Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Several options exist for the management of proximal humerus fractures including nonoperative care, closed reduction and percutaneous pinning, open reduction and internal fixation (ORIF) with a plate and screw construct, intramedullary nailing, and arthroplasty. The majority of these injuries are nondisplaced or minimally displaced and may be managed nonoperatively with positive functional outcomes. , However, a subset of patients presenting with displaced proximal humerus fractures are deemed surgical candidates based on a myriad of considerations including both fracture characteristics and patient-related factors (see Chapter 25 : Treatment Algorithm for Proximal Humerus Fractures). Fracture characteristics that should be taken into consideration include the degree of displacement, fracture complexity, bone quality, size of the humeral head fragment, history of rotator cuff deficiency or rotator cuff arthropathy, presence of fracture-dislocations, chondral damage/head-split, and risk for future avascular necrosis.
The Neer classification is the most widely used classification system for proximal humerus fractures. Fractures are described based on the number of displaced fragments (one-, two-, three-, or four-part), which include the humeral shaft, greater tuberosity, lesser tuberosity, and articular segment. Fragments displaced >1 cm or angulated >45 degrees are considered truly “displaced” segments based on the classification scheme. Despite the fairly low intraobserver reliability and reproducibility, we find it a helpful tool to communicate a general idea of fracture morphology. ,
Patient characteristics such as physiologic age, past medical history, preinjury level of activity, functional demands, occupation, handedness, home living condition and support system, and ability to participate in and comply with a structured physical therapy program should all be considered in deciding management.
Appropriate patient selection criteria for surgical management have been a topic of much debate, and a consensus on optimal management remains poorly defined. Results from the Proximal Fracture of the Humerus Evaluation by Randomization (PROFHER) trial, which suggested that operative intervention provides no benefit over nonoperative treatment, further clouds decisional management of these injuries. The validity of this study’s results has been questioned due to a number of methodologic limitations and poorly defined surgical indications.
Generally, we prefer management with ORIF for substantially displaced proximal humerus fractures in active, healthy, physiologically “young” patients, with adequate bone stock and no contraindications to surgery. This includes significantly displaced two-part tuberosity and surgical neck fractures as well as most three-part fractures, four-part fractures, and fracture-dislocations, where adequate reduction and stability can be achieved and healing potential remains adequate. Patients presenting with unreconstructable humeral heads, unacceptably high risk of osteonecrosis (i.e., delayed presentation of head-split or fracture-dislocations), rotator cuff deficiency, or significant glenoid arthrosis may be better suited with primary arthroplasty.
On the other side of the spectrum, patients may be better suited for nonoperative management or primary versus delayed arthroplasty if they are physiologically “elderly,” low-demand, have low potential to heal tuberosity fragments, have poor bone quality, or suffer from comorbidities such as diabetes, vascular disease, metabolic disorders, or poor nutritional status that risk bone failure around the fixation construct and screw cutout. Recent literature suggests inferior outcomes in elderly patients who undergo revision arthroplasty following failed ORIF attempts when compared with delayed arthroplasty following failed nonoperative attempts. This highlights the concept that ORIF should be performed in a select patient population on an individualized basis where a multitude of factors are taken into consideration and a patient-involved decision is reached.
Pertinent information to be obtained from a patient’s history include the mechanism of injury, antecedent pain, history of malignancy, and history of previous injuries and/or surgeries to the operative extremity. A low-energy mechanism such as a ground-level fall or history of other fragility fractures should clue the clinician into the patient’s overall poor bone quality. This can present as an opportunity for the orthopedic surgeon to diagnose and guide treatment for low bone density disorders in order to prevent future fragility fractures. ,
In the setting of high-energy injuries, physical examination should begin with the advanced trauma life support protocol. All other extremities should be evaluated, including the spine and chest wall, with a combination of palpation and range of motion to screen for concomitant injuries prior to performing a focused examination of the suspected injured extremity. Focused physical examination begins with evaluation of the soft tissues and skin surrounding the shoulder and axilla to rule out the presence of an open fracture. A careful neurovascular examination should be performed with particular attention to the motor and sensory function of the axillary nerve. Evaluation of the axillary nerve is performed by assessing independent muscle contraction of the posterior, lateral, and anterior divisions of the deltoid muscle and proximal lateral arm sensation.
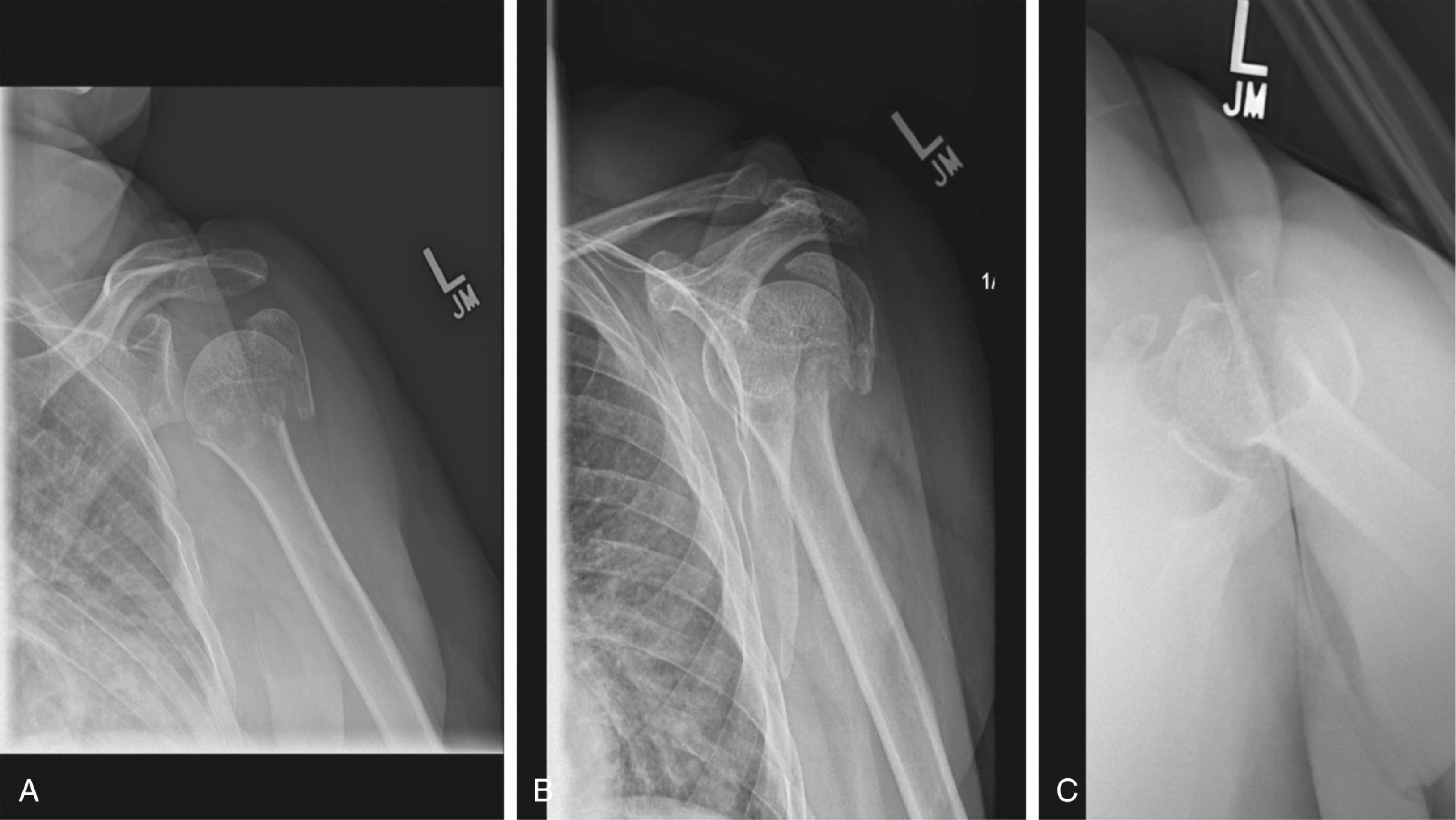
A complete radiographic shoulder series should be obtained, including a true glenoid anteroposterior (AP) or Grashey view, axillary lateral view, and scapula Y lateral view ( Fig. 27.1A–C ). The axillary lateral view defines the humeral head-glenoid relationship and is imperative in evaluating for glenohumeral dislocation or glenoid articular surface involvement. Lesser tuberosity displacement can also be further evaluated with this view. Alternatively, if the patient is unable to tolerate positioning for an axillary lateral, a Velpeau view can be obtained. The scapula Y view provides information on the head-shaft angulation and displacement in the sagittal plane, whereas the Grashey AP view provides information on coronal (varus/valgus) fracture alignment and tuberosity displacement. Computed tomography (CT) imaging with or without three-dimensional (3D) reconstructions is not always indicated for proximal humerus fractures; however, it can provide more detailed information regarding tuberosity displacement, nondisplaced fracture lines, degree of comminution, articular surface involvement, and definitive glenohumeral relationship especially when an axillary lateral radiograph is of poor quality or unable to be obtained. Generally, the authors obtain a CT scan in settings where the degree of tuberosity displacement is not well visualized on standard radiographs, axillary lateral views cannot be obtained to evaluate for fracture-dislocations, and if the fracture pattern is poorly visualized on radiographs in operative fractures for the purpose of surgical planning.
The procedure is typically performed under general endotracheal anesthesia to allow for adequate muscle relaxation to aid in reduction. Regional anesthesia such as an interscalene block may be performed for postoperative pain control. The patient is positioned supine with his or her head on the cantilever end of a radiolucent table. Following intubation, the table is rotated 90 degrees with the operative shoulder facing the center of the operating room. A plexiglass, radiolucent board is placed under the pad of the table such that an approximately one-foot by one-foot area beyond the edge of the table can support the patient’s upper arm. The patient’s torso is positioned so the operative shoulder is over the lateral edge of the bed to maximize access to the proximal humerus and to allow for an adequate axillary fluoroscopic view. At this point, AP and axillary fluoroscopic views with the C-arm positioned at the head of the OR table may be obtained to ensure that adequate orthogonal fluoroscopic images are accessible. An AP view of the humerus will be used to determine coronal plane alignment, cranial-caudal plate position, and screw lengths. The arm should be externally rotated 20 to 30 degrees to view the humeral head and neck in profile while accounting for native retroversion. An axillary view is performed with the beam parallel to the floor and the patient with the arm in 30 to 90 degrees of abduction ( Fig. 27.2A–B ). This view will be used to assess sagittal plane deformity, version, reduction of the glenohumeral joint and tuberosities, anterior-posterior placement of the plate, and screw lengths and trajectories.

Foam pads or towels are placed on the arm board to match the height of the table’s padding ( Fig. 27.2A ). Foam padding is placed under the heels and blankets are placed under the patient’s knees to provide hip and knee flexion ( Fig. 27.3 ). All other bony prominences are well padded. The patient’s head may be secured with tape and a towel placed over the forehead or a foam head holder. A U-shaped drape is placed within the axilla from the scapula posteriorly ending just above the nipple line medially. A straight drape is placed along the neck and mid-clavicular line.

The prep and drape is finalized with sterile towels and two U-shaped drapes with the aperture secured with strips of Ioban (3M; Saint Paul, MN, USA). A stockinette and Coban (3M) are placed over the ipsilateral upper extremity ending just distal to the supracondylar region of the humerus. A sterile drape to allow passage of the C-arm is placed distal to the operative extremity. The Mayo stand and back table are located lateral to the operative extremity ( Fig. 27.4A–B ). A summary of procedural equipment is presented in Table 27.1 .

| Positioning |
|
| Exposure Biceps tenodesis |
|
| Reduction |
|
| Fixation |
|
| Imaging |
|
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here