Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The tensor fascia lata (TFL) flap is one of the well-known flaps with a reliable and constant pedicle. This flap has served as a workhorse flap for a variety of indications such as trochanteric pressure ulcers. The TFL muscle has a single dominant pedicle (Mathes-Nahai type I muscle), which sends musculocutaneous perforators to supply the overlying skin. This flap can be used as a muscle, musculocutaneous, osteomusculocutaneous, musculo-osseous flap, or skin flap based on perforator vessels. It can be employed either as a pedicled flap for neighboring defects to cover pressure sores, or to reconstruct abdominal wall, groin, and perineum defects. When necessary, it can be transferred as a free flap to distant defects utilizing microvascular techniques.
The TFL muscle was first used by Wangensteen in 1934 as a pedicled flap without overlying skin to repair large hernia defects. It was proposed as a musculocutaneous flap by Bailey in 1967 for the closure of acetabular defects. Its use has gained greater currency following the extensive clinical application of the flap by Hill et al. in 1978, Nahai et al. in 1978, Bostwick et al. in 1979, and McGregor and Buchan in 1980. Since then, the TFL flap has found considerable popularity in reconstructive surgery for a variety of defects. Recently, the perforator vessel based flap with minimal donor site morbidity has been described by Deiler et al. in 2000 followed by Koshima et al. in 2001.
The TFL muscle originates from the outer lip of the anterior iliac crest between the gluteus medius and sartorius muscles as a broad and flat shaped tendon extending 5 cm along the crest toward the anterior superior iliac spine. The muscle, located on the lateral side of the proximal thigh, continues as a band-like aponeurosis and inserts onto the iliotibial band by way of the fascia lata at the junction of the upper and middle thirds of the thigh. The main functions of the TFL muscle are flexion and abduction of the hip, extension of the knee, and tightening of the iliotibial tract, which stabilizes the hip and knee in the standing position mainly assisting other thigh muscles. It can be considered as an expendable muscle since there are other muscles that can serve the same functions.
transverse branch of the lateral circumflex femoral artery
Length: 5 cm (range 4–7 cm)
Diameter: 2.5 mm (range 2–3 mm)
The lateral femoral circumflex artery invariably originates from the lateral side of the deep branch of the femoral artery 8–10 cm inferior to the anterior superior iliac spine. It travels laterally posterior to the femoral nerve divisions, between the rectus femoris and vastus lateralis muscles and divides into the ascending, transverse, and descending branches that nourish the posterior and lateral thigh musculature as well as the overlying fascio-adipocutaneous tissue. The ascending branch supplies the gluteus medius, gluteus maximus, and vastus lateralis and upper portion of the thigh skin; the transverse branch supplies the tensor fascia lata, the vastus lateralis, and the upper and middle portions of the thigh skin laterally. The transverse branch supplies the TFL muscle entering the anteromedial belly of the muscle 8–10 cm inferior to the anterior superior iliac spine. The transverse branch supplying the TFL muscle divides into three branches before entering the muscle at the hilus: (1) superior, (2) middle, and (3) inferior branches. The superior branch supplies the upper-third of the muscle, giving branches to the iliac crest through the origin of the muscle. The middle branch supplies the middle-third of the muscle. The inferior branch supplies the lower-third of the muscle, and then descends caudally superficial to the fascia lata along the insertion to the iliotibial tract toward the knee. The main vessel is supplemented by an extra vessel derived from the ascending branch in 10–15% of cases, and a vessel derived from the descending branch in 15–20% of cases.
All vascular divisions send an average of 2–4 musculocutaneous perforating branches to the overlying skin, measuring 0.8–1 mm in external diameter. These perforator vessels arise from the muscle proximally, then course superficial to the fascia lata in an axial fashion to supply anterolateral thigh skin. The distal skin of the thigh is nourished by perforator vessels that arise directly from the profunda femoris artery, which are not used as blood supply for the flap on transfer. In order to capture distal thigh skin reliably, a surgical delay procedure is needed. In most parts of the flap – especially in the distal part – inclusion of the fascia maximizes the blood supply of the flap.
All three branches of the transverse branch of the lateral circumflex femoral artery send perforating branches into the skin. The perforator vessel runs in a posterolateral direction in the adipose tissue after penetrating deep fascia, and divides into several branches in the middle of its course and runs a straight line to the subdermal plexus. The blood flow to the skin and lining adipose tissue are supplied mainly by the perforator, and partially by the capillary network in the adipose tissue. Aggressive thinning without leaving a large cuff of fat may sacrifice the blood circulation through this network, resulting in a less reliable area of skin.
the muscle is a type I muscle, so there is no minor pedicle. However, the distal skin of the thigh is nourished by perforator vessels arising directly from the profunda femoris artery.
venae comitantes of the transverse branch of the lateral circumflex femoral artery
Length: 5 cm (range 4–7 cm)
Diameter average 2.5 (range 2–3 mm)
There are usually two venae comitantes traveling with the accompanying artery.
although there are perforators in the distal aspect of the skin that drain directly into the deep femoral vein, these veins could not be considered as secondary venous drainage for the standard flap.
Length: 7 cm (range 5–12 cm)
Diameter: 2.5 mm (range 2–3 mm)
Theoretically, venae comitantes of the vascular pedicle of the anterolateral thigh flap, which eventually drain to the lateral femoral circumflex system, can potentially be used to drain the flap or to provide partial or augmented drainage if needed.
Sensory : (see Fig 13.1, Fig 13.2, Fig 13.19 )
The lateral cutaneous branch of the 12th thoracic nerve. This nerve innervates the skin overlying the iliac crest and superior portion of the TFL muscle. The nerve pierces the internal and external oblique muscles in the anterior axillary line, and courses inferior to the iliac crest and 6 cm posterior to the anterior iliac spine. Proximally, its diameter varies from 0.5–2 mm and it has 2–3 fascicles.
The lateral femoral cutaneous nerve of the thigh (L2–L3). The lateral femoral cutaneous nerve of the thigh, a branch of the second and third lumbar nerves, courses in the pelvis beneath the iliac fascia, enters the thigh below the inguinal ligament about 1–3 cm medial to the anterior superior iliac spine, lies just above the fascia lata, and then deep over the sartorius muscle. It enters the cutaneous territory of the TFL flap 10 cm below the anterior superior iliac spine. In the distal direction a few centimeters after reaching the skin territory, it becomes more superficial and divides into anterior and posterior branches It measures 2–3 mm proximally and has 3–4 fascicles.
the superior gluteal nerve (L4–L5, S1)
This nerve also innervates the gluteus medius and the gluteus minimus muscles. The nerve is accompanied by the superior gluteal vessels, descends in an anterior direction after traveling between the gluteus medius and gluteus maximus muscles, and enters the muscle in the posterior surface.
The flap can be harvested as a musculocutaneous flap, osteomusculocutaneous flap, or musculo-osseous flap, or a skin flap only. It can include the fascia lata and part of the iliotibial tract.
Lateral thigh skin (LTS) over the TFL
TFL muscle
LTS + TFL muscle
LTS + TFL muscle + iliac crest where TFL muscle originates
TFL muscle + iliac crest
The flap has a long and large-caliber vascular pedicle that is suitable for vascular anastomosis.
It has a wide, reliable, and consistent skin territory. The variation in vascular anatomy is low and the location of the pedicle is always between the rectus femoris and vastus lateralis muscles.
The skin portion can be transferred as a sensate flap by including the lateral cutaneous branch of the 12th thoracic nerve and/or the lateral femoral cutaneous nerve of the thigh.
The TFL muscle can be transferred as a functional unit by including the motor nerve to the muscle (a branch of the superior gluteal nerve).
It can be harvested with iliac bone for composite defects requiring bone.
It does not require positional change during surgery for most recipient sites in the extremities and head and neck regions.
It allows a two-team approach most times.
Reconstruction of defects around the pelvis and lower extremity can be performed under epidural anesthesia.
The flap can be harvested as a perforator flap and thinned to 5 mm, or it can include the entire skin, fascia, muscle, and bone.
The donor site can be closed primarily if the skin island of the flap is <8 cm or if muscle only is harvested.
The donor site may be difficult to conceal, and when skin grafting is needed for closure, it may result in an unaesthetic appearance.
Unless it is harvested as a perforator-based flap, it may be excessively bulky.
Sacrifice of the TFL muscle may cause minimal functional donor site morbidity, such as loss of knee stability. This seldom occurs and in order to minimize this risk, the skin flap can be elevated suprafascially as a perforator flap. If a small flap is needed, the fascia behind can be sutured back to minimize functional deformity.
The side of the flap chosen depends on the recipient site, or the provision of two teams to work simultaneously in distant tissue transfer. Based on the selection of the flap type, if a perforator-based flap is to be harvested, a Doppler probe can be used to determine the most reliable artery and its course. The thigh is prepared and scrubbed. Shaving the hair is usually optional and depends on the choice of the surgeon, and on the nature and length of hair and on the recipient site.
The area of the thigh and hip are prepared down to the level of the knee. For most cases, it is recommended that the hip and entire leg be prepared in order to facilitate hip and knee flexion when needed.
There is no special test that is used prior to surgery. When a perforator flap is planned, a handheld ultrasound Doppler device is used to locate the perforators. CT or MRI angiography can help in locating perforators.
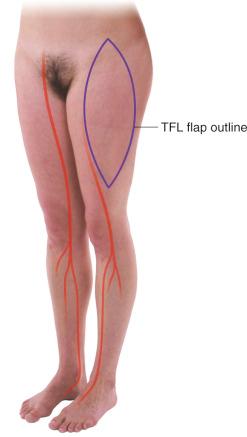
The anatomic landmarks for the flap include the anterior superior iliac spine (ASIS) and the lateral condyle of the tibia. A line drawn from the anterior superior iliac spine to the lateral condyle of the tibia marks the anterior border of the muscle, and a parallel line drawn 3–4 cm posterior to the first marks the location of the posterior border of the muscle. A point marked 8–10 cm (the location of the pedicle depends on the patient's height, so it could range between 8 and 12 cm) caudal to the anterior superior iliac spine on the line extending to the lateral condyle of the tibia, marks the location of the entrance of the vascular pedicle into the muscle belly.
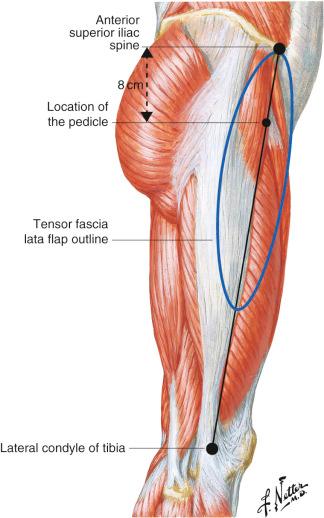
The location where the pedicle enters TFL muscle is not constant and can be found between 8 and 12 cm caudal to the ASIS. Therefore, during the dissection, this fact should be kept in mind.
For the extended version of the flap, the lower marking can be extended to the knee, but usually a delay procedure is needed.
The anterior and posterior marking for the vertical incisions can be extended in an oblique shape proximally and distally at the level of this line for the full, proper exposure of the fascia.
If a neurosensorial flap is planned, the positions of the sensory nerves are indicated as described above and dissection of the nerves continues until the desired length is obtained. Harvesting a relatively wide cuff of subcutaneous tissue around the nerve can be useful to protect neural structures.
The arc of rotation for the pedicled muscle flap reaches to the groin, perineum, great trochanter, ischium, and lower abdominal wall.
When performing local rotation flaps, the origin of the muscle proximally may be disinserted to avoid dog-ear formation.
For perforator flap harvest, preoperative imaging techniques can be useful.

Breast reconstruction: It is not commonly used for breast reconstruction; however, it can be considered as a secondary option because of donor site morbidities such as unsightly thigh scar and thigh asymmetry. The TFL perforator flap is also a versatile option for breast reconstruction in selected cases.
Upper and lower extremities, as well as head and neck defects requiring soft tissue and bone, can be reconstructed with this flap, which can include iliac bone.
It can be used as a neurosensorial flap for various soft tissue defects where sensation is required. Functional muscle transfer can be achieved by performing a coaptation between the motor nerve of the TFL muscle (the superior gluteal nerve) and recipient nerve (i.e., shoulder reconstruction, facial reanimation).
The flap can be designed to rotate anteriorly and superiorly to reach abdominal, perineal, and inguinal defects, or posteriorly and superiorly to cover ischial, trochanteric, perineal, and sacral defects.
The musculocutaneous flap can be planned as peninsular, island, and V-Y advancement flap. Although the skin island of the flap can be designed similarly in both free and pedicled flaps, there are some differences according to requirements and the distance to the recipient defects in pedicled flaps. In pedicled flaps, most of the useful part of the flap is designed in the area distal to the pedicle of the flap, which is 8–12 cm inferior to the ASIS. The arc of the rotation of the flap should be planned considering this location prior to dissection. When used as a rotation flap, the origin of the muscle and its overlying skin can be divided to form an island flap to add mobility around the axis of the pedicle (pivot point).
If the flap is designed as a perforator vessel-based skin flap, it can be rotated more freely.
Length: 13 cm average: 12 cm (range 12–15 cm)
Width: average 4 cm (range 3–5 cm)
Thickness: 2 cm (range 1.5–3 cm)
Length: average 20 cm (range 15–40)
Width: average 10 cm (range 7–20 cm), maximum to close primarily 8 cm
Thickness: average 10 mm (range 5–20 mm)
If the length of the flap is extended beyond 10 cm proximal to the knee or designed longer than 35 cm in an adult patient, a delay procedure is recommended. Based on the authors' experiences, if delay procedure is not performed, the distal skin of the flap has no chance of survival.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here