Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
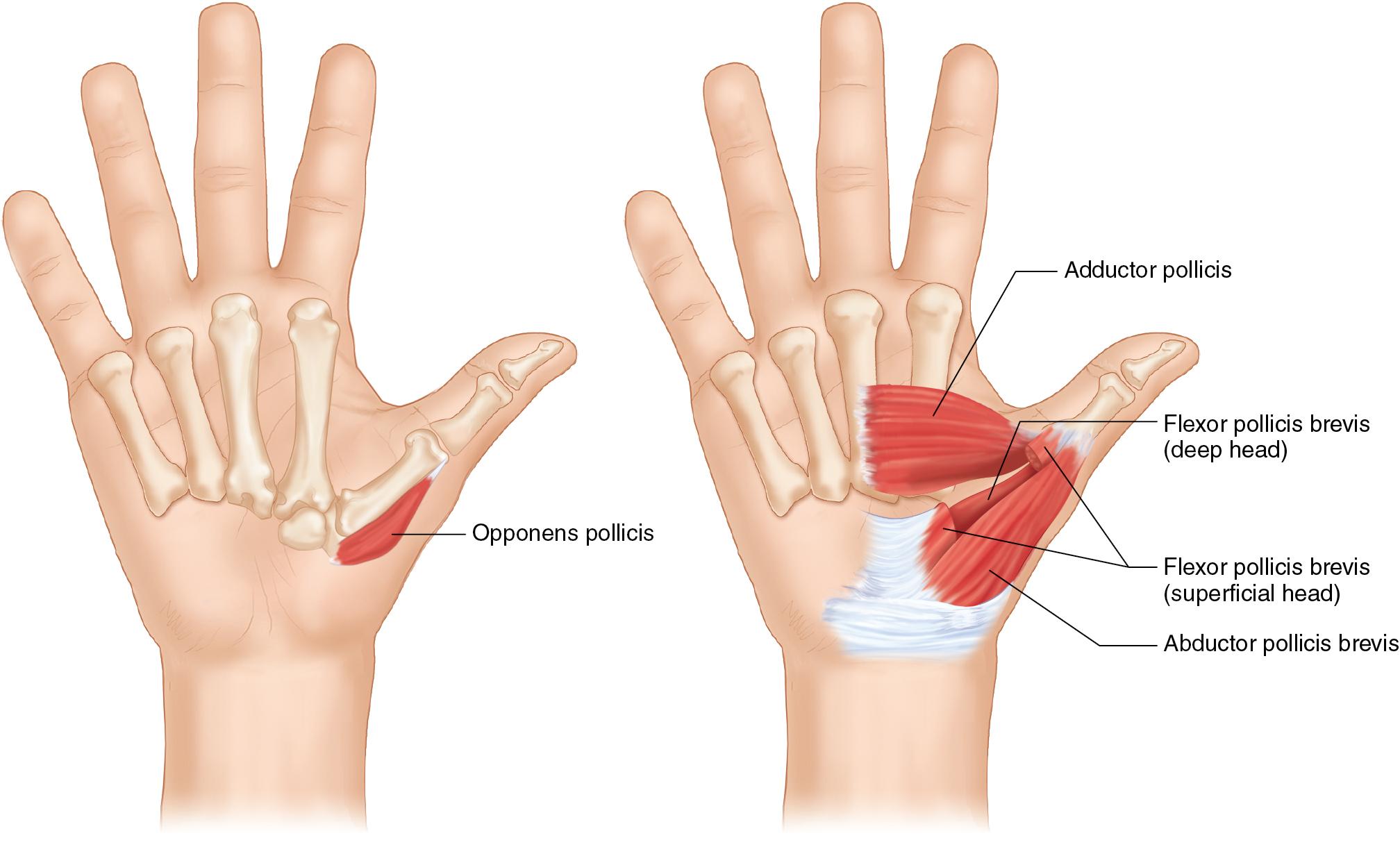
Median nerve injuries are classified as “low” injuries if they arise distal to the branch of the anterior interosseous nerve, causing functional loss that is limited to the intrinsic muscles of the hand: the abductor pollicis brevis (APB), the opponens pollicis, and the superficial head of the flexor pollicis brevis (FPB).
Both tendon transfers and nerve transfer options exist for patients with low median nerve injuries. Although tendon transfers lead to more predictable outcomes and earlier recovery, nerve transfers provide better fine motor control and require less retraining.
Tendon transfer is indicated for patients with low median nerve injuries when motor recovery is not expected. This typically includes three groups of patients:
Patients who experienced injuries more than 18 to 24 months prior and can no longer experience reinnervation given the onset of irreversible muscle fibrosis.
Patients with segmental nerve injury, who likely have inaccurate topographic alignment of the thenar motor fascicles. These patients can either wait to see if nerve regeneration is successful or can have a primary opponensplasty to provide a more predictable result with an earlier time to recovery of function.
Patients who prefer not to wait for nerve regeneration.
Several options for opponensplasty exist:
The Camitz transfer procedure is indicated for patients who require carpal tunnel release (CTR) for severe carpal tunnel syndrome with thenar atrophy because the palmaris longus (PL) can be transferred through the CTR incision to augment thumb opposition. The transfer can be performed with or without a pulley, which is typically created through a small window created in the flexor retinaculum. The pronation and flexion components of opposition are not reconstructed during this procedure.
The extensor indicis proprius (EIP) tendon may be used for opponensplasty for patients with either high or low median nerve injuries, and it is advantageous given the length and location of the EIP tendon. In these procedures, supplemental tendon grafts or additional pulleys to augment the line of pull are rarely necessary, and there is minimal donor morbidity. The pulley for this transfer is located at the ulnar border of the wrist.
During a Bunnell transfer, the flexor digitorum superficialis (FDS) tendon of the ring finger can be used to provide palmar abduction. Because the motor branch of the FDS muscle arises from the proximal aspect of the median nerve, this procedure is indicated only for patients with low median nerve palsy. Additionally, this technique requires the construction of a pulley along the ulnar aspect of the hand, typically the flexor carpi ulnaris (FCU) tendon. Harvesting the ring finger FDS tendon may result in weakened grip.
In a Huber transfer, transfer of the abductor digiti minimi (ADM) is commonly used to restore opposition among pediatric patients with congenital absence of thenar musculature (See Chapter 109 Pediatric Opponensplasty). This procedure can also improve appearance by increasing the bulk of the thenar eminence. Patients can adapt to use the transferred tendon without intensive rehabilitation. For pediatric patients, EIP tendon transfer is also indicated. The ADM origin acts as the “pulley” for this transfer.
Successful recovery from tendon transfer procedures demands that patients can comply with postoperative rehabilitation protocols and have supple joints with full passive range of motion (ROM), intact protective sensation, and no soft tissue scarring.
For many patients with low median nerve injuries, thumb opposition and palmar abduction are strong because of dual innervation by the ulnar nerve.
Difficulty with thumb opposition and palmar abduction may result from other causes, including sensory impairment and joint stiffness caused by diabetic neuropathy, severe carpometacarpal (CMC) osteoarthritis of the thumb, or rheumatoid arthritis.
Passive ROM should be tested at the thumb CMC, interphalangeal (IP), and metacarpophalangeal (MCP) joints.
Tendon transfers to restore opposition should be avoided in the setting of a first webspace contracture, which should be released before transfer.
Sensation in the hand should be assessed using the Semmes-Weinstein monofilament test (threshold test) and two-point discrimination (innervation-density test), with a specific focus on the sensation along the ulnar pulp of the thumb and the radial pulp of the index finger.
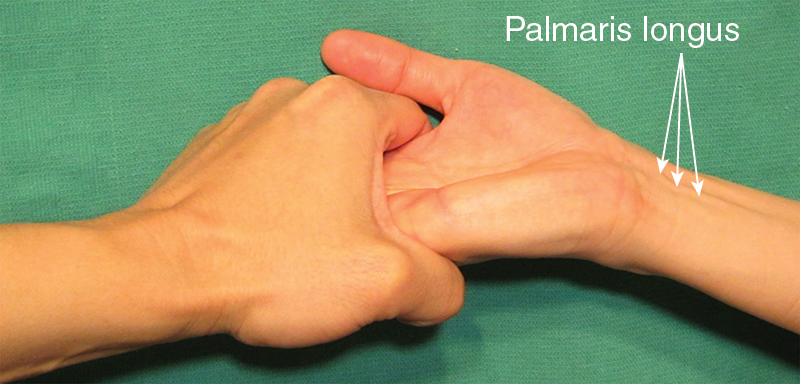
For patients who are potential candidates for a Camitz procedure, assess the presence of the PL. The Mishra test consists of passive hyperextension of the MCP joints followed by resisted active flexion at the wrist. This test can be performed for low median nerve palsy patients who cannot oppose their thumb ( Fig. 63.1 ).
A radiograph is useful to check the existence of other skeletal disorders such as CMC or MCP joint arthritis. Patients with thumb CMC arthritis often present with a supination and adduction deformity of the thumb, which may be corrected by trapeziectomy in conjunction with tendon transfer.
Thumb opposition is derived from thumb flexion, palmar abduction, and pronation at both the MCP and CMC joints. For patients with low median nerve palsy, the APB, opponens pollicis, superficial head of the FPB, and radial two lumbricals are denervated, but the deep head of the FPB and the adductor pollicis are innervated by the ulnar nerve, and this may provide sufficient palmar abduction and opposition for many patients ( Fig. 63.2 ).
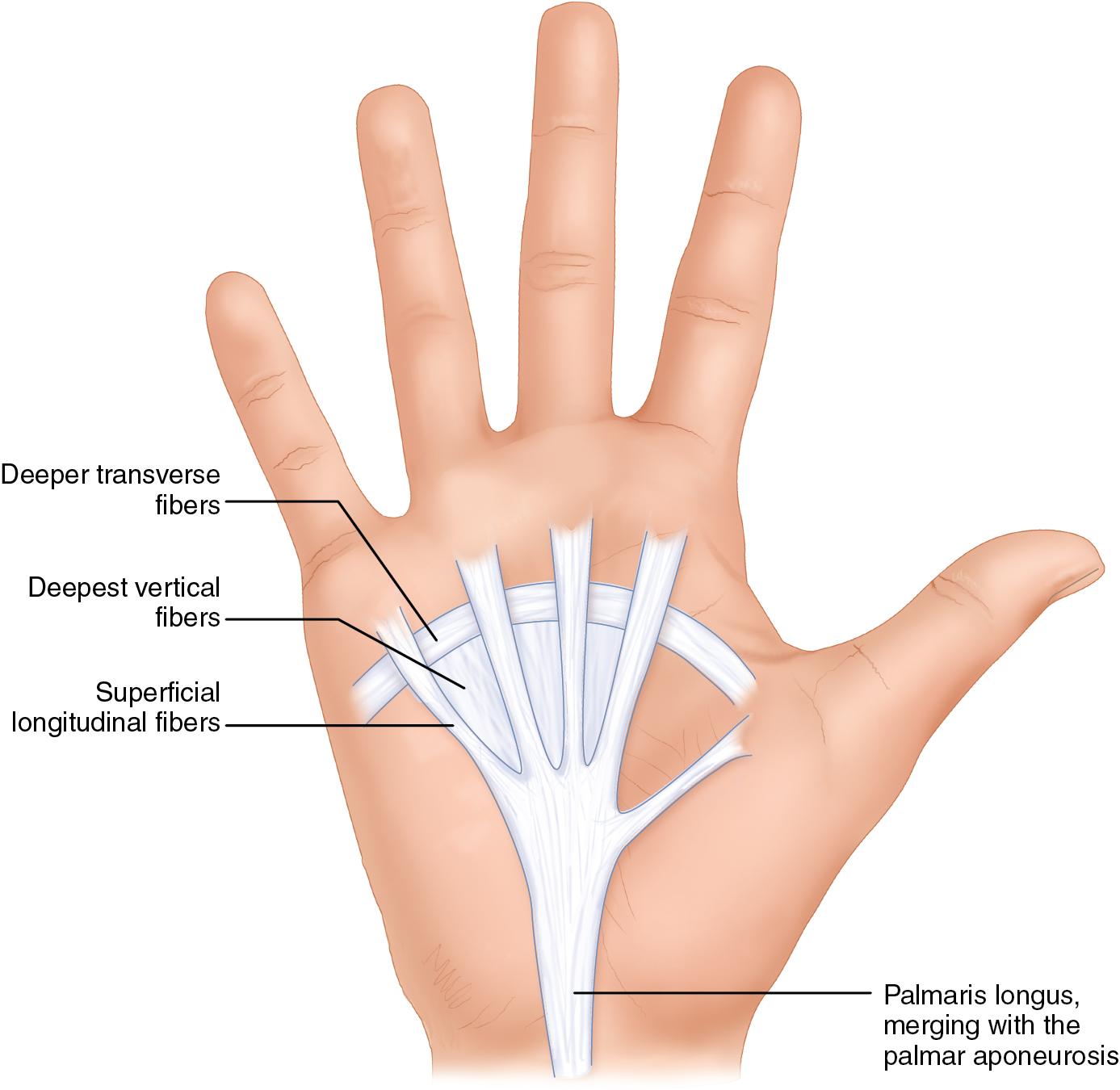
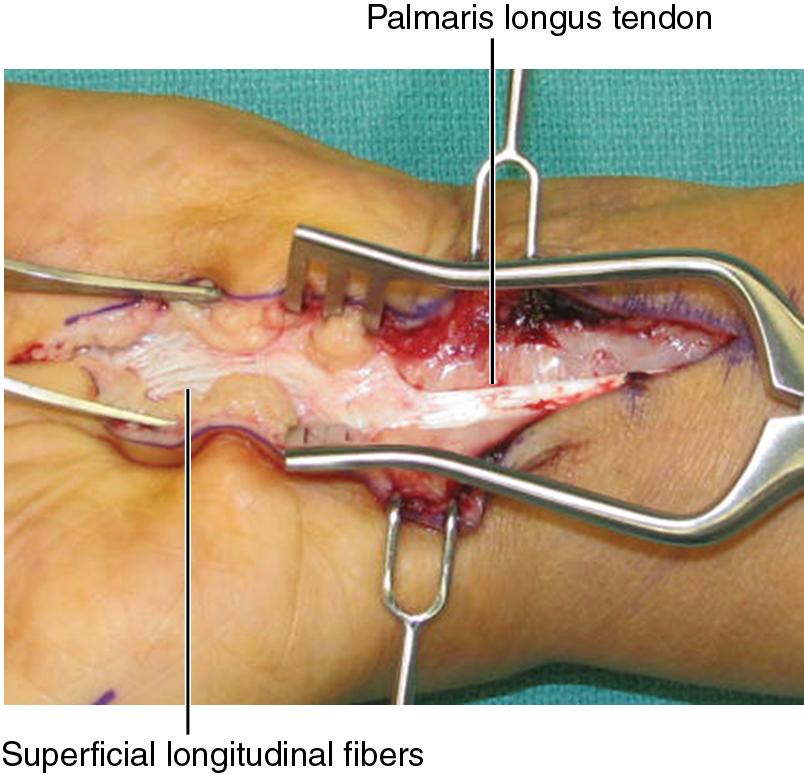
The palmar aponeurosis consists of three layers: superficial longitudinal fibers, deeper transverse fibers, and the deepest vertical fibers in the palm. For patients undergoing a Camitz transfer procedure, only the superficial longitudinal fibers are used to extend the length of the PL tendon for transfer ( Fig. 63.3 ).
Opponensplasty is performed under tourniquet control with the patient in the supine position and the extremity abducted with the hand on a hand table. It can be done under regional anesthesia, IV regional (Bier block) anesthesia, or local anesthesia.
This transfer can be performed in conjunction with carpal tunnel release (see Chapter 55 ) for patients with advanced median nerve compression at the wrist and weakened palmar abduction that is functionally limiting.
An extended carpal tunnel incision is marked: a 7-cm longitudinal straight skin incision is created over the palm along the axis of the ulnar border of the long finger. The incision is extended proximally with Bruner extensions at the wrist crease into the forearm ( Fig. 63.4 )
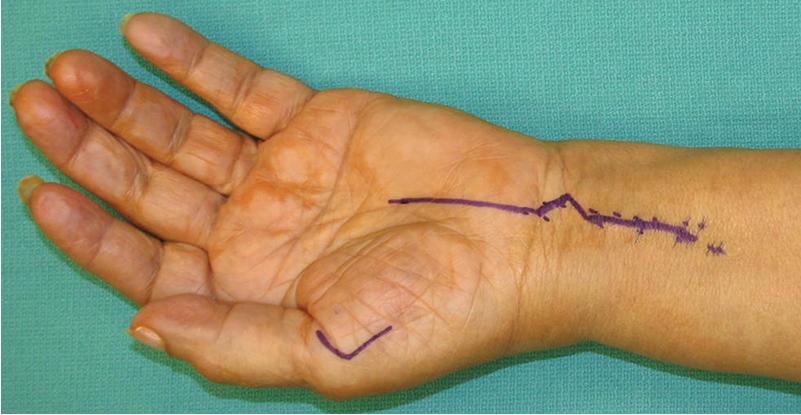
A 3-cm V-shaped incision is created along the radial border of thumb at the level of the MCP joint to expose the APB tendon (see Fig. 63.4 ).
To avoid scar contracture, the incision should not be made perpendicular to the wrist crease; use a Bruner orientation instead.
This skin incision over the palm and PL is created first.
The goal is to harvest both PL and an extension of palmar aponeurosis, with which PL is contiguous (see Fig. 63.3 ), to provide a longer donor tendon for transfer. Therefore wide exposure is provided by raising skin flaps radially and ulnarly to create an approximately 2-cm wide exposure of the palmar fascia.
The palmar aponeurosis is exposed distally to roughly where the transverse carpal ligament would be. Proximally, the palmar aponeurosis is exposed to where it merges with the PL insertion ( Fig. 63.5 ).
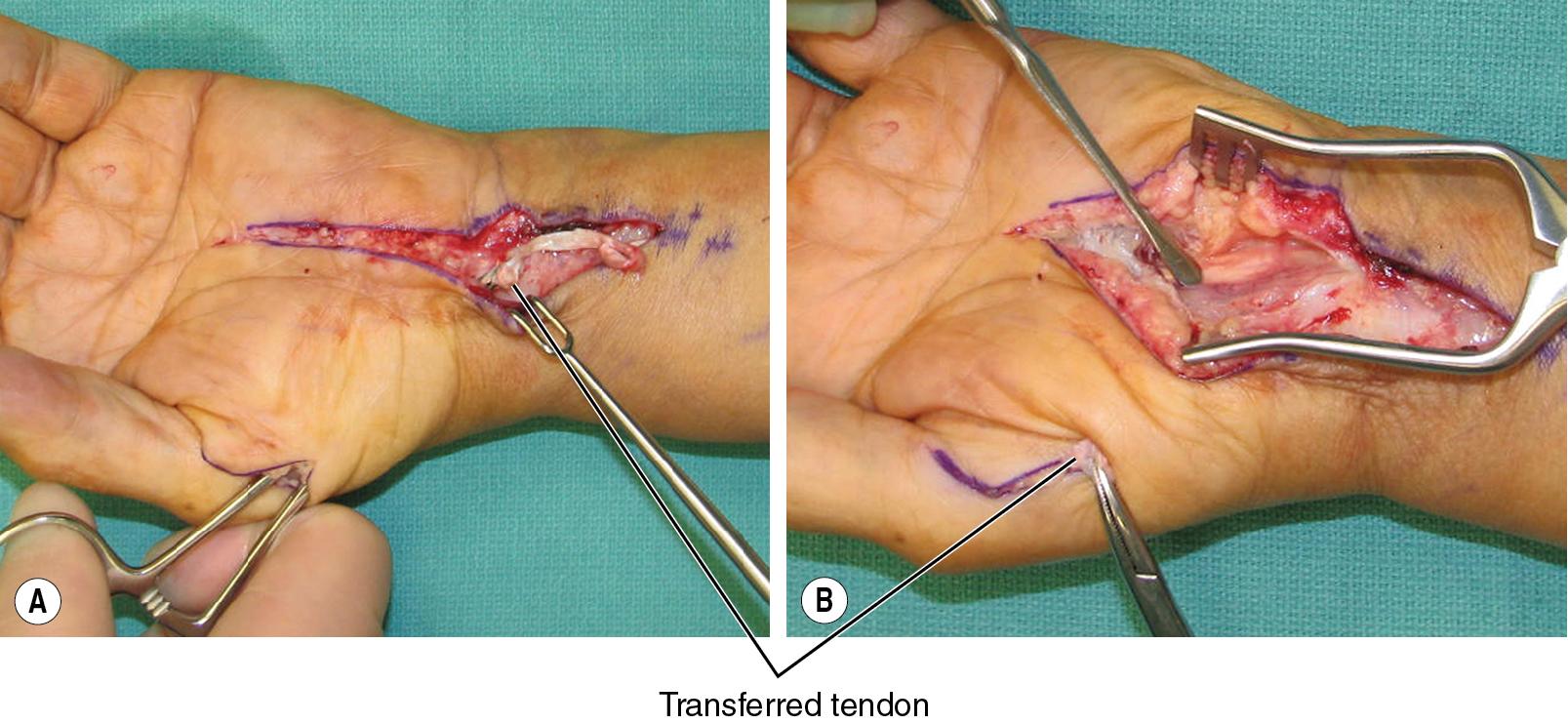
Once the donor tendon and palmar aponeurosis extension is exposed, the distal palmar fascia is dissected sharply free from the underlying transverse carpal ligament. Dissection is continued proximally until the PL tendon is dissected free. Dissection is continued distally until the tendon will reach the APB insertion ( Fig. 63.6 ).

A surgical sponge can again be used to estimate the length of the PL tendon needed for transfer that will reach the radial aspect of the thumb MCP joint.
A longer extension of palmar aponeurosis can be harvested, and the deep extension of dissection will be the palmar fat pad. Great care is taken during the distal dissection to protect the underlying superficial arch and common digital nerves. Once the TCL is visualized, dissection can proceed more expeditiously in the proximal direction.
Recognize that the PL harvest is quite proximal to the palmar cutaneous branch of the median nerve. This nerve arises in the forearm between PL and FCR and typically pierces the deep fascia to become a subcutaneous structure roughly 1 cm proximal to the wrist crease; however this is variable, so the surgeon needs to be looking for this branch when harvesting the PL tendon.
A standard carpal tunnel release is performed at this stage (see Chapter 55 ).
The incision along the radial border of the thumb MCP is created, and blunt dissection using tenotomy scissors is used to expose the APB tendon inserting onto the radial base of the thumb proximal phalanx.
The APB tendon is identified and exposed circumferentially with a small hemostat to facilitate the tendon weave.
The APB tendon is located just under the skin and attaches to the radial side of the base of the proximal phalanx of the thumb.
The APB tendon is quite small but stout; it only needs to be dissected circumferentially with a blunt hemostat for a few millimeters to facilitate the transfer.
Using a small hemostat, a subcutaneous tunnel is gently created along the thenar eminence from the MCP joint incision into the palmar incision.
A tendon passer is inserted through the subcutaneous tunnel from the incision along the MCP joint into the palm. The PL tendon and fascial extension are gently withdrawn through the tunnel into the incision along the radial aspect of the thumb ( Fig. 63.7 ).
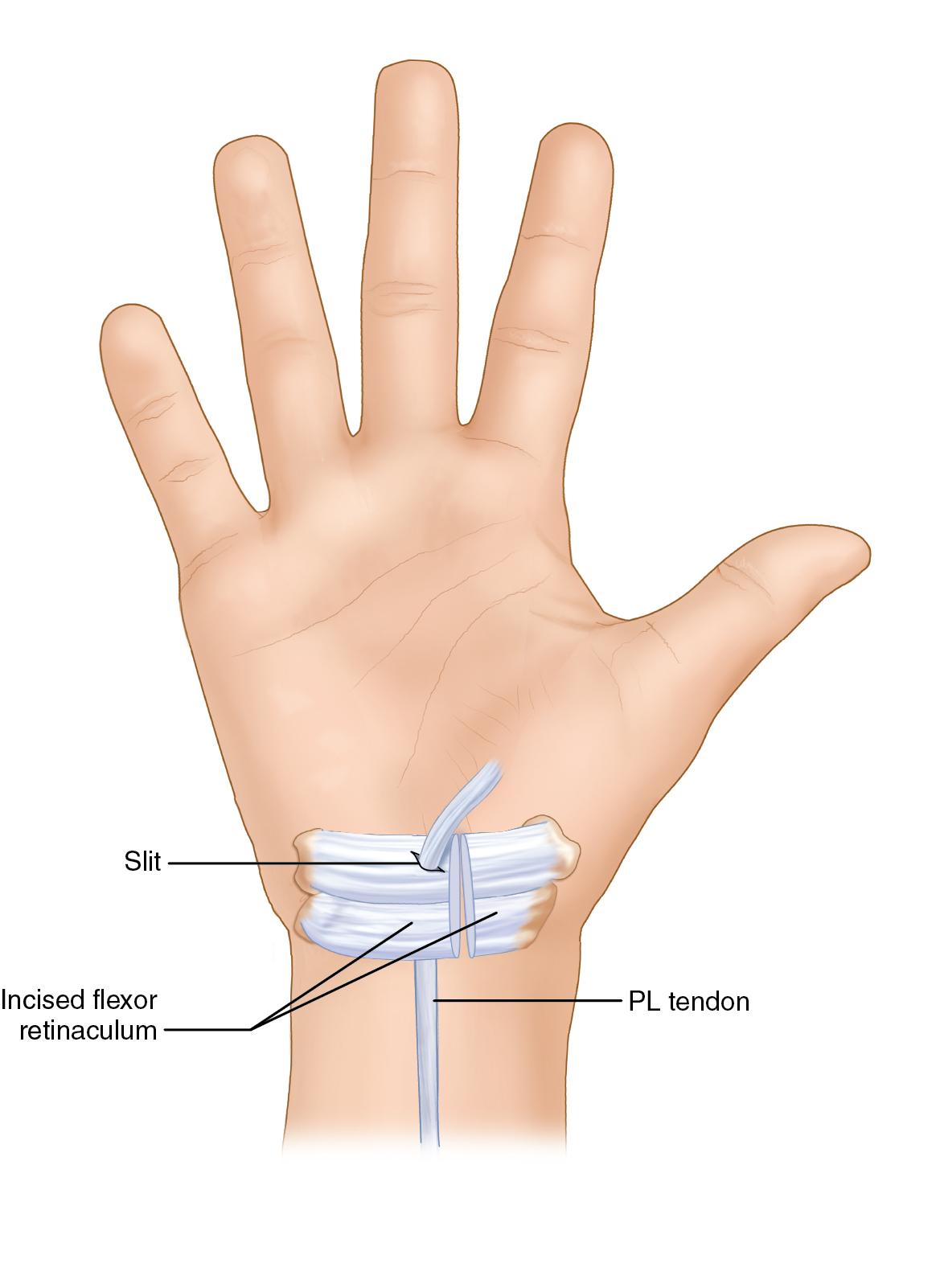
The original Camitz tendon transfer has been modified to include a pulley, which is typically made by passing the PL through a small window created in the ulnar side of the transverse carpal ligament ( Fig. 63.8 ).
The thumb is held in palmar abduction by an assistant.
The PL tendon is woven into the APB tendon using a sharp Pulvertaft tendon weaver and secured using 3-0 Ethibond suture.
Additional tendon weaves are performed as permitted and secured with 3-0 Ethibond sutures ( Fig. 63.9 ).
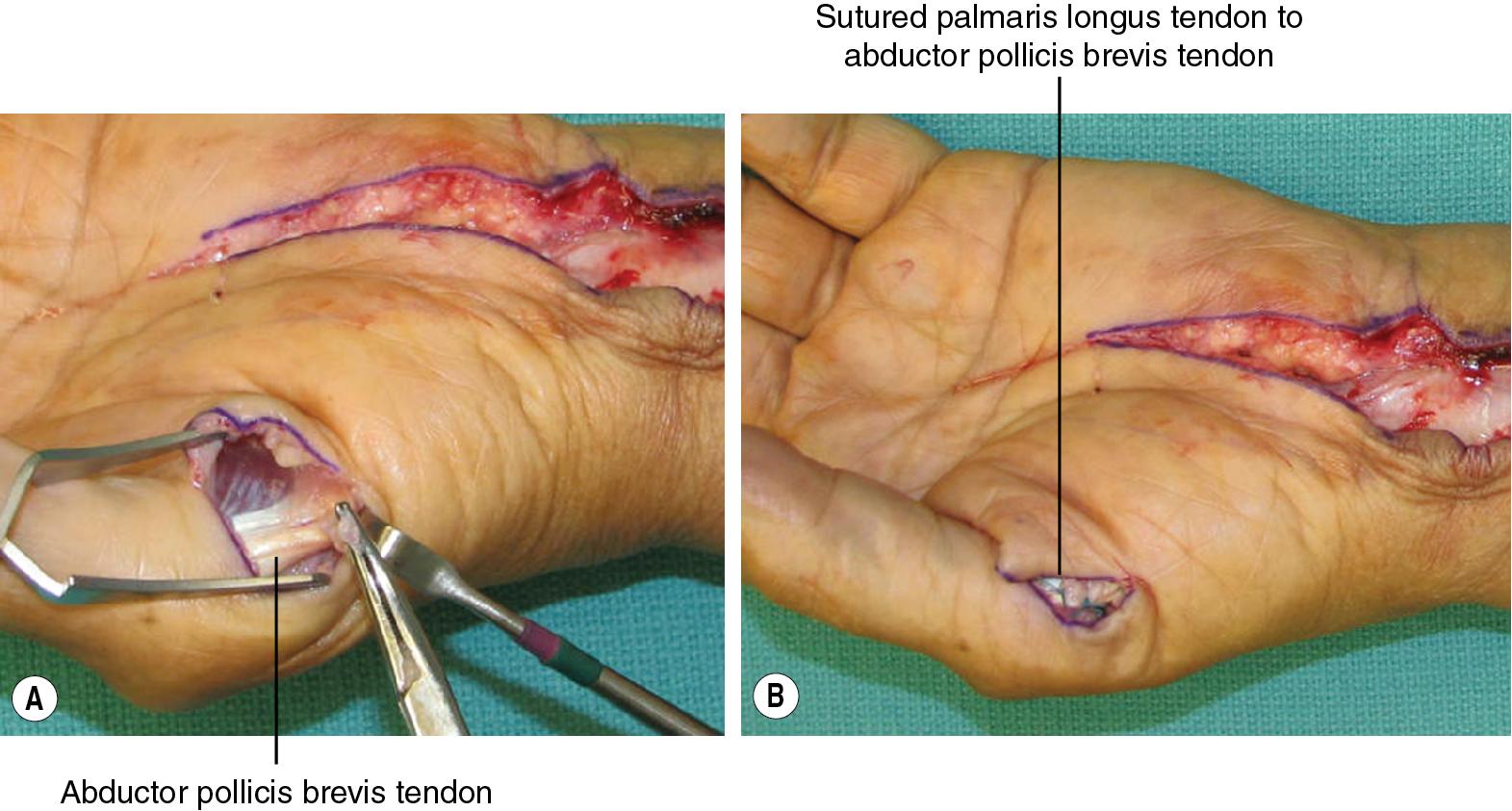
Subtle differences in postoperative thumb function depend on precisely where the PL is transferred: a more radial insertion adds stronger palmar abduction, and a more dorsal insertion adds greater opposition. It is difficult to split the tendon to insert at both ends because this may risk weakening the tendon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here