Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the introduction of reverse shoulder arthroplasty in the 1980s, the treatment of rotator cuff dysfunction has been completely revolutionized. It has allowed improved functional results, as well as an improved quality of life for patients with rotator cuff insufficiency. Previously, those symptomatic patients could only be treated surgically with expectation of a rather limited outcome. Nowadays, reverse shoulder arthroplasty may be indicated for numerous reasons: rotator cuff insufficiency, rotator cuff arthropathy, proximal humerus fractures and fracture sequelae, rheumatoid arthritis, pathologic glenoid morphology, and any kind of revision surgery.
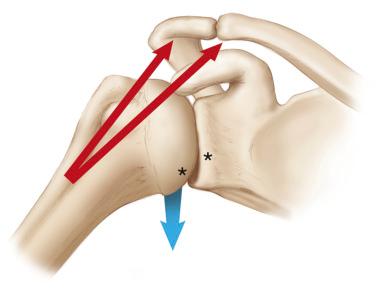
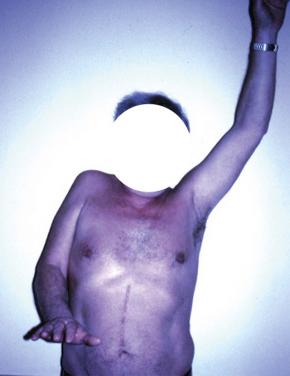
In patients with a rotator cuff insufficiency, the glenohumeral joint can become uncompensated. Depending on the number of the involved insufficient rotator cuff tendons, the shoulder range of motion is impacted in the sagittal and/or vertical plane. Because the shoulder joint is unbalanced in its natural state in both the vertical plane (deltoid stronger than the rotator cuff muscles) and the horizontal plane (four internal rotators stronger than two external rotators), this only becomes worse with aging. The aging shoulder often shows rotator cuff tendon wear, mostly including the supraspinatus and infraspinatus tendons first. That leads to unopposed cranial pull, creating an unbalanced shoulder in the vertical plane ( Fig. 41.1 ). Because the humeral head continues to rise, this creates a cascade of glenohumeral destruction that can be followed by the Hamada classification of rotator cuff arthropathy. Patients with an isolated loss of active elevation or a so-called pseudo paralysis, which describes the painless inability to abduct the arm to 90 degrees while maintaining a normal passive range of motion in the absence of neurologic impairment ( Fig. 41.2 ), are best treated with a reverse shoulder arthroplasty. Reverse shoulder arthroplasty moves the center of rotation distally and medially, allowing the deltoid to effectively transmit moments across the glenohumeral joint and thereby allowing improved forward flexion in a predictable fashion and a rebalancing of the vertical plane of motion.
As the arthropathy worsens, the infraspinatus and teres minor (if atrophic or in some cases torn) can become insufficient, resulting in a horizontal imbalance ( Fig. 41.3A,B ). This causes profound disability that reverse shoulder arthroplasty alone may not sufficiently address. This pattern may result in a combined loss of active elevation and external rotation (CLEER) and rarely may just be found to be an isolated loss of external rotation.
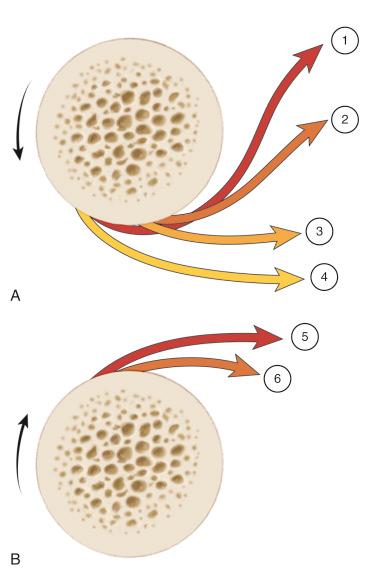
The shoulder itself has a natural predominance to internal rotation (IR) if each function of traversing muscle is reviewed. There are four internal rotators (the pectoralis major, the latissimus dorsi, the teres major, and the subscapularis), whereas there are only two external rotators (the teres minor and the infraspinatus). In the setting of a posterior cuff tear, it is easy to understand how a horizontal imbalance can occur with disruption or partial disruption of either of these external rotators. However, even in the setting of a two-tendon rupture, the teres minor—the dominant external rotator providing up to 40% of strength of external rotation—can experience atrophy in 24% of the cases, further reducing its ability to balance the shoulder. The loss of these muscles creates an environment of four stout internal rotators versus zero. Thus, a rebalancing of the shoulder is imperative in this setting.
In patients with a pseudo paralysis, who additionally have a horizontal imbalance as a consequence of their teres minor and infraspinatus insufficiency (patients with CLEER), activities of daily living are often drastically impacted. The ADLER (activities of daily living [ADL] that require active external rotation [ER]) score was suggested as an objective method to score a patient’s disability by judging their ability to perform everyday tasks, which are dependent on the external rotation of the shoulder ( Table 41.1 , Fig. 41.4 ). Simple tasks, such as shaving, brushing teeth or combing hair, eating, drinking, or opening doors, are classically affected. Therefore in patients with this dysfunction, a tendon transfer in conjunction with the reverse shoulder arthroplasty is indicated.
| Item | Task | Total Points |
|---|---|---|
| 1 | Comb hair | /3 |
| 2 | Shave or apply makeup | /3 |
| 3 | Dress (i.e, put on a shirt or a coat without help) | /3 |
| 4 | Fill a glass with a full bottle (being seated at the table) | /3 |
| 5 | Drink (bring a full glass to the mouth) | /3 |
| 6 | Eat soup (with a full spoon) | /3 |
| 7 | Eat with a fork | /3 |
| 8 | Shake someone’s hand or open a door | /3 |
| 9 | Use a phone (at ear level) | /3 |
| 10 | Write a letter (or sign a paper or typewriter or play the piano) | /3 |
| Total | /30 |
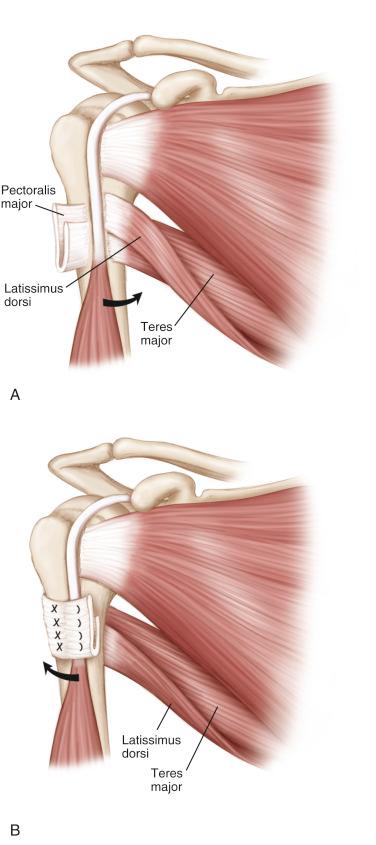
In 1934, L’Episcopo first described the technique of transfer of the latissimus dorsi and teres major (LD/TM) tendons in children with obstetric palsy. The procedure involves transferring both tendons laterally and posteriorly on the humerus, such that the function of the LD/TM changes from internal to external rotation ( Fig. 41.4A,B ). The technique was modified so that it could be performed through a single deltopectoral approach. In the literature, this technique has been established as a viable treatment option for these patients. Alternatively, it is also possible to perform a latissimus dorsi transfer combined with a reverse total shoulder arthroplasty using a two-incision technique with results similar to those described by Gerber et al. In a variation of these two known and established techniques, a latissimus dorsi transfer only through a single-incision technique was recently performed by the authors with equal restoration of the external rotation and even with better IR ability. In the following section, the single-incision modified L’Episcopo (LD/TM) and the single-incision LD transfer only as a variation are described.
This combined procedure involves performing a reverse shoulder arthroplasty with the addition of an LD/TM transfer. The tendons are harvested and passed from medial to lateral posteriorly behind the humeral diaphysis during reverse shoulder arthroplasty.
A variation is the single-incision latissimus dorsi transfer.
Instead of harvesting both the LD and the TM, only the LD is detached from the humerus in a sharp manner and passed around the humerus to the posterior side of the greater tuberosity (near the insertion of the teres minor).
Pain, usually with attempted lifting and at night
Inability to raise arm
Problems related to loss of external rotation:
Moving hand behind head
Reaching mouth
Grooming
Dressing
Writing
See Fig. 41.5 .

Often anterosuperior escape of the humeral head
Loss of active forward flexion
External rotation lag sign
Positive drop arm sign
Hornblower’s sign
See Figs. 41.6 and 41.7 .


Decreased acromiohumeral distance on radiographs
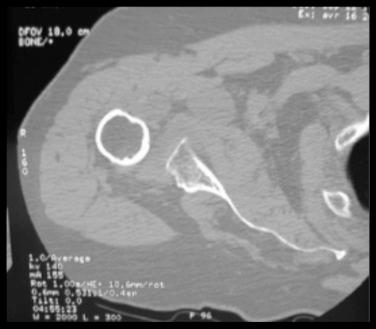
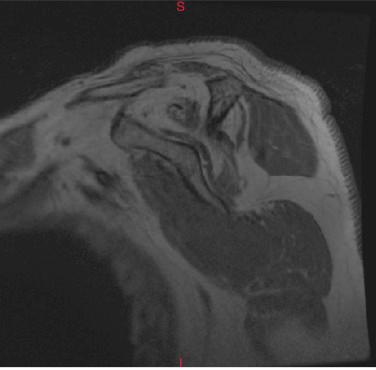
Teres minor atrophy, complete rupture, or fatty infiltration on advanced imaging studies obtained by computed tomography or magnetic resonance imaging
See Figs. 41.8–41.10 .

Nonoperative:
Physical therapy: strengthening of the leftover rotator cuff and the accessory muscles of the shoulder
Corticosteroid injections/nonsteroidal antiinflammatory drugs to decrease pain
Activity modification or cessation
Operative:
In functional shoulders and/or low-demand patients with mostly pain, a subacromial debridement and biceps tenotomy or tenodesis is indicated.
Isolated LD/TM (or LT alone) transfer if well compensated in the vertical plane respecting the contraindications (e.g., irreparable subscapularis tear, Hamada stage 4)
Reverse shoulder arthroplasty with LD/TM (or LD alone) tendon transfer in patients with CLEER
Deltoid
Pectoralis major
Long head of the biceps
Latissimus dorsi
Teres major
Radial nerve
CLEER
Clinically, the aforementioned signs are seen (positive drop arm sign).
Teres minor/infraspinatus rupture, atrophy, or severe fatty infiltration
Hamada stage 3 or higher
Beach chair position
Operative extremity free
Scapula free from operative table
Be sure after beach chair positioning that head is clear from shoulder.
Arm must be free so that assistant can hold and move the arm throughout the operation.
Space behind the operative shoulder must be free to allow for extension and adduction of the arm to dislocate the extremity and perform humeral preparation.
Headholder blocking instrumentation owing to close proximity
If arm cannot be fully extended/adducted, humeral dislocation, canal preparation, and dissection of the LD/TM will become more difficult.
Beach chair operative bed
Reverse shoulder prosthesis – (Tornier AEQUALIS ASCEND FLEX Reversed Shoulder System; Wright Medical, Bloomington, MN)
Shoulder retractors (author prefers Richardson, Hohmann, forked retractors)
Multicolored nonabsorbable sutures for tendon tagging (ETHIBOND 7-0; Ethicon/Johnson & Johnson, Somerville, NJ)
Curved clamp
Cannulated drill for LD transfer only
See Fig. 41.11 .

Single-incision deltopectoral approach
A standard deltopectoral approach is used, with a skin incision of 10–12 cm based proximally over the coracoid process and extending distally in line with the anterior border of the deltoid muscle. The cephalic vein is identified and retracted laterally. The humerus is exposed, and the pectoralis major tendon is identified.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here