of the patients in this age group in the series of Garcia and associates were victims of child abuse. Multiple fractures in different stages of healing are also a sign of child abuse and should raise the physician’s suspicion accordingly (see Chapter 20 ).
Pelvic fractures in children are uncommon and, as in adults, usually the result of high-velocity trauma. As opposed to adults, children have greater plasticity of the pelvic bones, thicker cartilage, and increased elasticity of the symphysis pubis and sacroiliac joints. Simple or isolated, nondisplaced pelvic fractures have low morbidity and mortality rates and tend not to be associated with other injuries ( Fig. 5.3 ). Silber and Flynn demonstrated that patients with open triradiate cartilages were more likely to sustain pubic rami and iliac wing fractures, whereas those with closed triradiate cartilages were more likely to sustain acetabular fractures and pubic or sacroiliac diastasis. This is secondary to the immaturity of the pelvis early on in life when the pelvic bones are weaker than the more elastic pelvic ligaments. After the triradiate cartilage closes, the bones of the pelvis become stronger than the ligaments. More severe fractures mandate a careful evaluation for other injuries because a great deal of energy is necessary to cause this type of fracture. Compared with adults, pediatric patients have been found to have less severe pelvic fracture patterns despite high frequencies of high-energy mechanisms and high rates of associated injuries and similar overall mortality rates with pelvic fractures. Associated injuries can include head injuries; other fractures, including open fractures; hemorrhage; genitourinary injuries; and abdominal injuries. A sacral fracture, which is common in pelvic fractures, may have associated neurologic deficits. The presence of severe pelvic fractures should alert the physician to possible injuries to the abdominal and pelvic contents, particularly genitourinary injuries such as urethral lacerations (especially in males) and bladder rupture. Abdominal injuries may include rectal lacerations, tears of the small or large intestine, and visceral rupture of the liver, spleen, and kidneys. Blood at the urethral meatus, a high-riding or nonpalpable prostate gland on rectal examination, and blood in the scrotum are indications of serious damage to the genitourinary system. Such genitourinary complications must be investigated further, usually with a retrograde urethrogram, before an attempt is made to insert a Foley catheter. Rectal or vaginal lacerations indicate that the pelvic fracture may be open. A diverting colostomy may be necessary for these individuals so that the risk of infection is decreased. If a pelvic fracture is diagnosed and if it is necessary to perform peritoneal lavage, a supraumbilical approach is recommended instead of the routine infraumbilical approach because the former approach may avoid false-positive findings secondary to pelvic bleeding. Unstable fractures, such as vertical shear or wide pelvic diastasis, are often associated with significant hemorrhaging and hypovolemic shock secondary to retroperitoneal bleeding (see Chapter 11 ). In general, however, significant hemorrhage requiring transfusion or angiography is rare in children, perhaps because of the ability of their vessels to readily vasoconstrict as well as the smaller caliber of their vessels that contributes to rapid vasoconstriction.

Understanding injury patterns and the types of associated injuries can be helpful in evaluating a multiply injured patient. However, almost any combination can occur in a child, and the injury patterns are most closely related to the mechanism, the total force applied, and the age of the patient. According to Peclet and colleagues, head injuries are most common in child abuse victims, occupants in vehicular accidents, and children sustaining falls; nearly 40% of abused children have injuries to the head and face. In their study, thoracic and abdominal injuries were most common in children with penetrating injuries (gunshot and stab wounds), whereas extremity injuries predominate in bicyclists and pedestrians. These investigators also showed that the types of injuries change with age: burns and foreign bodies account for most injuries to children ages 1 to 2 years compared with a median age of 7 years for pedestrian bicycle injuries and 12 years for gunshot and stab wounds. Falls and traffic-related injuries are most common in children 5 to 10 years of age. Children who sustained injuries from falls are significantly younger than those with traffic-related injuries. The pattern of injuries from falls also changes with age. Sawyer and associates found that adolescents sustain a greater number of vertebral fractures and total fractures per fall than do younger children, who have a greater number of long bone fractures. Because the mechanisms of injury change with age, injury patterns and associated injuries also vary accordingly.
Childhood obesity is a major public health problem in the United States. Obesity in children is defined as an age- and gender-specific body mass index at or above the 95th percentile. Not only are these children at risk of many short- and long-term health consequences, but several recent studies have also suggested that these children may display different patterns of injury than their peers. In a population-cohort study, Kessler and colleagues demonstrated that overweight, moderately obese, and extremely obese children are at an increased risk of fractures of the foot, ankle, leg, and knee. This association was especially strong in those children 6 to 11 years of age. A recent study of children with tibia and femur fractures 2 to 14 years of age who were treated at a level I trauma center found that compared with nonobese children, obese children had significantly higher injury severity scores, a significantly higher rate of abdominal injury, a significantly higher frequency of pelvic ring injuries, a trend toward more spinal column injuries, and more incidences of bilateral tibia and femur fractures. They were also more likely to be admitted to the intensive care unit and had longer hospital stays and greater mortality when adjusted for age but not injury severity score. Another study completed at a level I trauma center found a higher incidence of extremity fractures and a lower incidence of intraabdominal and intracranial trauma in obese children. They also found an increased rate of deep vein thrombosis and decubitus ulcers in these patients.
The impact of obesity on injuries sustained in motor vehicle collisions was investigated in a retrospective database review in 2009. Among children 2 to 5 years of age who were obese, there was an increased risk of severe head, face, and neck injuries and severe thoracic injuries. Severe thoracic injuries and severe lower extremity injuries were more common in obese children 6 to 13 years of age. In the obese 14- to-17-year-old age group, investigators found an increased risk of severe lower extremity injuries but a decreased risk of severe abdominal, head, face, and neck trauma. Severe upper extremity injuries and spinal cord injuries were not associated with obesity in any age group. Although more prospective data are needed, an increased level of awareness for associated injuries and complications should be present when the physician evaluates and treats obese pediatric trauma patients.
A multiply injured child has a spectrum of injuries of varying degrees of severity. The need for a measure of the severity of trauma is well recognized, both to assist in management and as a predictor of outcome. This need has been documented in adult trauma patients, and several systems have been developed, including the Injury Severity Score, Shock Index, Trauma Score, Revised Trauma Score, Glasgow Coma Scale (GCS), Abbreviated Injury Scale, TRISS-Scan (a combination of the Trauma Score, Injury Severity Score, and patient age), Acute Trauma Index, and Hannover Polytrauma Score. Similar systems have been recommended for pediatric patients, of which the most widely used are the Modified Injury Severity Scale (MISS) and the Pediatric Trauma Score (PTS).
Significant controversy exists regarding which is the best trauma scoring system and whether specific pediatric scores are needed. Two studies showed that both the Trauma Score and the TRISS-Scan have the greatest accuracy in predicting survival. The need for pediatric-specific scores was therefore questioned. Nevertheless, the MISS and PTS can be useful in assessing and monitoring the outcomes of multiply injured children.
The MISS represents an adaptation of the Abbreviated Injury Scale (1980 revision), combined with the GCS for neurologic injuries. The pediatric MISS categorizes injuries into five body areas: (1) neurologic system, (2) face and neck, (3) chest, (4) abdomen and pelvic contents, and (5) extremities and pelvic girdle ( Table 5.1 ). The severity of each injury is rated on a scale of 1 to 5: one point for minor injury, two points for moderate injury, three points for severe but not life-threatening injury, four points for severe injury but with probable survival, and five points for critical injury with uncertain survival. The GCS is used for grading neurologic injuries. The usefulness of this scale has been well established in head injuries in both adult and pediatric populations. The verbal component of this score has been modified for children, especially for those younger than 36 months ( Box 5.1 ).
| Body Area | 1: Minor | 2: Minor | 3: Severe, Not Life-Threatening | 4: Severe, Life-Threatening | 5: Critical, Survival Uncertain |
|---|---|---|---|---|---|
| Neural | GCS Score of 13–14 | GCS Score of 9–12 | GCS Score of 9–12 | GCS Score of 5–8 | GCS Score of 4 |
| Face and neck | Abrasions or contusions of the ocular apparatus or lid Vitreous or conjunctival hemorrhage Fractured teeth |
Undisplaced facial bone fracture Laceration of the eye, disfiguring laceration Retinal detachment |
Loss of an eye, avulsion of the optic nerve Displaced facial fracture Blowout fracture of the orbit |
Bone or soft tissue injury with minor destruction | Injuries with airway obstruction |
| Chest | Muscle ache or chest wall stiffness | Simple rib or sternal fracture | Multiple rib fractures Hemothorax or pneumothorax Diaphragmatic rupture Pulmonary contusion |
Open chest wounds Pneumomediastinum Myocardial contusion |
Lacerations, tracheal hemomediastinum Aortic laceration Myocardial laceration or rupture |
| Abdomen | Muscle ache, seat belt abrasion | Major abdominal wall contusion | Contusion of abdominal organs Retroperitoneal hematoma Extraperitoneal bladder rupture |
Minor laceration of abdominal organs Intraperitoneal bladder rupture Spine fractures with paraplegia |
Rupture or severe laceration of abdominal vessels or organs |
| Extremities and pelvic girdle | Minor sprains Simple fractures and dislocations |
Open fractures of digits Nondisplaced long bone or pelvic fractures |
Thoracic or lumbar spine fractures Displaced long bone or multiple hand or foot fractures Single, open long bone fracture Pelvic fractures with displacement Laceration of major nerves or vessels |
Multiple closed long bone fractures Amputation of limbs |
Multiple open long bone fractures |
Spontaneous
To speech
To pain
None
Oriented
Confused
Inappropriate
Incomprehensible
None
Appropriate words, social smile, fixes and follows
Cries, but consolable
Persistently irritable
Restless, agitated
None
Obeys commands
Localizes pain
Withdraws
Flexes to pain
Extends to pain
None
The MISS score is determined by the sum of the squares of the three most severely injured body areas. The MISS has been shown to be an accurate predictor of morbidity and mortality in pediatric trauma. Mayer and colleagues found that scores of 25 points or more were associated with an increased risk of permanent disability. A score of more than 40 points was usually predictive of death. In their initial study, a score of 25 points or more was associated with 40% mortality and 30% disability, whereas a score of 24 points or less was associated with no deaths and only a 1% disability rate. Their mean MISS score for death was 33.4 points; for permanent disability, it was 30.2 points.
Marcus and colleagues used the MISS in their series of 34 multiply injured children and showed a progressive increase in disability and mortality with increasing scores. The mean score was 22 points, with a range of 10 to 34 points. Children with scores of 25 points or less had a 30% incidence of impairment, children with scores of 26 to 40 points had a 33% incidence of impairment, and children with scores of more than 40 points had a 100% incidence of impairment. Contrary to the findings of Mayer and associates, children with scores over 40 were able to survive but with significant disability.
Loder in 1987 also confirmed the relationship of increasing MISS scores with increasing mortality and morbidity in his series of 78 multiply injured children. He reported a mean MISS score of 28 points (range, 10–57 points). No deaths occurred in children with MISS scores of less than 40 points. The mortality rate for those with MISS scores above 40 points was 50%, and above 50 points, it increased to 75%.
Garvin and colleagues in 1990 demonstrated the accuracy of the MISS in predicting morbidity and mortality after pediatric pelvic fractures. Disrupted pelvic fractures had a higher MISS score than did nondisrupted fractures, and the former were associated with an increased incidence of morbidity and mortality.
Yue and associates in 2000 used the MISS in comparing the extent of injuries and the results of nonoperative versus operative or rigid stabilization in the management of ipsilateral pediatric femur and tibia fractures (i.e., the floating knee). The scores were useful in comparing the severity of injuries in both groups of patients. Loder and associates in 2001 demonstrated an increasing rate of complications related to fracture immobilization in patients 8 years or older with MISS scores of 41 points or greater.
The PTS can also be used to predict injury severity and mortality in children. This score is based on six components: size, airway, systolic blood pressure, CNS injury, skeletal injury, and cutaneous injury. Each category is scored +2 (minimal or no injury), +1 (minor or potentially major injury), or −1 (major or immediately life-threatening injury), depending on severity, and these points are added ( Table 5.2 ). One major advantage of this system is that it is based on criteria that can be easily obtained either at the scene of the accident or in the emergency department, and it can thus be used for triage purposes. Tepas and associates in 1988 demonstrated an inverse relationship between the PTS and the Injury Severity Score, as well as mortality, and found that the PTS was an effective predictor of both morbidity and mortality. No deaths occurred in children with a PTS greater than 8 points; those with a PTS less than 0 had 100% mortality. The PTS has also been validated in other studies as a tool for predicting mortality in pediatric trauma patients. The PTS allows for rapid assessment of trauma severity in a multiply injured child, which assists in appropriate field triage, transport, and early emergency treatment of these patients. It is recommended that children with a PTS of 8 points or less be transported to a pediatric trauma center for management.
| Component | Severity Points | ||
|---|---|---|---|
| +2 | +1 | −1 | |
| Size | >20 kg | 10–20 kg | <10 kg |
| Airway | Normal | Maintainable | Unmaintainable |
| Central nervous system | Normal | Obtunded | Comatose |
| Systolic blood pressure | >90 mm Hg | 90–50 mm Hg | <50 mm Hg |
| Open wounds | None | Minor | Major or penetrating |
| Skeletal | None | Closed fracture | Open or multiple fractures |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here