Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An irritable infant is a challenge to the caregiver and medical provider and is a common presenting complaint in early infancy. An irritable infant is defined here as a patient younger than 1 year of age who, according to the caregiver, cries excessively or is excessively fussy without a specific defined time period. In addition, this chapter also addresses issues of an irritable toddler (∼2–3 years of age). There are many causes, but most irritable infants do not have significant underlying pathologic processes. However, there are serious entities that must not be missed ( Table 30.1 ).
| Emergent/Urgent Diagnoses | Nonemergent/Urgent Diagnoses |
|---|---|
| Eyes, Ears, Nose, Throat | |
| Choanal atresia | Otitis externa |
| Corneal abrasion | Teething |
| Foreign body | Stomatitis |
| Glaucoma | |
| Otitis media | |
| Respiratory | |
| Airway obstruction (croup, foreign body) | Upper respiratory tract infection |
| Lower respiratory tract infection (pneumonia, bronchiolitis) | |
| Cardiovascular | |
| Congestive heart failure | |
| Supraventricular tachycardia | |
| Anomalous coronary artery | |
| Myocarditis | |
| Kawasaki disease | |
| Gastrointestinal System | |
| Incarcerated hernia | Constipation |
| Gastrointestinal obstruction (intussusception, volvulus, pyloric stenosis, Hirschsprung disease) | Uncomplicated gastroenteritis Anal fissure |
| Abdominal trauma | Gastroesophageal reflux |
| Peritonitis (appendicitis, spontaneous) | Inappropriate feeding volume or technique |
| Milk or soy protein allergy | |
| Genitourinary System | |
| Testicular torsion | |
| Ovarian torsion | |
| Urinary tract infection | |
| Orchitis | |
| Balanitis | |
| Epididymitis | |
| Musculoskeletal System | |
| Osteomyelitis | Minor, soft tissue injury |
| Diskitis | |
| Septic arthritis | |
| Fractures | |
| Radial head subluxation | |
| Leukemia, neuroblastoma | |
| Skin | |
| Cellulitis | Impetigo |
| Tourniquet syndrome (digit, genitalia) | Dermatitis |
| Insect bites | |
| Minor injury | |
| Central Nervous System | |
| Encephalitis | |
| Meningitis | |
| Increased intracranial pressure (trauma, hydrocephalus, intracranial hemorrhage) | |
| Intracranial mass | |
| Miscellaneous | |
| Drug ingestion | Vaccine reaction |
| Neonatal abstinence syndrome | Poor caregiver-infant interaction |
| Inborn error of metabolism | Normal crying |
| Sepsis | |
| Sickle cell crisis | |
| Physical abuse | |
| Familial pain syndromes | |
Medical providers should also recognize the profound anxiety and stress that infant crying may place on families and other caregivers. Although excessive crying generally resolves with time, the family’s beliefs about the cause of the crying can have a lasting effect on the way they interact with the child and their beliefs about the infant’s health. Caregivers who perceived their infant’s crying as excessive or inconsolable described higher rates of depression, strained family relationships, and guilt about their inability to calm the infant. Excessive crying may even trigger thoughts of harming the infant and is reported as a common trigger for child physical abuse. Additionally, infants with early cry-fuss problems in combination with family dysfunction are at higher risk for ongoing behavioral problems, highlighting the need for early identification and intervention in this population. Therefore, the provider’s response when evaluating an irritable infant should be focused on diagnosing potentially treatable medical conditions including rare disorders and on addressing the caregiver’s understanding and response to the crying.
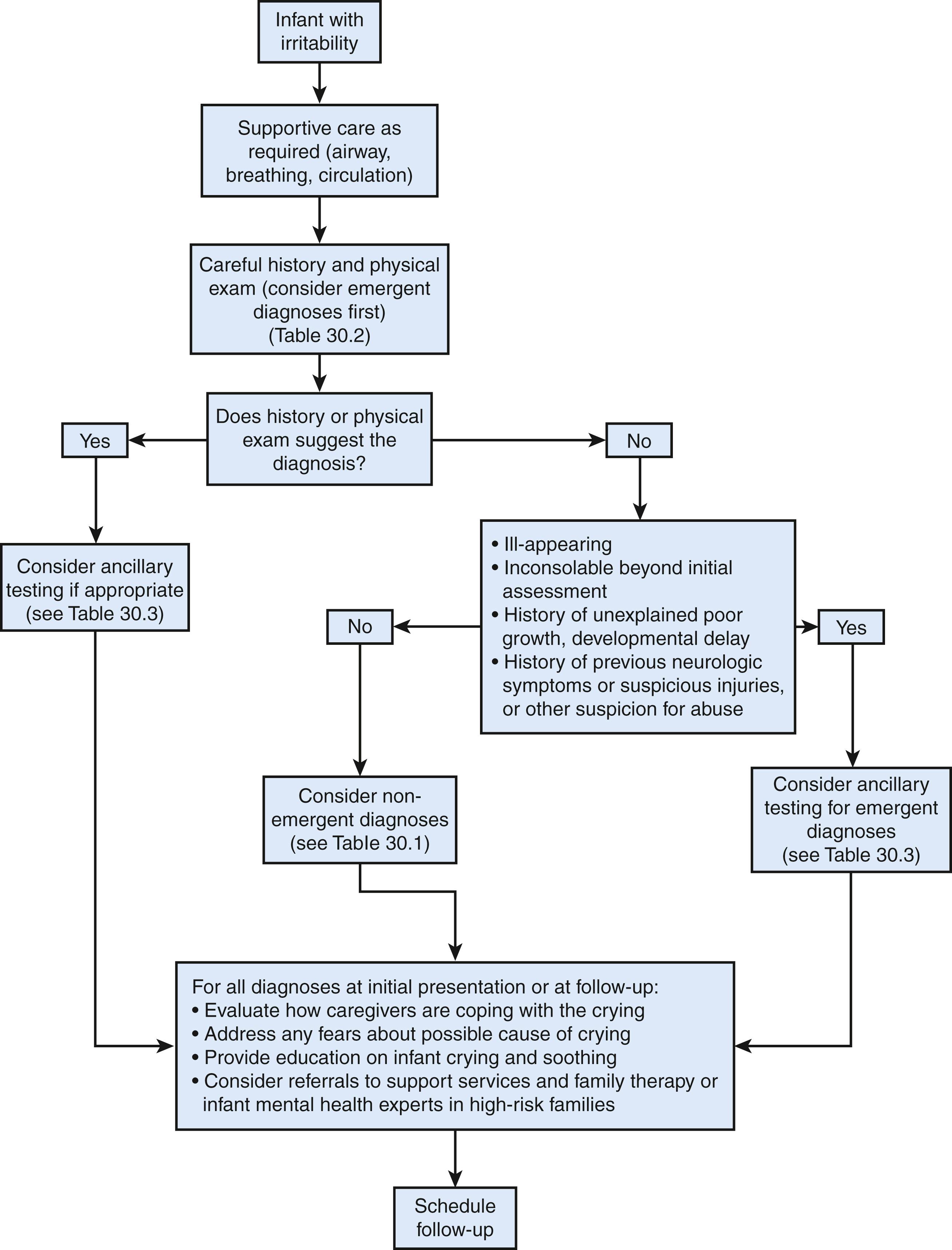
Less than 5–10% of infants who present for medical care due to excessive crying will have a serious underlying etiology. However, a thorough medical evaluation including a detailed history and physical examination is needed to identify the minority of infants with treatable issues, and in healthy infants a thorough evaluation may reassure caregivers. The initial evaluation should focus on ruling out potentially emergent conditions ( Fig. 30.1 ). The physical examination should include a complete examination of all body systems with the clothing removed. Table 30.2 lists elements of the history and physical examination suggestive of emergent and common diagnoses that may present with a chief complaint of crying. The history should be comprehensive, given the wide array of possible diagnoses to consider. The history should include questions about the characteristics of the cry (the time of day, duration, whether it is associated with feeds) and any changes to the infant’s typical crying pattern. Infants with a sudden increase in the frequency and duration of inconsolable crying compared to their normal crying pattern are more likely to have an underlying medical condition. Clinicians should also ask caregivers why they think the infant is crying to specifically address any fears about the infant’s health.
| Review of Systems | Possible Physical Exam Findings | Diagnoses to Consider |
|---|---|---|
| Eyes, Ears, Nose, Throat | ||
|
|
|
|
||
|
|
|
|
|
|
|
|
|
| Respiratory | ||
|
|
|
| Cardiovascular | ||
|
|
|
| Gastrointestinal System | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Genitourinary System | ||
|
|
|
|
|
|
| Musculoskeletal System | ||
|
|
|
| Skin | ||
|
|
|
|
|
|
|
|
|
|
|
|
| Central Nervous System | ||
|
|
|
|
|
|
| Miscellaneous | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
In most cases, the history and/or physical examination will suggest the diagnosis, which can be confirmed with the judicious use of laboratory and imaging studies. However, providers should be aware of potentially serious diagnoses that may present with vague symptoms of fussiness and few other signs or symptoms on physical examination, including neurologic conditions and certain fractures. In very young infants, the neurologic exam is a poor screening tool to detect subtle neuropathology, and intracranial injury may not be accompanied by external evidence of trauma. In cases of physical abuse, an accurate history of injury may be concealed or unknown to the presenting caregiver, and the child may present for medical care after the symptoms of acute injury have resolved. In addition to questions about recent symptoms, medical providers assessing crying complaints should ask about any remote history of bruising or other injury. A history of previous neurologic symptoms, such as episodes of unexplained seizures, apnea, altered mental status, developmental delay, or periods of extreme lethargy, may suggest an occult head injury or other nontraumatic neuropathology. Consider head imaging and a skeletal survey in infants with a history of neurologic symptoms or prior injury.
Growth parameters, including head circumference, should be obtained. Increasing head circumference percentile may point to increased intracranial pressure in infants with otherwise vague symptoms. Though conditions such as constipation, gastroenteritis, and gastroesophageal reflux are most often benign, poor growth or developmental delay may indicate more severe disease or that another medical condition is causing the symptoms.
A urinary tract infection (UTI) may also present with vague symptoms of irritability in infants. A UTI is one of the few conditions in which laboratory or imaging may lead to a diagnosis in the absence of a suggestive clinical picture. Some suggest that a urinalysis and culture should be a standard screening test in infants who present with crying.
When the history and physical examination do not suggest a diagnosis, additional laboratory or radiographic evaluation may be needed. In particular, if the infant is ill-appearing, has evidence of poor growth or developmental delay, or is persistently inconsolable beyond the initial assessment, laboratory and radiographic studies should be done ( Table 30.3 ). Patients may need to be monitored in the hospital until a diagnosis can be established. Some tests to consider include:
A CBC with differential, ESR, and/or CRP measurement (for infection or inflammation, anemia)
Analysis of cerebrospinal fluid (for meningitis or encephalitis)
Blood culture
Serum pH and complete metabolic panel, amylase, and lipase (for electrolyte abnormalities, metabolic diseases, abdominal trauma)
UA and culture (for trauma or infection)
Stool guaiac (for intussusception, gastroenteritis, cow’s milk allergy)
A skeletal survey (for trauma)
CT scan or MRI of the head (for intracranial hemorrhage, mass, or hydrocephalus)
Comprehensive urine drug screen (for ingestion)
| Potential Diagnoses | Ancillary Testing or Consultations to Consider |
|---|---|
| Eyes, Ears, Nose, Throat | |
| Corneal abrasion or foreign body | Fluorescein stain |
| Glaucoma | Ophthalmology consult |
| Foreign body | Radiographs and/or ENT consult |
| Respiratory | |
| Pneumonia or bronchiolitis | Chest radiography, pulse oximetry, nasopharyngeal viral testing |
| Airway obstruction (croup, foreign body) | Chest and/or neck radiography, pulse oximetry, ENT consult for bronchoscopy |
| Cardiovascular | |
| Congestive heart failure | Chest radiography, pulse oximetry, electrocardiogram, echocardiography, CBC, CMP, BNP, troponin, Cardiology consult |
| Supraventricular tachycardia | |
| Anomalous coronary artery | |
| Myocarditis | |
| Gastrointestinal System | |
| Incarcerated hernia | Ultrasonography with Doppler, Surgical consult |
| Gastrointestinal obstruction (intussusception, volvulus, pyloric stenosis, Hirschsprung disease), peritonitis, abdominal trauma | CBC, CMP, amylase, lipase, abdominal and pelvic radiography, abdominal ultrasound, upper gastrointestinal contrast study, abdominal and pelvic CT, air contrast enema for intussusception, Surgical consult |
| Milk and/or soy protein allergy | Hemoccult testing |
| Genitourinary System | |
| Testicular torsion | Ultrasonography with Doppler, Surgical consult |
| Ovarian torsion | Pelvic ultrasonography or CT, Surgical consult |
| Urinary tract infection | UA with culture, CBC, blood culture |
| Musculoskeletal System | |
| Osteomyelitis | CBC, ESR, CRP, blood culture, radiography, MRI, Orthopedics and Infectious Disease consult |
| Septic arthritis | |
| Fractures | Skeletal survey |
| Diskitis | ESR, spine radiographs, spine MRI |
| Leukemia, metastatic neuroblastoma | CBC, bone marrow, abdominal imaging |
| Skin | |
| Cellulitis, infection | CBC, wound culture |
| Central Nervous System | |
| Encephalitis | Lumbar puncture, head CT or MRI, CBC, blood culture, EEG |
| Meningitis | |
| Increased intracranial pressure (abusive or nonabusive trauma, hydrocephalus, intracranial hemorrhage), neoplasm | Head CT or MRI |
| Miscellaneous | |
| Drug ingestion | Comprehensive urine drug screen (with confirmatory testing) |
| Neonatal abstinence syndrome | Urine or meconium drug screen |
| Inborn error of metabolism | CBC with differential, ABG, CMP, serum ammonia, serum uric acid, LDH, blood glucose, aldolase, creatine kinase, UA, urine reducing substances, serum amino acids, urine organic acids, serum acylcarnitine profile, lactate, Genetics consult |
| Sepsis | CBC, LP, UA, urine and blood culture |
| Sickle cell crisis | CBC, reticulocyte count, chest radiography, pulse oximetry |
| Physical abuse | Injury surveillance: Skeletal survey; head CT or MRI in infants <6 mo of age or current or prior symptoms of head injury; AST, ALT, amylase, lipase; comprehensive urine drug investigation screen with confirmatory testing, Child Protection Team consult |
In the consolable infant without history or physical examination findings suggestive of a serious condition, nonemergent causes of crying are more likely (see Table 30.1 ). The most likely diagnosis in infants younger than 4 months of age is above-average crying in a normal infant. However, because a definitive diagnosis has not been established, infants should receive a follow-up evaluation within 24 hours to ensure that a more serious illness was not missed and to address any additional concerns or questions about the crying. This element is especially critical if the clinician has any doubt concerning the establishment of the correct diagnosis.
Paradoxical irritability occurs when a parent attempts to console a crying infant but in the process of holding or cuddling the child, there is an exacerbation of crying. This should suggest that a painful site has been touched or moved and is seen in septic arthritis, osteomyelitis, meningitis, or a fracture.
The distress, frustration, and anxiety that persistent or inconsolable crying may cause caregivers should be recognized and acknowledged with empathy, regardless of the cause. After addressing any urgent medical needs, caregivers should be educated about the normal pattern of infant crying and methods to soothe the infant.
Normal infant crying progressively increases after 2 weeks and peaks in the 2nd month of life, then gradually decreases by the 4th or 5th month. It generally peaks in the late afternoon and evening within the first 6 months of life. At times it may be unrelated to the needs of the infant. Therefore, even in healthy infants some episodes of fussiness will not be soothed with typical caregiver attempts to soothe, such as feeding, cuddling, carrying, and diapering, and may occur for up to 4–5 hours per day. This pattern of crying is consistent among normal infants regardless of caretaking styles, cultural groups, and socioeconomic status, and has been demonstrated even in some nonhuman mammalian species. The pattern may reflect a developmental stage characterized by infants’ increased reactivity to their environment and an immature ability to self-regulate. Though this crying pattern seems to be universal, the frequency and duration of crying varies significantly between infants. This variation is due to several factors, including infant temperament, the caregivers’ response to crying, and likely other unidentified factors.
Caregivers should be reassured that physical contact in the form of carrying and feeding on demand within the first months of life will not spoil the infant. Responding promptly to crying in very young infants before it becomes inconsolable may reduce the amount of crying over the long term by creating a more secure attachment between the infant and caregiver. Room sharing, with the infant’s crib or bassinet in the caregiver’s bedroom, may also decrease infant crying in the first 3 months of life. Conversely, in infants older than 3–4 months of age a consistent daily routine of feeding and sleeping and reasonable delays in caregiver responses to crying may encourage infants to develop autonomous settling and improve infants’ ability to self-regulate. Soothing techniques (swaddling, pacifier use, rocking the baby in a calm environment, or providing some background noise or vibration) are inconsistently effective in studies assessing their efficacy to reduce infant crying. However, these techniques cost nothing and are not associated with adverse effects. It is reasonable to recommend these techniques as an initial response to infant crying.
Despite caregivers’ best efforts, there will be times even healthy infants may not be soothed. The caregivers’ inability to soothe the infant is often their primary source of negative feelings such as frustration, anger, or guilt, creating a loss of confidence in parenting skills and feelings of resentment toward the infant. Infants then respond to caregiver anxiety with increased crying. Caregivers may be reassured by information that bouts of fussing do not necessarily indicate illness or pain but may simply reflect the infant’s inability to regulate the crying once it has started. Medical providers can also reassure caregivers that most infant cry-fuss problems are transient and not necessarily predictive of ongoing behavior problems in childhood. In a prospective, community-based study of outcomes in infants with sleep and cry-fuss problems, only 5% of mothers reported persistent problems at age 2 years.
The clinician must be aware that parental distress from prolonged, unexplained crying can lead to the use of ineffective, inappropriate, or even dangerous remedies. Fennel extract may show promise as a way to decrease crying, although additional study of this treatment and possible negative effects is needed. If herbal teas containing fennel replace infant formula, they may lead to malnutrition and electrolyte abnormalities. Treatments that have been shown to have no significant or reproducible effect in treating crying are acupuncture, reflexology, soy formula, simethicone, gripe water, glucose, sucrose, dimethicone, fiber-enriched formula, and the introduction of lactase enzyme into the infant’s milk. Treatment with anticholinergic drugs (dicyclomine hydrochloride, dicycloverine, and cimetropium bromide) was effective in reducing infant crying but is associated with unacceptable side effects. In addition, several reports have been published of hospitalization or death in infants treated for excessive crying with sedating medications such as dextromethorphan and diphenhydramine, dimenhydrinate, and opiates. Clinicians should counsel caregivers about the dangers of using these medications in young infants.
Given the stress that crying can place on a family and the fact that all families will inevitably be faced with the challenge of a fussy infant, this education should be a routine part of each well-child evaluation in the 1st year of life. It should not only be given to the caregiver who presents with the child for medical care, but also to all adults who will be caring for the child.
More intensive educational and behavior modification interventions directed toward families with persistently fussy infants have shown promise to reduce crying, improve parent-child relationships, and positively influence behavioral development in infants. Successful programs generally assess and address caregiver needs, sources of vulnerability, and infant health. They also provide respite and educate families about infant crying, soothing, and ongoing emotional care. In addition, multidisciplinary approaches may include family therapy or referrals to perinatal and infant mental health experts who can support caregiver-infant interactions.
Caregiver perceptions of prolonged or inconsolable crying place the infant at risk of abuse; caregivers may smother, slap, or shake their baby in response to crying. Crying is a common stimulus for abusive head trauma, and the abuse is often repeated because the head injury stops the crying.
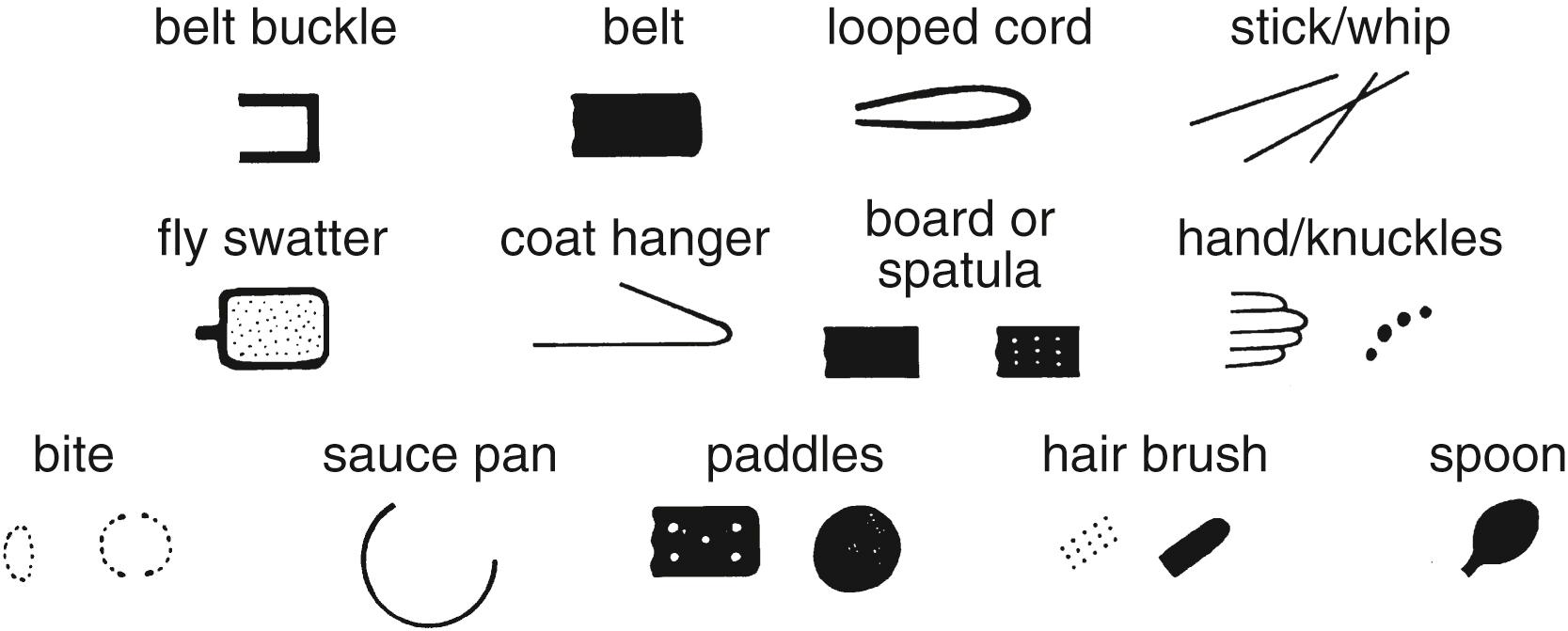
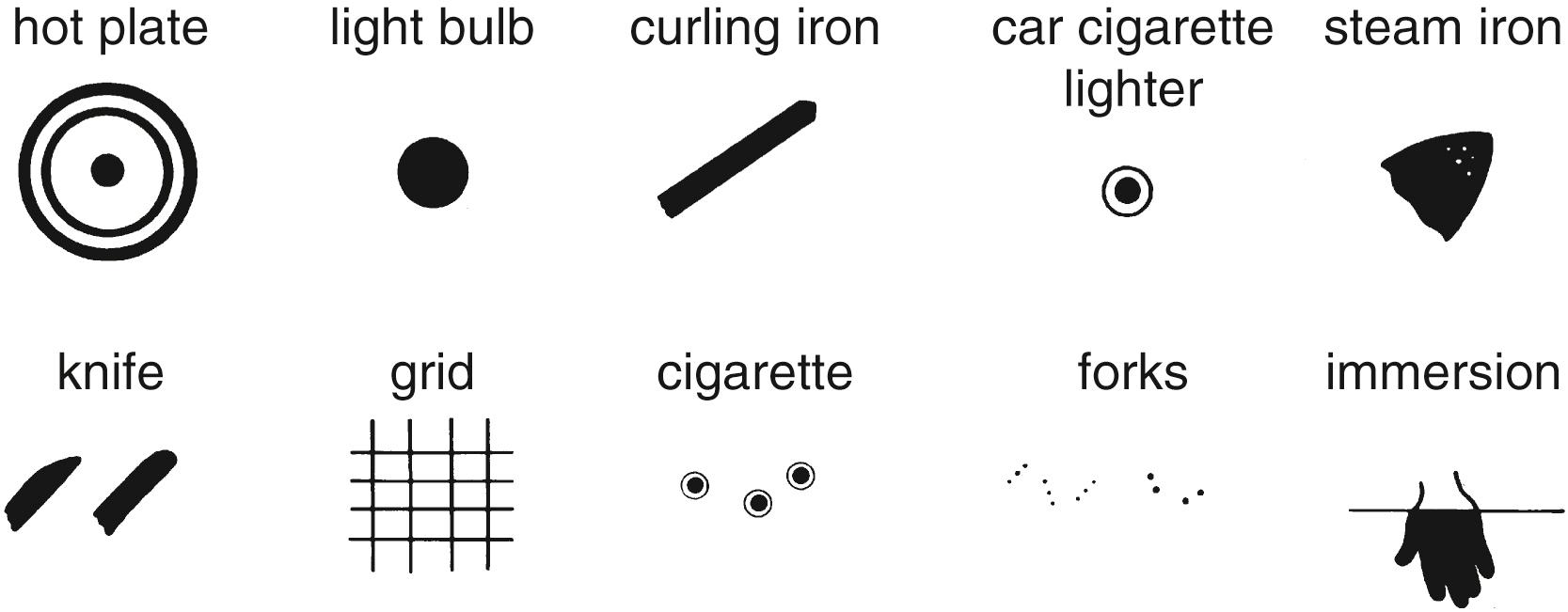
Any injury in a noncruising infant raises concern for abusive trauma and should prompt an evaluation for additional injuries. In older infants and children who can independently ambulate, most accidental bruising occurs over bony prominences on the anterior surface of the body. Bruising to the ears, neck, genitals, and buttocks is unusual in nonabused children ( Table 30.4 ). Abusive bruises tend to be larger, often clustered, and associated with other cutaneous injury. Patterned injuries and any significant, unexplained, or poorly explained injury also may suggest abuse ( Figs. 30.2, 30.3, and 30.4 ). The purpose of additional testing when infants present with suspicious findings is injury surveillance and identification of medical conditions that may mimic abusive trauma. The absence of additional injury does not rule out abuse. Even in isolation, the presence of a suspicious injury places the infant at risk for more severe ongoing abuse. In infants who were ultimately diagnosed with physical abuse, almost 30% of the infants had a history of previous, more minor suspicious injuries. Medical providers were reportedly aware of these injuries in 40% of cases but did not recognize them as concerning ( Table 30.5 ). If there are doubts about whether an injury should be considered suspicious or what tests are indicated, providers should consult a child abuse specialist.
| Locations That May Raise Concern for Abuse | Common Locations of Accidental Injury in Mobile Infants |
|---|---|
| Any bruising in a precruising infant Upper arms Soft parts of the trunk Ears Soft parts of the face Neck Genitals Buttocks Hands and feet |
Nose Shins Bony prominences of the trunk Occiput Forehead Chin |

|
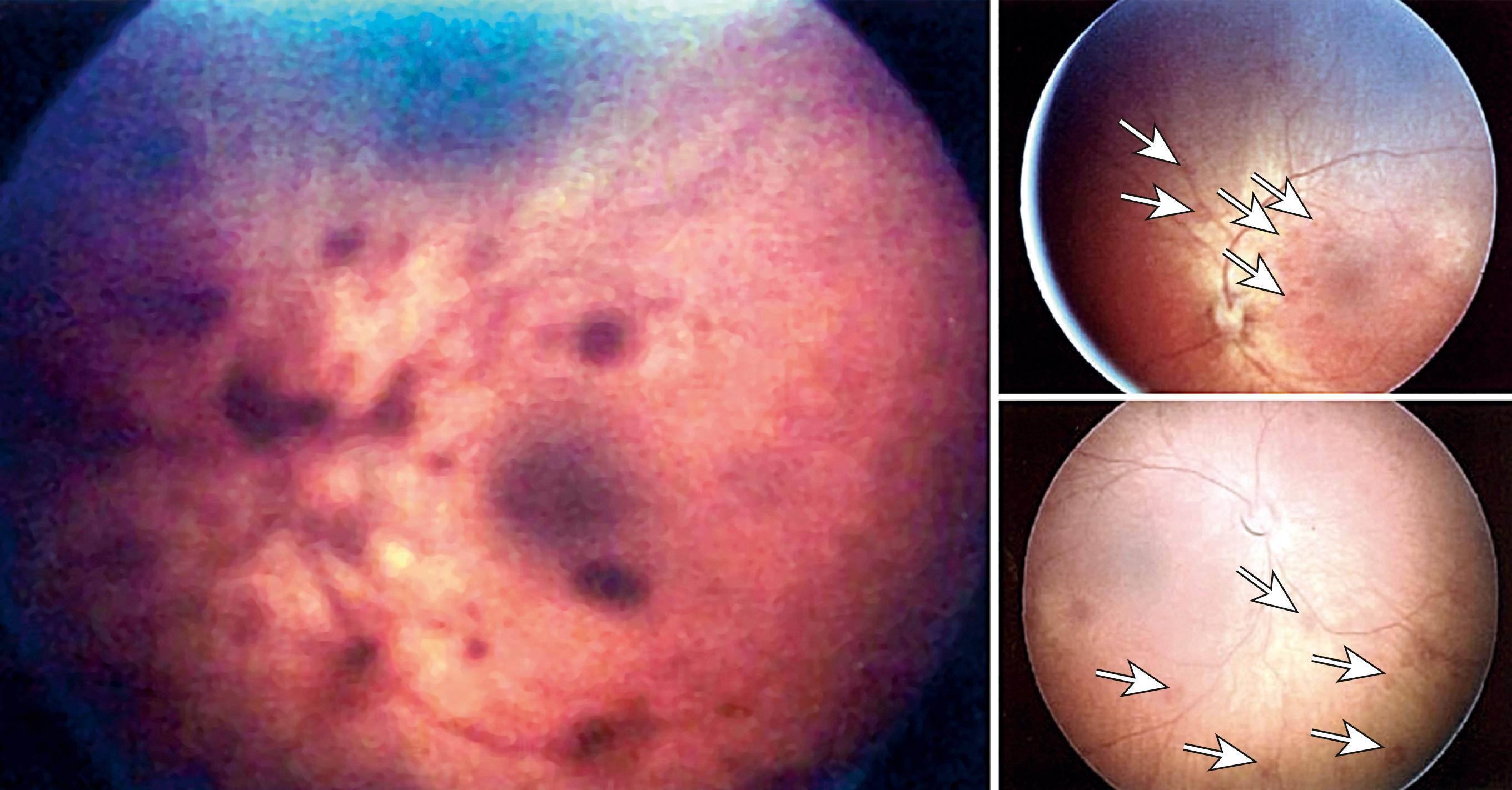
An evaluation for suspected child abuse may need to include imaging studies ( Table 30.6 and Fig. 30.5 ) as well as an eye exam by an experienced ophthalmologist looking for traumatic retinal hemorrhage. Retinal hemorrhages may occur in a significant number of normal neonates after birth; over 75% resolve by 10 days of life, while all resolve by 2 months. Retinal hemorrhages atypical for a neonate or after 1–2 months suggest child abuse ( Fig. 30.6 ).
High-Specificity Findings
Moderate-Specificity Findings
Low-Specificity Findings
|

Medical providers are in a unique position to identify infants at risk for maltreatment when they present for medical care, and to provide education and resources to high-risk families. In infants hospitalized for abusive head trauma, the majority of victims’ caregivers sought medical care for excessive crying prior to the abuse. Multiple phone calls and visits to the pediatrician for excessive crying is a warning sign that it is causing significant distress in the family. Ask caregivers how the crying is affecting the family and address any feelings of guilt or frustration. Clinicians can also ask how caregivers typically respond to the crying. All families who present with a fussy infant should be encouraged to seek support and periodic relief from the infant’s care. Instruct the caregivers to safely place the infant in a crib or other safe location and walk away for a short time if they feel frustrated and at risk of harming the infant.
The definition of infantile colic varies within the medical literature. The most commonly used definition is derived from Wessel’s Criteria, where crying occurs for at least 3 hours a day, at least 3 days a week, for at least 3 weeks in an otherwise healthy infant. Crying from colic generally occurs in the evenings, usually starts between 3 and 21 days of age, peaks at ∼6 weeks, and subsides by 3–4 months of age. During crying bouts, parents describe that colicky infants often flex their legs over the abdomen or may arch their backs with a “pained” look on their face. However, many of these criteria, including the appearance of pain, are also common features of normal infant crying. It is not clear whether the appearance of pain in these infants is due to a true organic etiology or related to caregivers’ anxiety about the duration and unsoothable nature of the cry.
The definition of colic for clinical purposes has shifted to remove strict criteria regarding the duration and characteristics of crying in colic. The 2016 Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers support a diagnosis of colic in an infant who (1) is younger than 5 months of age when the symptoms start and stop; (2) experiences prolonged periods of infant crying, fussing, or irritability reported to occur without obvious cause, which cannot be prevented or resolved by caregivers; and (3) has no evidence of infant failure to thrive, fever, or illness.
A single clear cause of colic remains elusive. Some suggest that the crying from colic is a response to pain from gastrointestinal (GI) dysfunction, such as milk protein or lactose intolerance, gastroesophageal reflux disease, abnormal peristalsis, excessive gas, or altered GI microbiota. However, objective testing for these disorders has not revealed significant differences between colicky and noncolicky infants, and treatments for most have been inconsistently effective. Systematic reviews of complementary and alternative treatments of infant crying have found moderately strong evidence that some probiotics may reduce crying in breast-fed infants, supporting a possible connection between altered GI microbiota and crying in some cases.
Many theorize that colic symptoms are not caused by a single condition, but rather are a common end-point for multiple processes, including infant temperament and caregivers’ responses to the crying. In this view, the term “colic” is used to describe a constellation of common symptoms rather than an underlying disease. Because of the significant overlap in the pattern and characteristics of crying in infants diagnosed with colic and normal infants, colic may represent a point further along a continuum of normal infant behavior. This perspective suggests that, in healthy infants, the clinical focus should be shifted from attempting to diagnose and treat a particular medical condition to providing education and support to caregivers. From a practical standpoint, the clinician should follow the same method of evaluation that would be initiated for any crying infant regardless of whether the crying meets the definition of colic. The duration and frequency of crying in this population can be particularly distressing for caregivers, and education on soothing and coping with the crying should be emphasized.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here