Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The talus’s multiple articulations facilitate complex motion of the ankle and hindfoot critical to the biomechanics of gait, earning its title “the universal joint of the foot.” While fractures of the talus are uncommon, accounting for approximately 1% of all fractures, they are frequently the result of high-energy trauma, such as motor vehicle collisions and falls from height, and frequently lead to considerable morbidity. Injuries to the talus are serious because this bone is the critical link between the subtalar, transverse tarsal, and ankle joint complex. The variety of coupled actions occurring from the motion of this bone or surrounding bones permit the effortless flexibility of the hindfoot and midfoot. If the talus is damaged, the universal combined motion of the foot and ankle becomes compromised, and severe disability can result.
The terms talus and astragalus date back to the pre-Christian era. The modern word talus comes from the Old French talo , meaning ankle, and originates in the Latin word for dice, or taxillus , because the Romans made their dice from the heel bone of a horse. The Greeks, on the other hand, made their dice from the second cervical vertebra of the sheep. The word for this vertebra in Greek is astragalus .
Early accounts of talar fractures, dating over 400 years ago, revealed a high rate of morbidity and mortality. Coltart credits Fabricius Hildanus with the first account of an injury to the talus in 1608, a complete dislocation treated with talectomy. Astley Cooper first described the natural history of dislocation of the talus in 1818. In 1848, James Syme reported that of 13 patients admitted to the Royal Infirmary of Edinburgh with compound fracture-dislocation of the talus, only two survived. Therefore, he recommended below-knee amputation for these injuries, a procedure that still produced a mortality rate of 25% in his era. In 1909, Stealy confirmed a 50% mortality rate after open fracture-dislocation of the talus based on a review of available reports.
With the advent of aviation, a new mechanism of injury arose. Anderson, while serving as consultant surgeon to the Royal Flying Corps in 1919, reported on 18 cases of fracture-dislocation of the talus. Because parachutes were not in use at this time, pilots went down with their aircraft, resulting in a hyperdorsiflexion force exerted on the sole of the foot by the rudder bar of the aircraft on impact. He coined the term “aviator's astragalus” for this injury. In 1952, Coltart described 228 injuries of the talus that he collected from the Royal Air Force records during the World War II, including 106 fractures or fracture-dislocations of the talar neck, to date the largest series ever reported.
Further study has led to classification of these injuries. In 1970, Hawkins classified vertical fractures of the talar neck into three groups based on the roentgenographic appearance of the fracture at the time of injury. The significance of this classification was its prognostic value with respect to avascular necrosis (AVN). Since that time, a plethora of publications have documented a variety of problems associated with vertical fractures of the talar neck, including AVN, nonunion, malunion, infection, arthritis, and bone loss.
The talus is the second largest tarsal bone. It sits between the distal tibia and fibula above and the remainder of the foot below. Two thirds of the talar surface is articular, and its five articular surfaces all have a weight-bearing function ( Fig. 46-1 ). Perhaps due to the extent of articular cartilage coverage, it is devoid of tendons and muscles attachments.
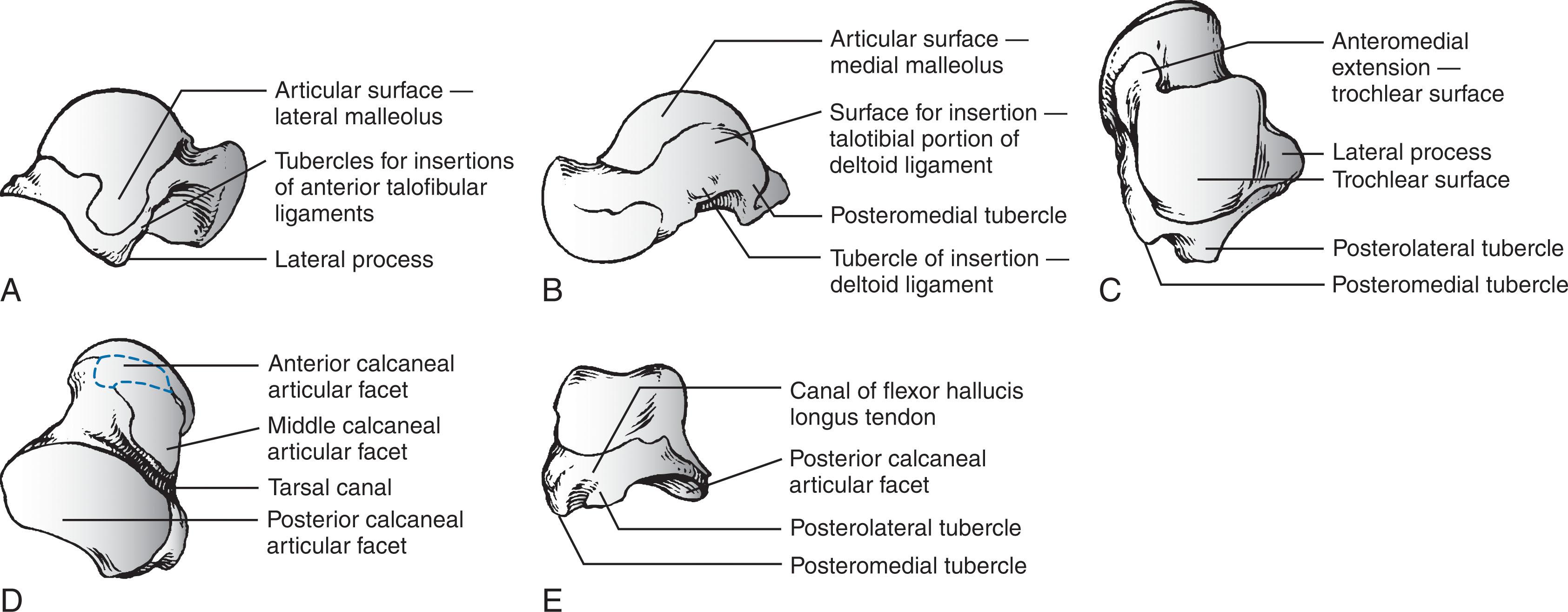
The talus is composed of three parts—the head, neck, and body—and two processes—the lateral and posterior. The head is the portion that articulates mostly with the navicular. The body includes the dome of the talus at the ankle joint and the posterior facet at the subtalar joint. Between the head and the body is the neck , which does not articulate with the ankle and sits over the sinus tarsi. The body and neck of the talus are not coaxial because, in the horizontal plane, the neck angles medially with a variable angle of declination.
The body of the talus is divided into five surfaces: lateral, medial, superior, inferior, and posterior.
The lateral surface consists of a large articular surface, the facies malleolaris lateralis, which articulates with the distal fibula. Along the anterior, inferior, and posterior perimeter of this lateral articular surface is the lateral process , a nonarticular component of the talus, which is the origin of the anterior talofibular ligament, posterior talofibular ligament, and talocalcaneal ligament.
The medial surface of the body presents two areas: superior and inferior. The superior portion is occupied by the articular facet, or facies malleolaris medialis. The inferior portion is nonarticular, and its anterior half is a depressed surface perforated by numerous vascular foramina, while the posterior half of the inferior portion provides insertion for the deep component of the deltoid ligament.
The superior surface of the talar body is completely covered with articular cartilage and is shaped like a pulley, with the groove of the pulley (trochlea) closer to the medial border. The transverse diameter of the superior surface is greater anteriorly than posteriorly and resembles a keystone. This unique shape provides maximal articular congruence in the articular joint when the talus is in a dorsiflexed position ( Fig. 46-2 ).
The inferior surface of the talar body consists of the facies articularis calcanea posterior tali. This articular surface is quadrilateral and is concave in the long axis and flat transversely. It articulates with the posterior facet of the calcaneus (see Fig. 46-1D ).
The posterior surface of the talar body consists of posterolateral and posteromedial tubercles that flank the sulcus for the flexor hallucis longus tendon. The posterolateral tubercle is larger and more prominent than the posteromedial tubercle. The posterolateral tubercle contributes an inferior articular surface that is in continuity with the posterolateral aspect of the posterior calcaneal surface of the talus. The posterolateral tubercle may appear as an oversized trigonal process known as the Stieda process or as a separate accessory bone, the os trigonum, which is seen in approximately 3% to 8% of the population.
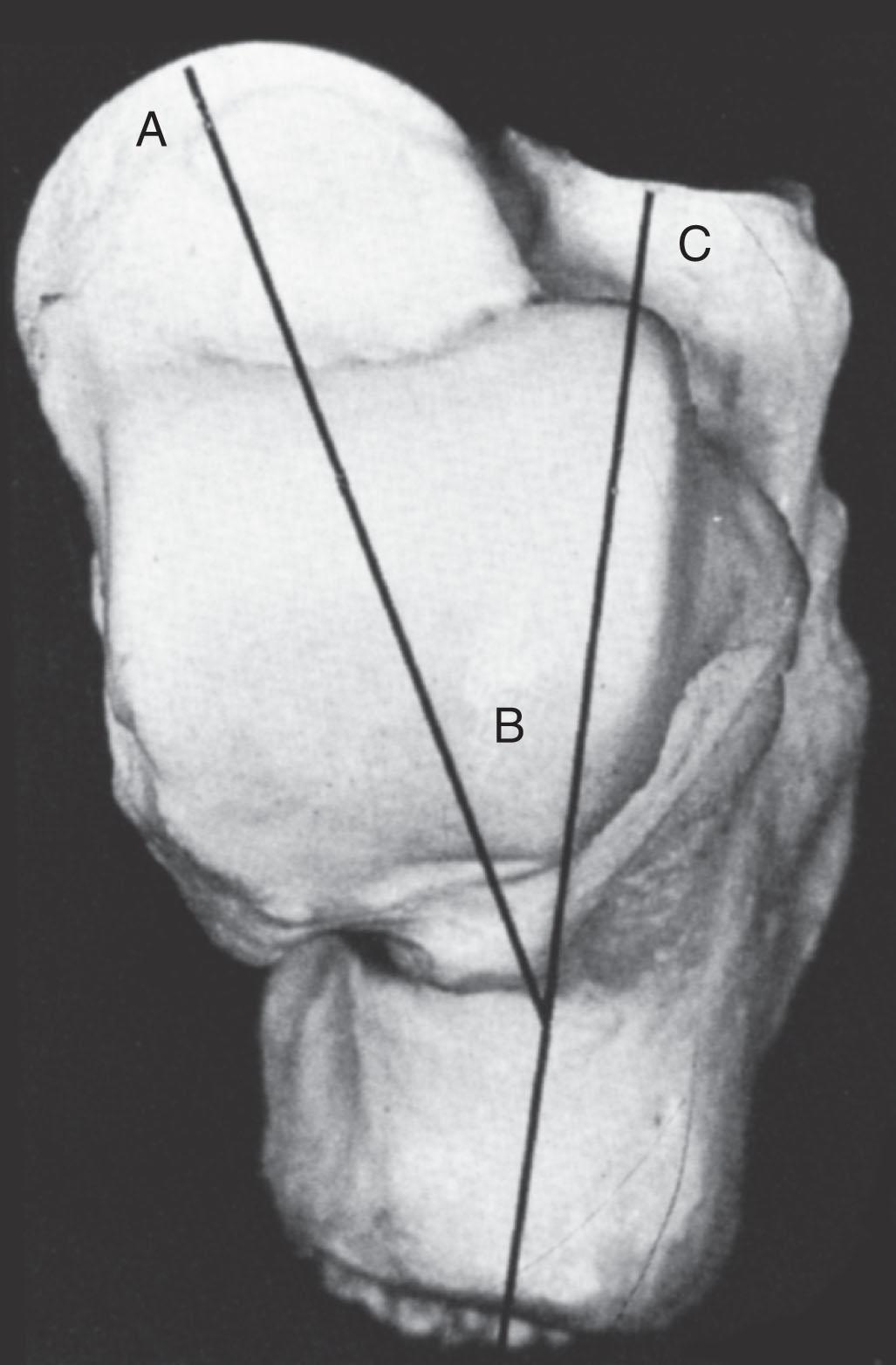
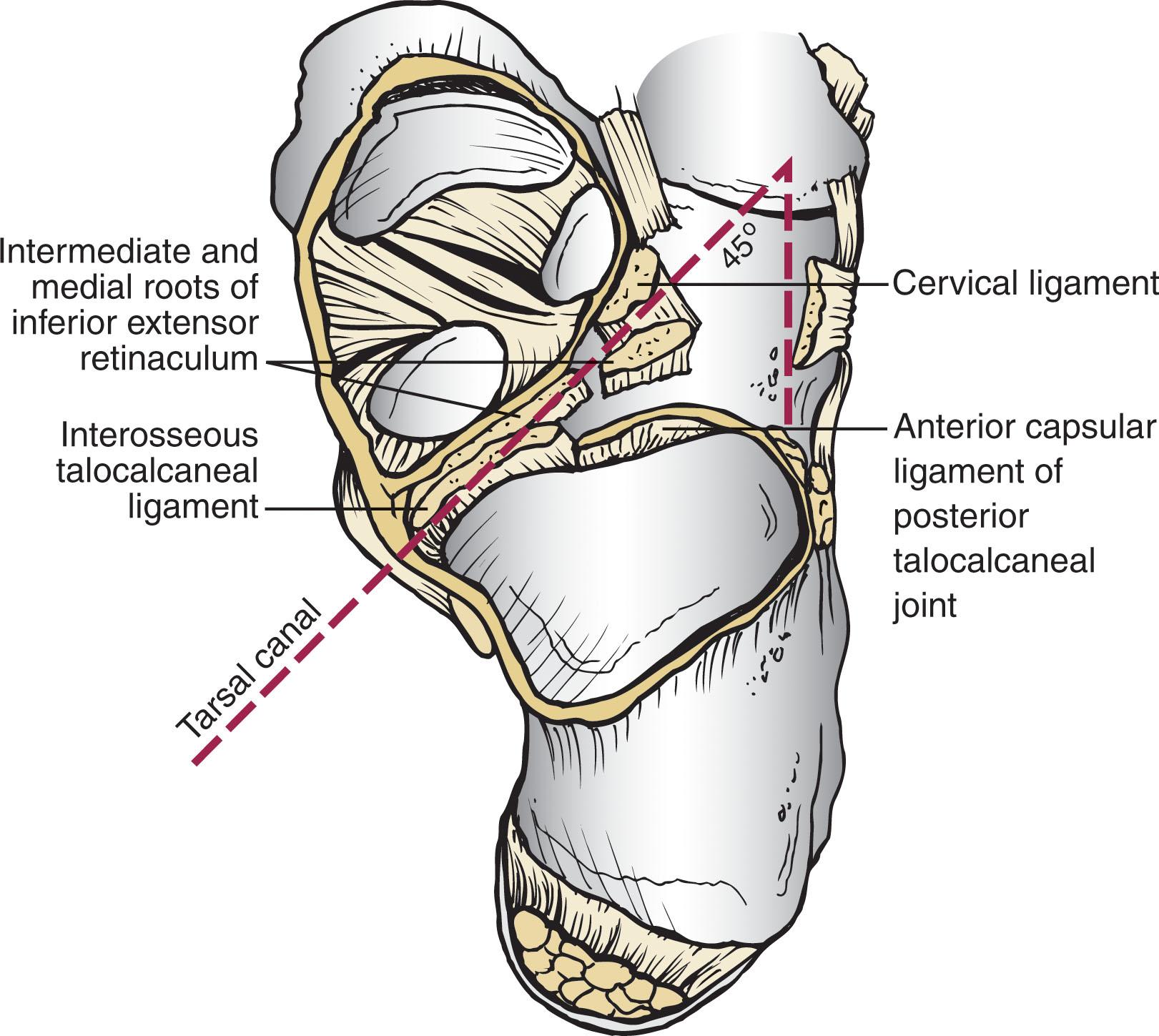
The neck of the talus is one of the few areas of the talus not covered by articular cartilage, allowing ligamentous attachment. It has four surfaces: superior, lateral, medial, and inferior. The superior surface of the neck is limited posteriorly by the anterior border of the trochlea of the talus (the dome or body) and anteriorly by the articular surface of the talar head. The ankle joint capsule inserts along this superior surface just proximal to the insertion of the capsule of the talonavicular joint. The lateral surface of the neck provides an insertion for the medial aspect of the inferior extensor retinaculum. The lateral cortex of the talar neck is concave and flares as it approaches the lateral cortex. The inferior surface of the neck forms the roof of the sinus tarsi and sinus canal and is the insertion point for the talocalcaneal ligament, a major stabilizer of the subtalar joint. The mildly convex medial surface provides an area for insertion of the talonavicular ligaments. The talar neck is angled at a mean of 24 degrees medially (range, 10–44 degrees) and plantarly (range, 5–50 degrees), and it is the portion of the talus most vulnerable to fracture ( Fig. 46-3 ).
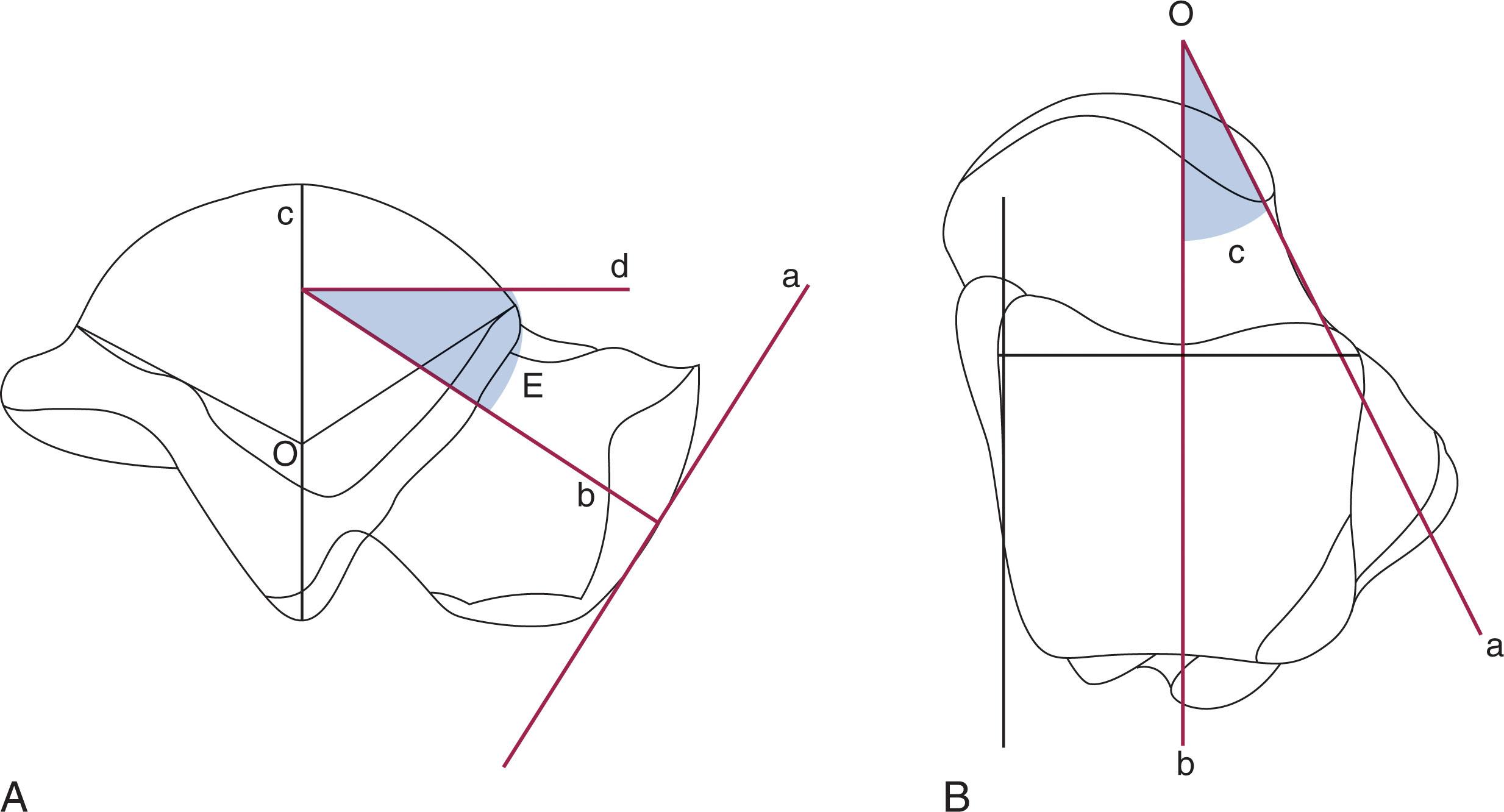
The head of the talus is the distal portion that nests within an articulation known as the acetabulum pedis , or foot socket, as described by Sarrafian ( Fig. 46-4 ). This socket is formed by the calcaneal middle and anterior facets and proximal navicular joint surface. It connects to the large navicular articular surface by the inferior and superomedial calcaneonavicular ligaments. It is hinged laterally by the lateral calcaneonavicular component of the bifurcate ligament and medially by the posterior tibial tendon and the spring ligament. The anteroinferior medial portion of the talar head is quadrilateral or oval and provides articulation with the anterior facet of the calcaneus. This portion of the head is flat and continuous anteriorly with the navicular articular surface. The acetabulum pedis has a variable volume capacity and adapts to the changing position of the talar head during gait.
The blood supply to the talus has been studied in detail because of the incidence of AVN after fractures and dislocations ( Fig. 46-5 ). Fractures or dislocations of the talus are often associated with disruptions in the blood supply and thus pose potential problems for the healing and integrity of the talus. Although early reports indicated poor vascular flow, more recent investigators note the presence of an extensive extraosseous and intraosseous blood supply to the talus. However, because most of the talar surface is covered with articular cartilage and no muscles originate or insert into this bone, the areas available for vessels to enter are few.
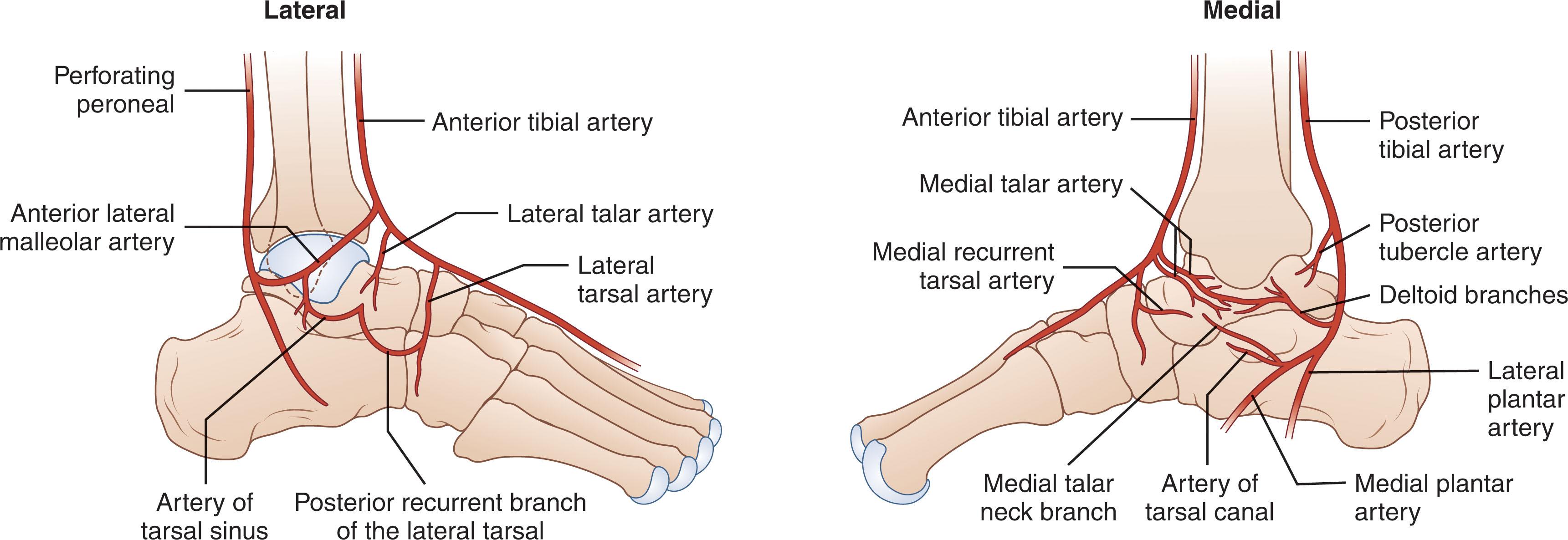
The extraosseous arteries to the talus include branches from the posterior tibial, dorsal pedis/anterior tibial artery, and peroneal arteries through a vascular network that covers all its cartilage-free surfaces. Miller et al studied the blood supply of the talus using gadolinium enhanced magnetic resonance imaging (MRI) and demonstrated that the greatest contribution of the blood supply (47%) comes from the posterior tibial artery, which is current consensus. However, all these vessels anastomose to form several vascular networks that surround and supply blood to the talus. Of the anastomosing vessels, the arteries of the tarsal sinus and tarsal canal, together with the medial periosteal network, are the most important sources of blood supply to the talus.
Medially, the posterior tibial artery gives rise to two main branches to the talus. The first, the artery of the tarsal canal , gives rise to a branch that supplies the medial surface of the talar body. This vessel, known as the deltoid branch , passes between the talotibial and talocalcaneal portions of the deltoid ligament and supplies the medial periosteal surface of the talar body. The second branch derived from the posterior tibial artery consists of a vascular plexus over the posterior medial tubercle of the talus. It is formed by calcaneal branches of the posterior tibial artery and an anastomosis with branches from the peroneal artery.
The anterior tibial, or dorsalis pedis, artery also provides blood to the talus from two groups of vessels. First, it sends branches to the superior surface of the talar neck. These branches arise either directly from the anterior tibial artery as medial tarsal branches or indirectly as branches of the anteromedial malleolar artery, providing important circulation to the talar head. Second, the anterior tibial artery gives rise to the anterolateral malleolar artery, which can anastomose with the perforating peroneal artery that becomes the artery of the tarsal sinus.
The peroneal artery also provides two sources of blood supply to the talus. First, small branches from the peroneal artery join with the calcaneal branches of the posterior tibial artery to form the vascular plexus over the posterior tubercle of the talus. Second, the perforating peroneal artery anastomoses with other vessels to form the artery of the tarsal sinus laterally.
The posterior tibial artery gives rise to the artery of the tarsal canal about 1 cm proximal to the origin of the medial and lateral plantar arteries. This artery of the tarsal canal passes anteriorly between the sheaths of the flexor digitorum longus and flexor hallucis longus muscles to enter the tarsal canal. Within the canal, the artery lies in the dorsal half of the canal, closer to the talus than the calcaneus. It anastomoses with the artery of the tarsal sinus to form what is called the artery of the tarsal sling; this artery is located beneath the talus and passes through the tunnel formed by the tarsal sinus and the tarsal canal. In this tunnel, it gives rise to branches that enter the inferior aspect of the talar neck.
Along with its anastomoses to the artery of the tarsal canal, the sinus tarsi artery is the principal supplier of the intra-sinus structures and of the talus. The sinus tarsi artery is formed from anastomoses among various arteries of the lateral region of the foot. These included the anterior lateral malleolar and proximal lateral tarsal arteries. In some specimens an additional branch is from the distal lateral tarsal artery or an additional anastomotic branch is from the peroneal artery.
The head of the talus has two sources of blood supply. Branches from the anterior tibial (dorsalis pedis) artery supply the superior medial half, and the inferior lateral half is supplied directly from the arteries of the tarsal sling. Inferiorly, the part of the talar neck that forms the anterior boundary of the tarsal sinus is the entryway for the intraosseous circulation to the talar head. According to Mulfinger and Trueta, this vascular pattern to the talar head is relatively constant. Peterson et al described a rich vascular connection between the head of the talus and the navicular arising from the many supporting ligaments and the talonavicular capsule.
The body of the talus is supplied by vessels that enter through five surfaces: the superior surface of the talar neck, the anterolateral surface of the talar body, the inferior surface of the talar neck (roof of the tarsal canal), the medial surface of the talar body (deltoid ligament), and the posterior tubercle. The main blood supply to the lateral two thirds of the talar body is from the artery of the tarsal canal, which provides four or five main branches into the body, and the medial one third of the body is supplied by the deltoid branch, which enters from the medial surface of the talus. The arteries that enter the superior aspect of the neck send one or two branches into the central anterosuperior aspect of the body. Finally, the posterior tubercle of the talus is supplied by small branches from the posterior anastomotic network formed by the peroneal artery and posterior branches from the posterior tibial artery. These posterior vessels also provide communication between the intraosseous blood supply of the tibia through the posterior capsule of the talotibial joint.
Anastomoses between the various intraosseous arteries of the talus are responsible for the survival of the talus in severe injuries. Mulfinger and Trueta noted vascular anastomoses within the talus in 60% of their specimens. Arteries entering the superior neck anastomosed with branches of the artery of the tarsal canal in 26% of cases, and anastomoses between the inferior and superior vessels of the talar head were noted in 13% of cases. Anastomoses between branches of the artery of the tarsal sinus and the artery of the tarsal canal occurred within the talus 13% of the time, and anastomoses between the posterior tubercle branches and branches arising from the artery of the tarsal canal occurred in 3% of specimens. Finally, the deltoid branches medially anastomosed with branches from the artery of the tarsal canal in 3% of patients.
These anastomoses may protect the talus when it sustains a major injury, and the lack of these connections in certain areas of the talus may also explain why AVN can affect portions of the talar body differentially. Peterson et al demonstrated that although nondisplaced fractures of the talar neck disrupted some of the intraosseous branches arising from the tarsal sinus and tarsal canal arteries, the major portion of the vascular supply of the talus remained intact through the deltoid ligament and major branches from the artery of the tarsal sling. With displaced fractures of the talar neck, however, the deltoid branches, the superior talar neck branches, and the artery of the tarsal sling could all be potentially disrupted, thereby increasing the incidence of AVN. When even one of these three major sources was spared injury, intraosseous anastomoses possibly permitted the talus to survive. These findings support the concept that degree of fracture displacement predicts risk of AVN due to increasing damage to a significant portion of the talar blood supply.
The variability of the anastomotic network and the susceptibility to injury also require careful fracture manipulation and minimal soft tissue stripping during surgery to prevent further insult to the blood supply. Preservation of the deltoid artery branches is extremely important and deserves care when performing a medial malleolar osteotomy because this may be the only remaining source of blood supply to the talar body in the case of a displaced talar neck fracture.
Fractures and fracture-dislocations of the talar neck account for 50% of all major injuries to the talus. Most talar neck fractures occur in young adults, and men outnumber women 3 to 1.
These injuries are significant because of the frequency and severity of associated complications and long-term disability. The principal problems associated with these fractures and fracture-dislocations include AVN, nonunion, malunion, infection, arthritis, and bone loss. Quality of reduction is paramount in mitigating complications.
Approximately 20% to 30% of all talar neck fractures are open, and there is a high rate of associated injuries to the foot, ankle, and spine. Associated injuries to the musculoskeletal system are common and were present in 64% of Hawkins' patients and 45% of Pennal's patients. There are a high number of associated contralateral and ipsilateral foot injuries. The most common associated injuries are fractures of the medial malleolus and lumbar spine.
The neck represents the weakest portion of the talus because it has the smallest cross-sectional area and the greatest porosity due to vascular ingrowth. It is the only portion of the talus that is extraarticular, bridging the posterior, anterior, and middle facets of the talus. The orientation of the neck differs in both the sagittal (downward) and the horizontal (medial) planes, with the average deviation of the neck being 24 degrees (see Figs. 46-3 and 46-4 ).
Talar neck fractures most likely result from forced dorsiflexion of the foot with the ankle held rigidly in a neutral position, either from a compressive force through the heel or contraction of the gastro-soleus muscles. Older theories that hyper-dorsiflexion forcing the talar neck against the anterior edge of the tibia were not substantiated in cadaveric studies, instead leading to fractures of all the surrounding bones, including the tibia. The only way the talar neck would reproducibly fracture was to place the ankle in a neutral position, eliminate ankle motion by compressing the calcaneus against the overlying talus and tibia, and apply a dorsally directed force to the plantar surface of the foot at a point just distal to the talus. The talus thus acted as a cantilever between the plantar aspect of the foot and the tibia. Clinically, this is reproduced in an extended leg by contraction of the gastrocnemius or by pressing the heel against the floor of a vehicle.
The degree of the dorsally directed force determined the extent of the injury. If no further disruption occurred, a nondisplaced talar neck fracture would be the result. If the dorsally directed force continued, however, the posterior talocalcaneal and interosseous ligaments were disrupted, and the calcaneus translated anteriorly with the remainder of the foot. In association with this anterior displacement, the calcaneus dislocated in either a medial or a lateral direction. If the forces ceased at this point, the talar body tipped into equinus, and the talar head was displaced dorsally on the neck. However, further disruption would tear the posterior capsular ligaments of the ankle, and the talus would be forced backward out of the ankle mortise, much like a melon seed squeezed between two fingers. The talar body then came to lie between the posterior aspect of the medial malleolus and the anterior aspect of the Achilles tendon, with the fracture surface of the neck facing lateral and cephalad. This position was influenced by the curve of the posterior facet and the tethering effect of the intact deltoid ligament. The posterior tibial artery and nerve often escape injury because they lie anterior and are protected by the flexor hallucis longus muscle.
Forced supination of the foot can also create a talar neck fracture. Sneppen and Buhl reviewed 1806 ankle fractures and found 26 that had an associated talar neck fracture. They found that a supination force was most often associated with combined injuries. This also correlated with the observation made by Hawkins that the oblique or vertical fracture pattern of the medial malleolus suggested a compression fracture rather than a tension-type pattern. Penny and Davis also noted that severe fracture-dislocations were more often associated with fractures of the medial malleolus. Achilles tension at the time of impact also causes a supinatory stress through a varus hindfoot, which may explain the dorsomedial comminution present at the talar neck.
Early in the twentieth century, classification systems for talar fractures were broad and nonspecific. In 1952, Coltart published his series of talar injuries occurring during the Second World War. He noted that the injuries to the talus fell into three broad categories: fractures, fracture-dislocations, and total dislocations. Dunn et al, Mindell et al, Kenwright and Taylor, and Pennal all used this classification to evaluate their results. Weber and Marti developed a classification system based on anatomic location and displacement.
The most commonly used classification was initially described by Hawkins and later modified by Canale and Kelly, based on the radiographic appearance of the talus at the time of the injury ( Fig. 46-6 ). Because of its simplicity, usefulness in guiding treatment, and prognostic value, the Hawkins classification remains the standard for describing talar neck fractures. Hawkins originally described three injury “groups” with increasing severity, while Canale and Kelly added a fourth “type” to the original three for when the talonavicular joint is involved.
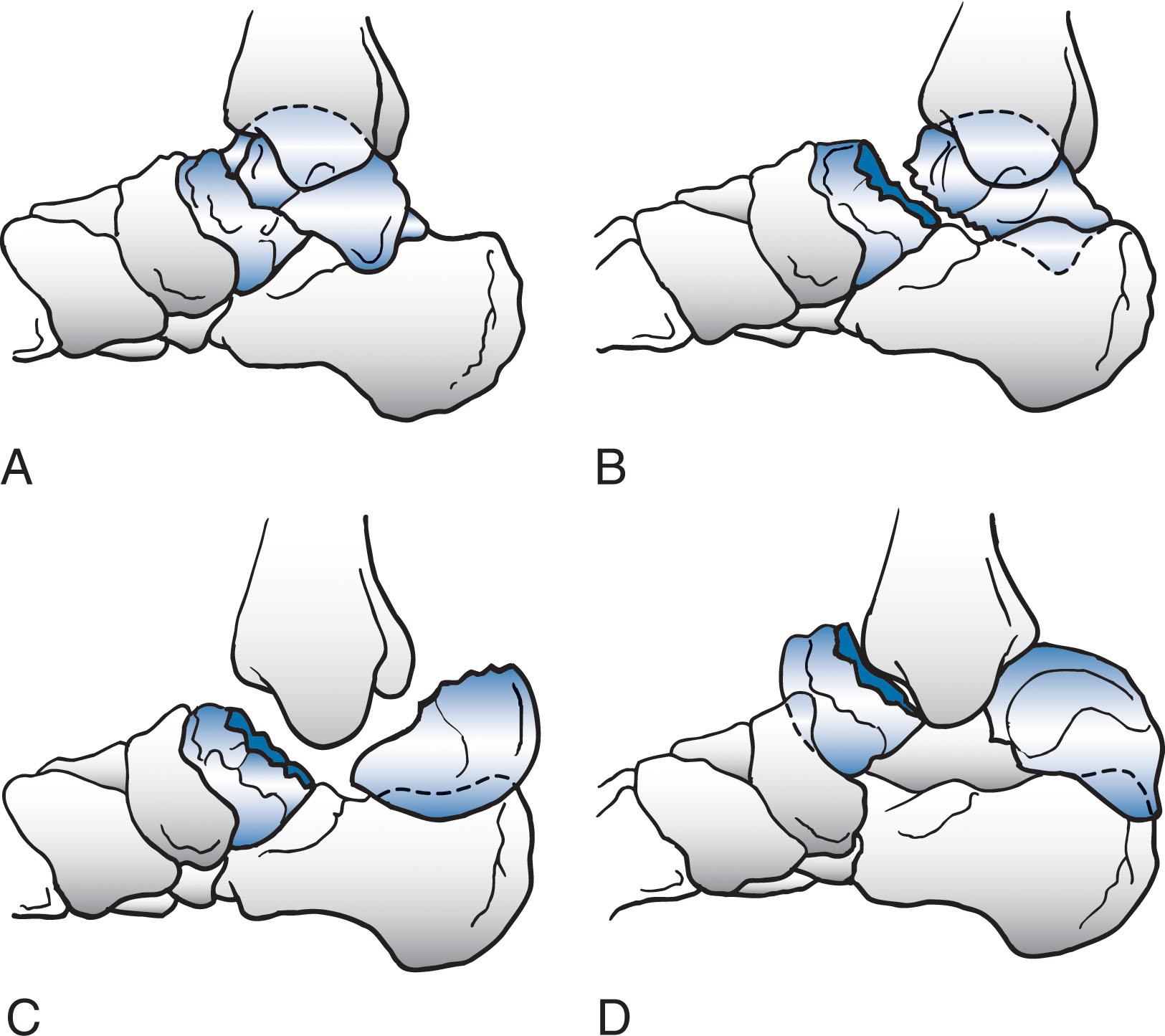
Type I fractures of the talar neck are nondisplaced, and the talar body maintains its normal relationship in both the ankle and subtalar joints (see Fig. 46-6A ). The fracture line exits the inferior aspect of the talar neck between the anterior and middle facets of the subtalar joint. The fracture line is often parallel to the x-ray beam on a lateral radiograph and can be easily missed on plain radiographs. In type I injuries, only one of the three main sources of blood supply to the talus is typically interrupted: the vessels that enter the foramina on the dorsolateral aspect of the talar neck and progress proximally into the body.
Type II fractures are displaced fractures of the talar neck with subluxation or dislocation of the subtalar joint (see Fig. 46-6B ). The associated subtalar dislocation can occur medially, secondary to an inversion force, or laterally if secondary to an eversion force. According to Penny and Davis, medial dislocation is more common. If the subtalar dislocation is complete, the injuries are often open because of the thin subcutaneous layer of tissue at the level of the ankle joint. The relationship of the talus in the ankle joint is normal, and the talar head retains its normal relationship with the navicular and the anterior facet of the subtalar joint. In type II injuries, at least two of the three sources of blood supply to the talus are interrupted: the blood supply proceeding proximally from the talar neck (as in type I) and that entering vascular foramina located inferiorly in the roof of the sinus tarsi and tarsal canal. The third main source of blood supply, that entering vascular foramina on the medial surface of the talar body, can also be injured.
In type III injuries, the vertical fracture of the talar neck is displaced and the talar body is dislocated from both the ankle and the subtalar joints (see Fig. 46-6C ). The talar body is often extruded posteriorly and medially and is thus located between the posterior surface of the tibia and the Achilles tendon. The talar head maintains its normal relationship with the navicular. The tibial neurovascular bundle is at risk, and the skin can be tented over the dislocated body fragment. Greater than 50% of type III fractures are open, and the skin may fail in tension over the anterolateral aspect of the ankle, or less likely the extruded fragment may create an open wound posteromedially. Vascular supply to the talus can be damaged.
Canale and Kelly added a fourth type of fracture dislocation, type IV , in which a fracture of the talar neck is associated with a dislocation of the body from the ankle or subtalar joint and a dislocation or subluxation of the talar head from the talonavicular joint (see Fig. 46-6D ). In this injury, damage to the vascularity of both the body (as in type III injuries) and the head and neck fragments is possible.
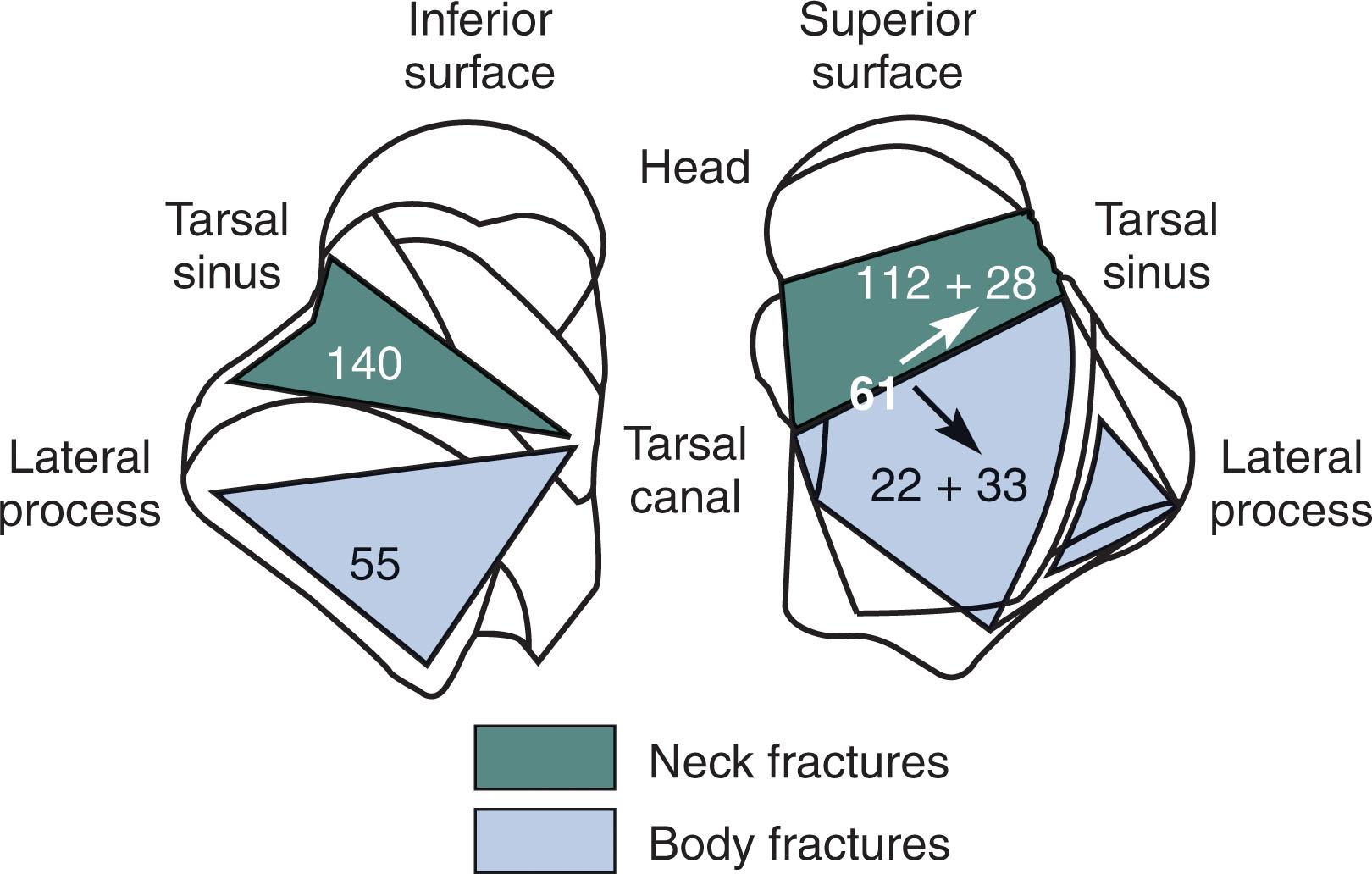
There is significant overlap between what may be termed a talar body or neck fracture, particularly when comminution from a talar neck fracture extends into the talar body. Both fractures types have similar rates of AVN and posttraumatic arthritis. Hawkins included vertical fractures of the talar neck that entered a portion of the talar body, with a fracture line involving the trochlea and the articular surface of the posterior facet of the subtalar joint. Inokuchi et al accurately defined the difference between vertical fractures of the neck and shear fractures of the body ( Fig. 46-7 ). In evaluating 215 fractures, they recognized that neck and body fractures could be distinguished most clearly by evaluating the fracture line on the inferior surface of the talus. The inferior fracture line consistently propagated either distal or proximal to the lateral process of the talus. Fractures distal to the lateral process entered the sinus tarsi and thus were extraarticular talar neck fractures. Fractures behind the lateral process entered the articular surface of the posterior facet and thus were intraarticular talar body fractures. This distinction can be helpful for when planning fixation constructs for the lateral side of the talus that either cross (body) or span (neck) the primary fracture line.
Patients with a talar neck fracture complain of severe pain in the foot and ankle. If the patient is seen before swelling is marked, the talar body can be palpated either anterior or posterior to the ankle. If displacement at the fracture site is associated with dislocation of the talar body, the normal contour of the ankle is distorted, with the rapid onset of swelling preventing palpation of the displaced talar body.
In these injuries, the pressure and tension from the displaced bones beneath the unyielding anterior skin are accompanied by extensive hemorrhagic infiltration of the tissues and venous thrombosis of the skin. This can result in an area of skin necrosis over the protruding bone ( Fig. 46-8 ). For this reason, any dislocation or fracture-dislocation of the talus can present a surgical urgency. Prompt restoration of the dislocation or the fractured fragment to its normal position is mandatory to relieve pressure and tension if there is any evidence of circulatory impairment in the skin. Bonnin reported a 73% slough rate in 56 irreducible dislocations, and McKeever noted the high correlation between skin necrosis and wound infection with subsequent osteomyelitis. However, with respect to AVN or posttraumatic arthritis, recent evidence suggest there is no effect of time to reduction for fracture or fracture-dislocations of the talus.
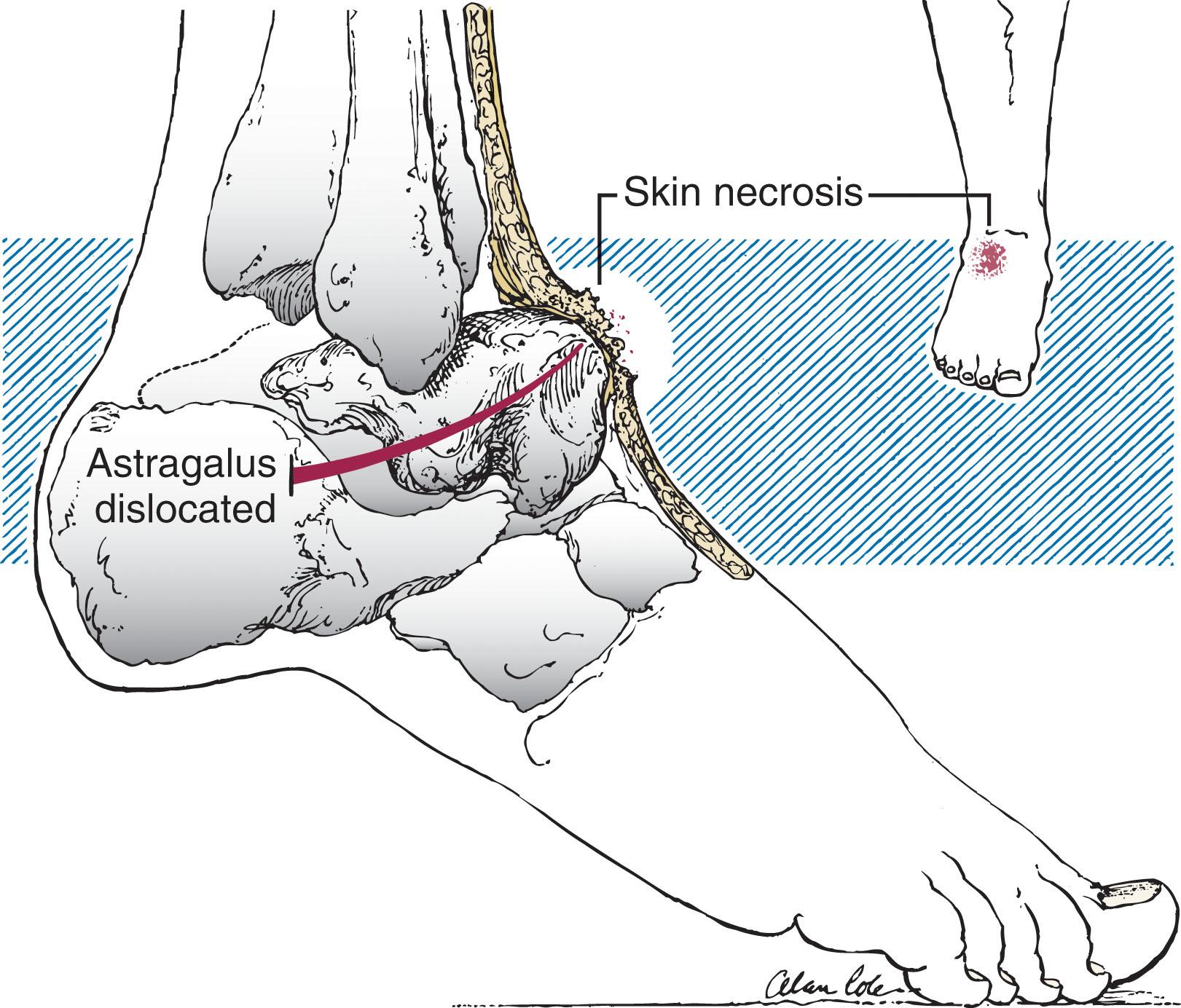
In fracture-dislocations where the talar body dislocates posteriorly, the bony fragment occupies the posterior capsular space, causing the tendons and neurovascular bundle to bowstring around it. Careful examination and documentation of the neurovascular examination should be performed. Clinically, the foot may have flexed toes. The patient has pain with contraction of the flexor hallucis longus and flexor digitorum longus muscles, and motion of the foot in any direction produces pain. If the talar body is significantly dislocated, the injury may be open (greater than 50% of the time in some series).
Routine anteroposterior (AP), lateral, and oblique radiographs of the ankle and foot are used in fracture evaluation. The lateral radiograph of the ankle best demonstrates fractures of the talar neck. The AP and oblique (mortise) views demonstrate the relationship of the talus within the ankle mortise. Radiographs are carefully reviewed for associated fractures, such as of the medial malleolus, calcaneus, navicular, and cuboid.
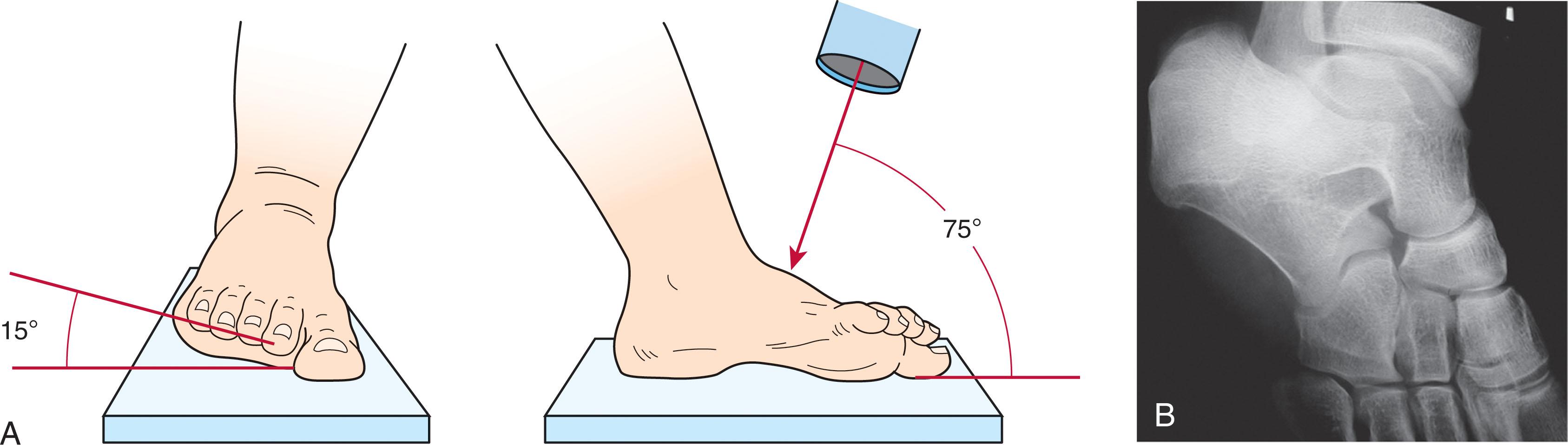
Canale and Kelly noted that the displacement seen in a talar neck fracture can occur in two planes. Dorsal-plantar displacement, which is noted on the lateral radiograph, is well recognized, whereas varus displacement is less often appreciated. Canale described a view to evaluate the entire talar neck ( Fig. 46-9 ). To obtain this view, the foot is maximally plantar flexed on an x-ray cassette and pronated 15 degrees, with the x-ray beam directed cephalad and pointing 75 degrees from the horizontal. This radiograph is helpful in determining the degree of initial displacement of a talar neck fracture for purposes of classification. In cases of surgical treatment, an intraoperative Canale view is essential to assure anatomic reconstruction of the talar neck.
Fine cut (1- to 2-mm ) multiplanar CT scanning is indicated to better delineate the fracture and assess for displacement. If closed reduction of the fracture is easily performed, the CT is more useful after reduction. CT scanning can also detect fractures initially missed on radiographs, such as a posterior process, a lateral process, and avulsion fractures, as well as acute osteochondral fractures and impaction fractures of the undersurface of the talus at the level of the posterior facet.
MRI is not indicated in the acute setting other than evaluating patients with suspected type I nondisplaced talar neck fractures with negative radiographs. Type I fractures are often missed and the patient is misdiagnosed with a sprained ankle. In the nonacute setting, however, MRI would be helpful in evaluating the region for ligamentous and osteochondral injuries.
The goals of treatment for fractures of the talar neck are anatomically reducing the fracture and surrounding joints, restoring alignment between the talar neck and body, and minimizing further vascular disruption. Attaining these goals provides the best opportunity to preserve motion, achieve joint stability, and minimize complications, such as infection, nonunion, malunion, posttraumatic arthrosis, and AVN.
Nonoperative treatment of talar neck fractures is reserved for truly nondisplaced type I fractures. Any displacement of the talar neck fracture, no matter how small, requires significant ligamentous disruption and results in subtalar subluxation or dislocation, thus representing a type II injury. If the fracture line is easily appreciated on the lateral radiograph, a CT scan should be obtained to classify the fracture correctly, because it will have ramifications for treatment and prognosis.
If the fracture is found to be truly nondisplaced, it should be immobilized in a non–weight-bearing removable splint to allow for early range of motion. Most authors recommend that the patient remain non–weight bearing for 6 to 8 weeks, or as long as 16 weeks, until radiographic signs of healing are present. CT scan confirmation of healing may be considered to avoid displacement of a previously nondisplaced fracture from premature weight bearing. Early range of motion of the ankle and subtalar joints is allowed in reliable patients while keeping them non–weight bearing.
The foot should be placed in neutral flexion in a non–weight bearing removable splint for 8 to 10 weeks so that range-of-motion exercises can be performed starting at 2 weeks. If the patient is not reliable, a cast should be used for 6 weeks before transitioning to a non–weight bearing removable splint to initiate range of motion. Most patients do not require physical therapy, unless stiffness is significant, at which point many months of exercise may be needed. Surgical intervention (as described next) is only required if the fracture displaces, or possibly in a patient unable to comply with weight bearing precautions to prevent displacement.
The incidence of AVN for type I fractures is 0% in most series. Although Canale and Kelly stated that aseptic necrosis occurred in 2 of 15 type I fractures (13%), Shelton and Pedowitz believed that these represented occult type II lesions that reduced spontaneously. Although nonunion after closed treatment of type I fractures has not been reported, a significant percentage of patients with type I fractures have decreased range of motion in the subtalar and ankle joints, leading to a worsened clinical result.
Type II fractures ( Fig. 46-10 ) are characterized by displacement of the talar neck fracture and an associated dislocation of the subtalar joint. Because of the dislocation, these injuries are often associated with compromise of the skin about the ankle, and prompt reduction is needed.

An immediate closed reduction should be attempted in the emergency department under conscious sedation. The foot is manipulated into full plantar flexion, thereby bringing the head in line with the body. The knee is then flexed to relax the deforming force of the gastrocnemius. Reduction of the subtalar joint is then obtained by manipulating the hindfoot into either inversion or eversion, depending on whether the subtalar component of the dislocation is medial or lateral. Repeated forceful attempts at closed reduction are discouraged; if closed reduction of the subtalar dislocation is unsuccessful, open reduction in the operating room is required.
Open anatomic reduction and stable internal fixation is recommended for definitive treatment of displaced talar neck fractures. Small amounts of malalignment and displacement translate to significantly altered mechanics of the subtalar joint. Historically, despite a lack of sufficient evidence, urgent treatment of displaced talar neck fractures was advocated to reduce the risk of AVN. However, more recent studies suggest no relationship between the timing of surgery and the subsequent development of AVN. Instead, the displacement of the fracture, fracture comminution, soft tissue injury (open fractures), and quality of surgical reduction impact the development of AVN, union rates, and overall result.
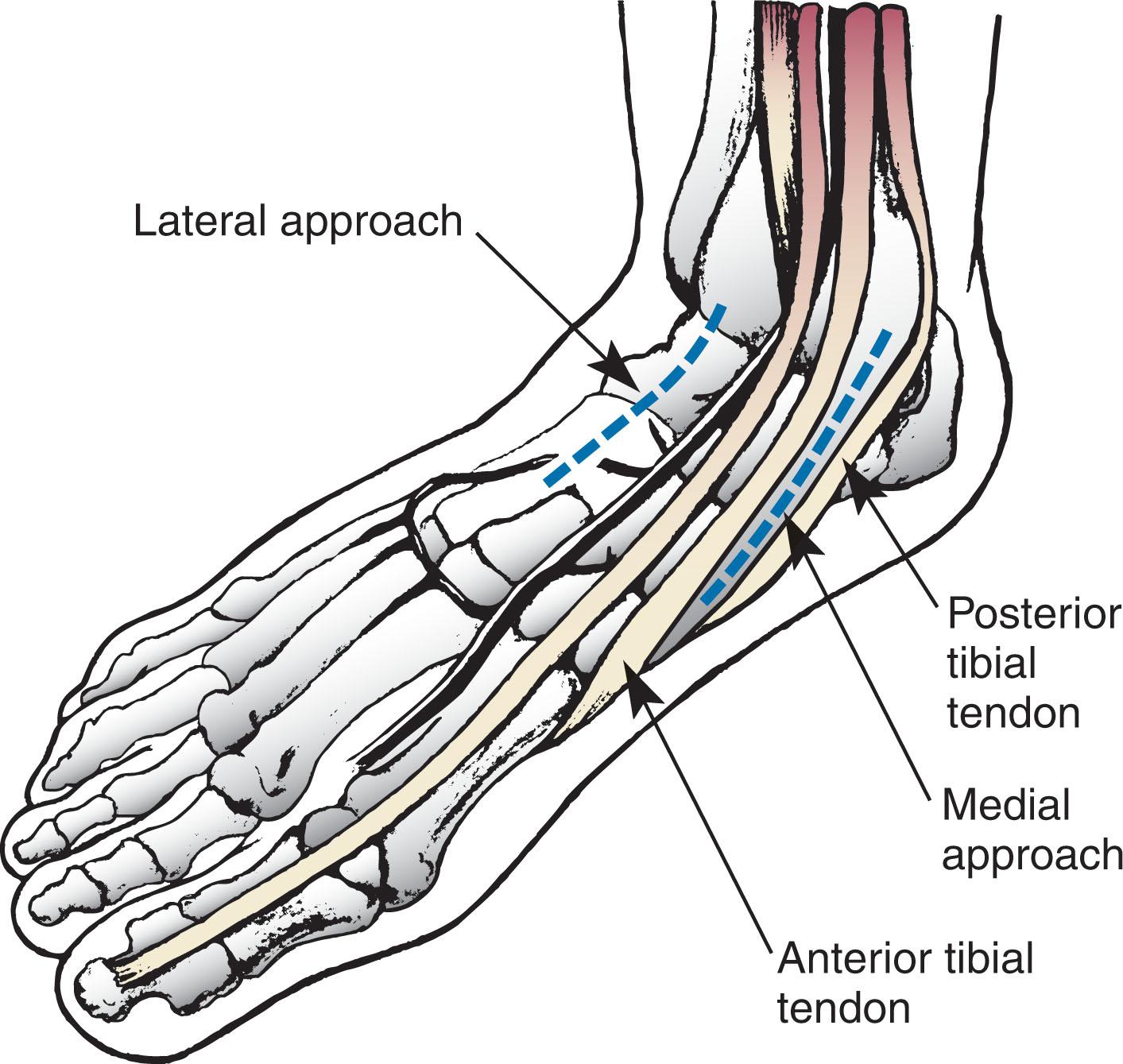
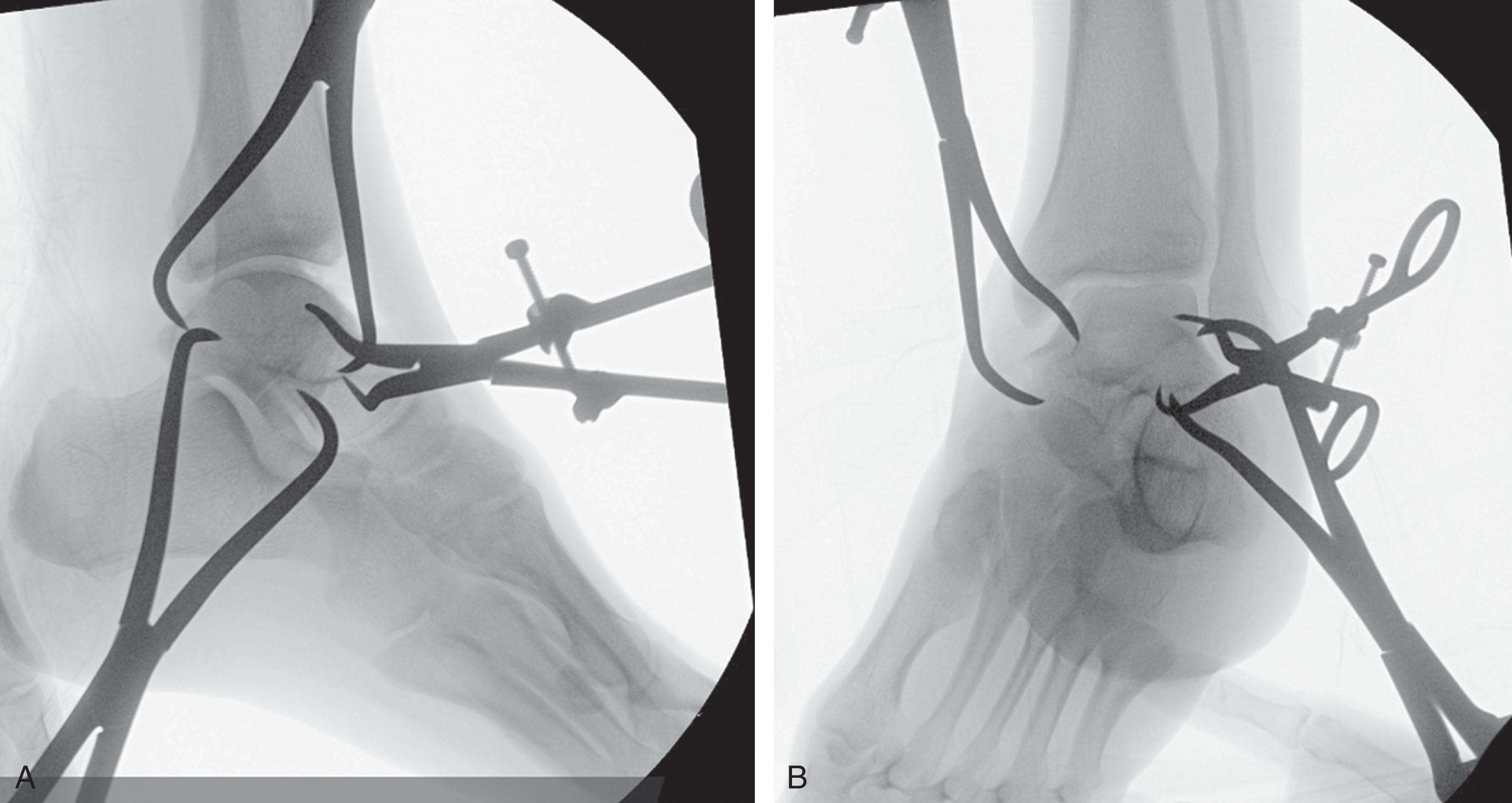
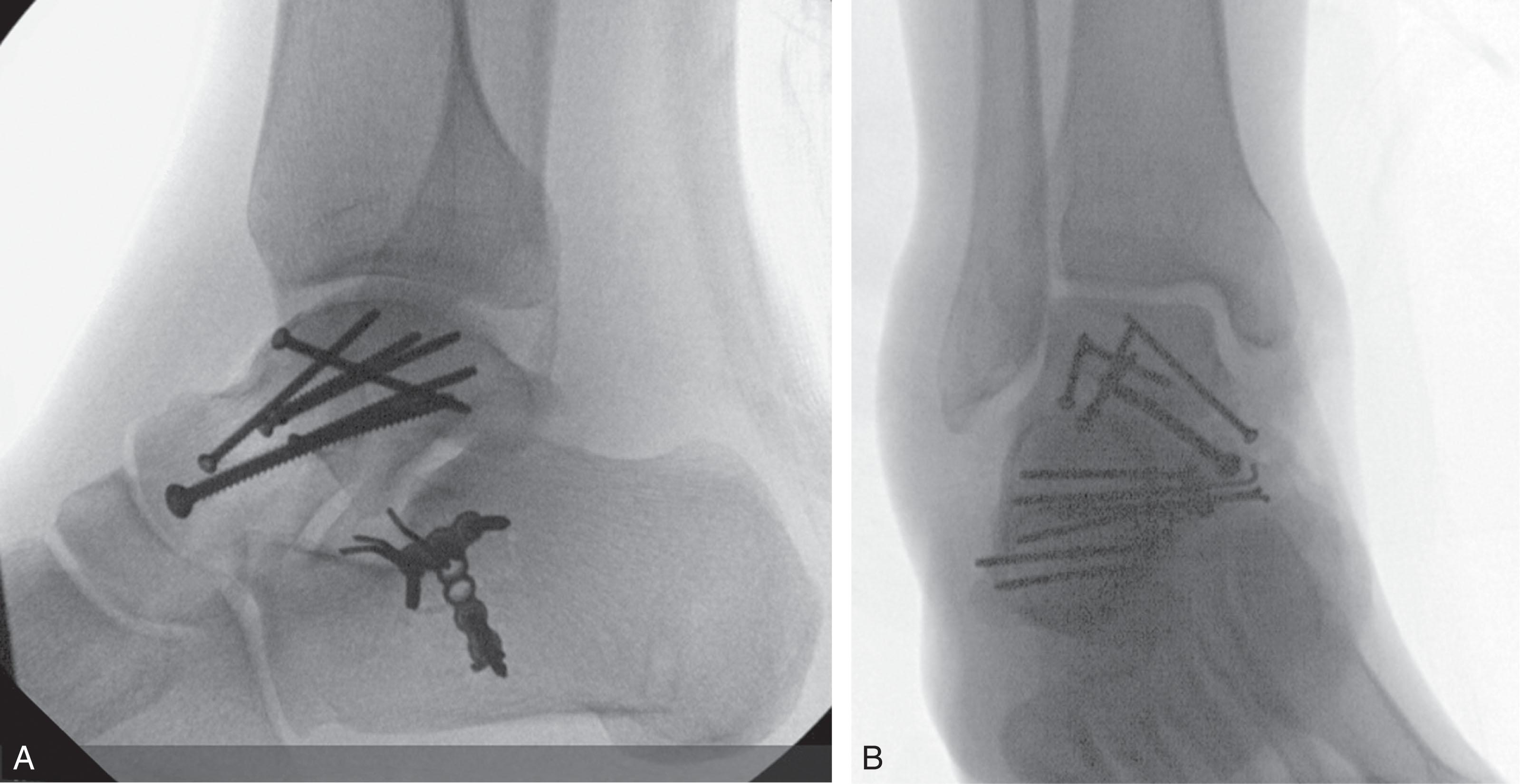
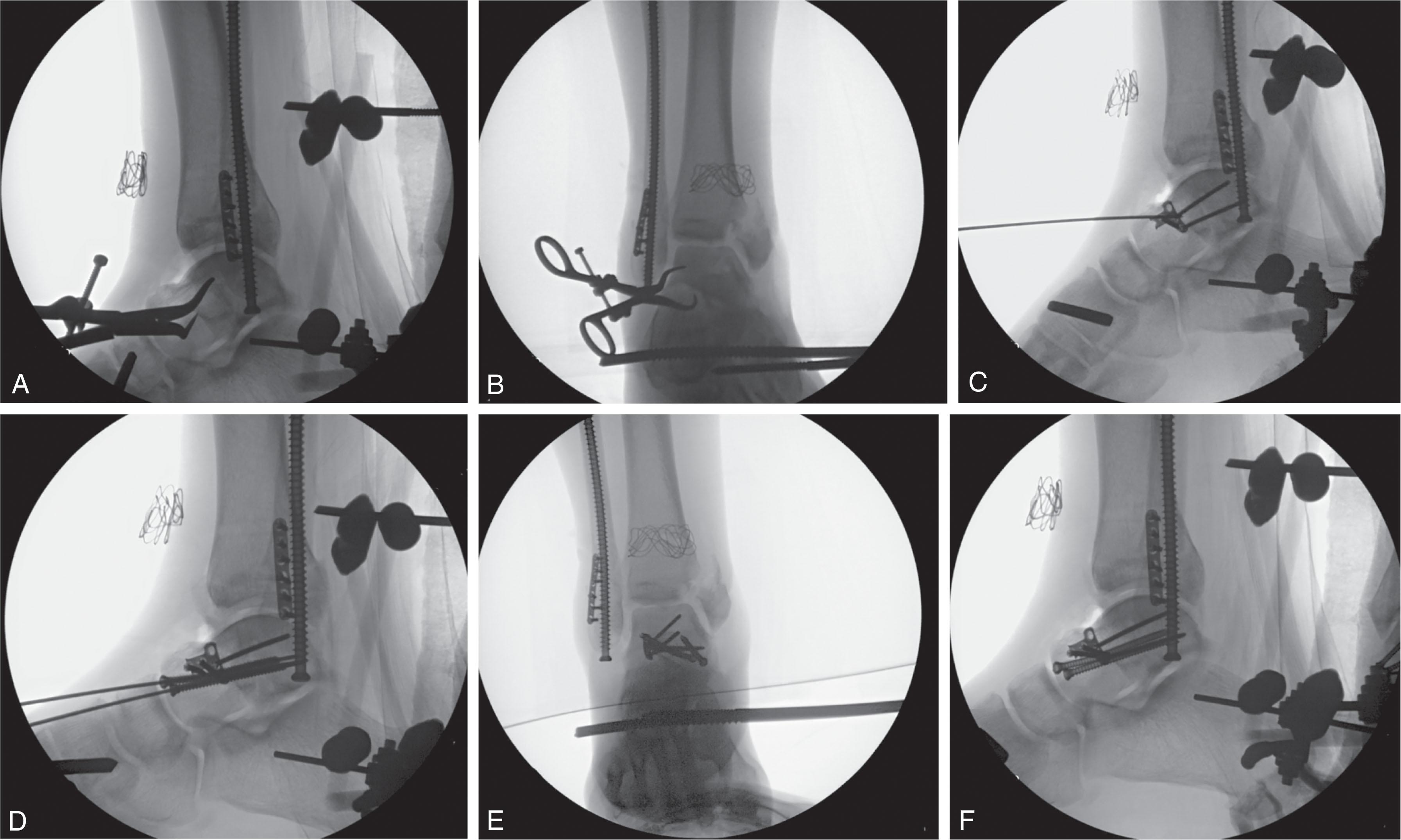
Because reduction quality is paramount, a dual anteromedial and anterolateral open approach is typically performed for direct assessment ( Fig. 46-11 ). If the condition of the soft tissue envelope precludes an open approach (e.g., hemorrhagic skin blisters, swelling), a medial ankle spanning external fixator can be applied to assist with reduction of the subtalar dislocation and provide stabilization until soft tissues allow for an open approach ( Fig. 46-12 ).

Reduction strategy depends on fracture characteristics. Reduction aids such as dental picks, small terminally thread Schantz pins for joysticks, and shoulder hooks can be useful to obtain an anatomic reduction Typically, the fracture fails in varus with tension on the lateral side and compression on the medial. It is often useful to first reduce the lateral side directly with a clamp while assessing the lateral and dorsal neck ( Fig. 46-13 ). Because the medial side often failed in varus at the time of injury, there can be significant comminution and impaction. Overcompression of the medial side with a clamp for cortical apposition can worsen this deformity. There are some instances when the impaction must be addressed with structural bone grafting to prevent varus failure and restore alignment. When unable to directly access the medial fracture secondary to comminution, the surgeon can rely on reduction of the lateral and superior neck and radiographic assessment.
Fixation strategy also depends on fracture characteristics, particularly the exit point of the neck fracture laterally. If the fracture exits proximal to the lateral process, then independent small fragment screws can be inserted across the fracture line laterally. Alternatively, if the fracture exits distal to the lateral process, it is often difficult to transverse the fracture with screw fixation from the lateral side. In this scenario, mini fragment plates can be placed across the neck to act as a tension band, with at least two points of fixation proximal and distal to fracture ( Fig. 46-14 ). If there is lateral side comminution, the plate functions to bridge the fracture, and consideration should be made for a more stout plate with greater bending strength.
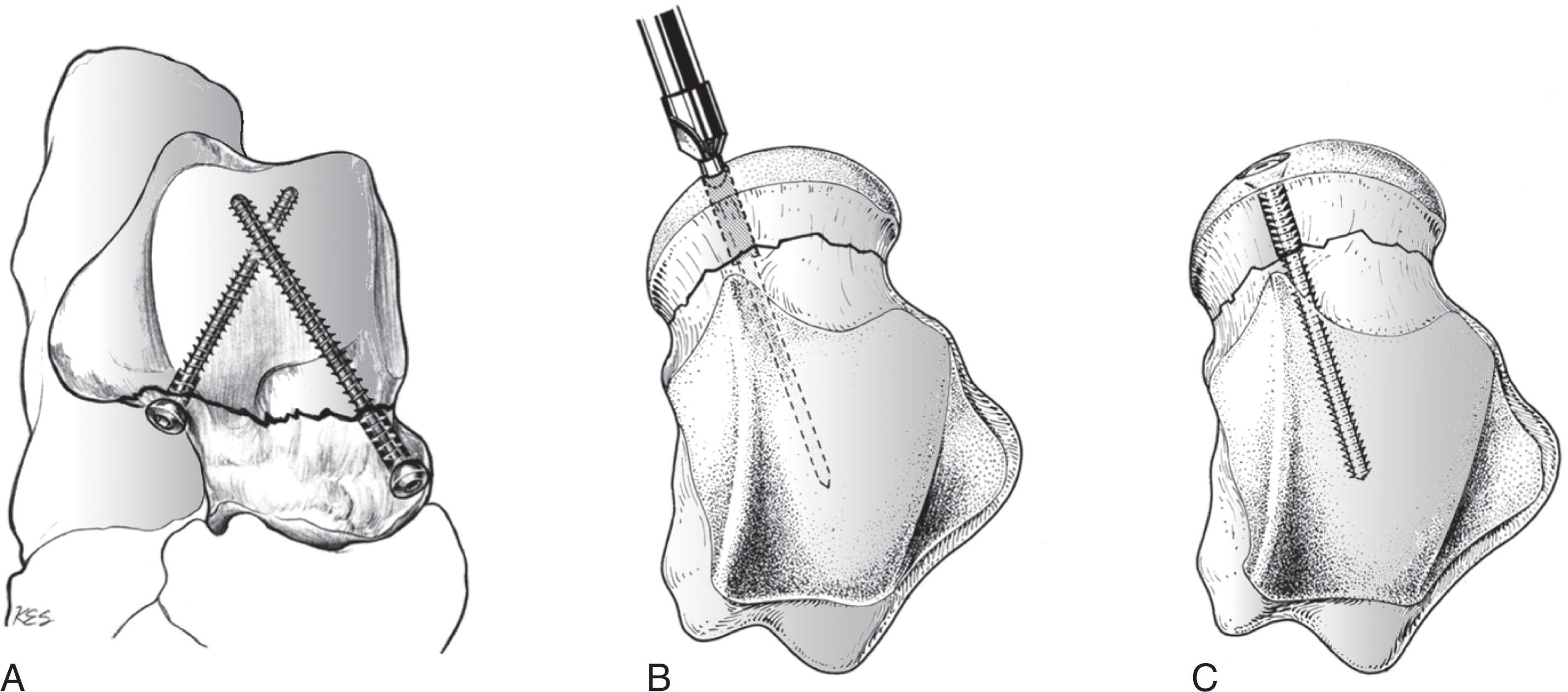
Fixation of the medial column of the talar neck fractures typically employs independent screw fixation. Retrograde small or mini fragment positional screws can be inserted and buried into the talar head cartilage ( Fig. 46-15B and C ). These strut screws prevent varus collapse of the medial column. Strategic resection of medial boarder of the navicular with a small rongeur can create a screw path with little clinical consequence if abduction of the forefoot is insufficient to allow for screw placement. The surgeon must be careful when using lag screws medially as this may exaggerate varus deformity. There are some scenarios where a small medial spanning bridge plate can be placed in the extraarticular recess between the talar head and body, across the neck.
The authors manage displaced talar neck fracture with open reduction and surgical fixation for definitive treatment when the soft tissues allow. If the subtalar joint is not able to be reduced closed in the emergency department, the patient is taken for reduction in the operating room. Attempt at a closed reduction is then performed under anesthesia.
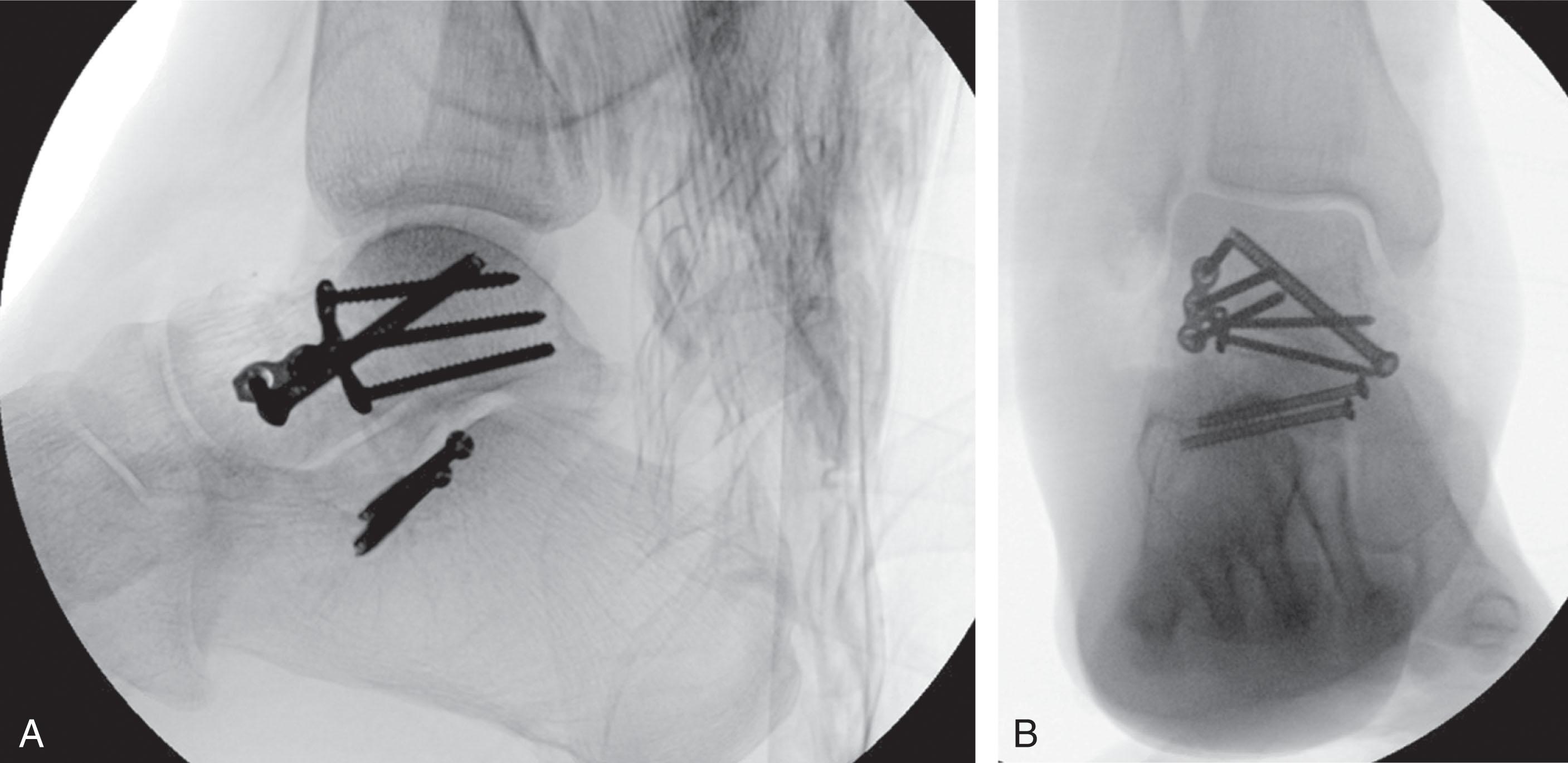
For definitive treatment, patients are placed supine on a radiolucent table. The fracture is approached through dual incision, medially and laterally. After anatomic reduction, the fracture is held with provisional K-wires. For simple noncomminuted fractures, the talus is stabilized with 2.7 mm lag screws by technique placed retrograde through the distal portion of the talar neck or the talar head (with countersinking) to achieve bicolumnar fixation ( Fig. 46-16 ).
In many cases, the dorsomedial portion of the talar neck is comminuted, precluding an optimal “read” of the fracture. The authors therefore use the lateral approach to obtain fracture reduction. In these cases, the authors prefer to stabilize the lateral neck with a screw, as described above, or with a 2.0- or 2.4-mm plate contoured to fit the lateral-aspect talus. Adequate intraoperative fluoroscopic verification of reduction is performed (including a Canale view), taking care in particular to ensure that the neck is not placed in varus because of the medial comminution. The medial neck is then spanned with a 2.0-mm or 2.4-mm bridge plate or a 3.5- or 2.7-mm fully threaded screw to prevent collapse across the comminution. Although less common, if the lateral talar neck is comminuted, then the medial neck is used for initial fracture reduction, followed by spanning fixation of the lateral neck. Bony defects are filled with autogenous cancellous graft from the ipsilateral calcaneous or Gerdy’s tubercle. If the subtalar joint has significant injury, the authors recommend performing primary subtalar arthrodesis with screw fixation after removal of the remaining articular cartilage of the joint.
Plate fixation of talar neck and body fractures is a useful adjunct to screws. Larger (3.5 mm or 2.7 mm) lag or position screws are optimally inserted perpendicular to the talar neck fracture or along the long axis of the talus, but this is sometimes difficult to achieve because of the anatomy of the talar head and neck. Using small- or mini-fragment plates to stabilize the fracture can avoid this difficulty. In cases of comminution, as discussed above, small- or mini-fragment plates allow spanning of the fracture while preventing collapse or shortening.
The authors prefer using 2.0- or 2.4-mm plates, because these plates are low profile and easily contoured to fit the medial and/or lateral talar neck ( Fig. 46-17 ). In most cases, depending on the remaining bone stock and quality of the fractured talus, the authors have not found it necessary to use locked plates. The low thread pitch of 2.0- and 2.4-mm screws allows excellent purchase in the talus. However, in cases of significant talar neck comminution or osteoporosis, a locked mini-fragment plate is useful. When plate fixation is used, the ankle should be plantar and dorsiflexed intraoperatively and carefully examined to ensure that the plates do not impinge on the medial malleolus, lateral malleolus, or talonavicular joint.
After anatomic reduction and stable fixation, the patient should be kept non–weight bearing for a minimum of 8 to 12 weeks, with early motion of the tibiotalar and subtalar joints initiated at 2 weeks. Weight bearing is not commenced until clinical and radiographic signs indicate the fracture has healed. Penny and Davis noted that uncomplicated fracture healing occurred by 10 to 12 weeks, but Kenwright and Taylor noted these fractures can take as long as 4 months to heal.
The results of type II talar neck fractures are somewhat unpredictable when compared with types I and III fractures. Nonunion rates are low, but Kenwright and Taylor had 2 (14%) of 14 type II fractures that developed delayed unions that went on to AVN.
The most common complications of type II fracture are AVN and subtalar or, rarely, ankle arthrosis. A recent systematic review reported AVN in 15.9% and osteoarthritis in 41.3% of type II fractures overall. Rates of AVN in clinical series vary from 0% to 50%. Posttraumatic arthrosis is more common and has been reported as high as 90% in some series. Vallier et al suggested that worse results in type II and type III talar neck fractures were seen with comminuted and open fractures, suggesting that the initial injury had a substantial impact on the result.
When critically reviewing the literature, most series include nondisplaced and displaced neck fractures in conjunction with associated juxtaarticular fractures. This can falsely decrease the true incidence of AVN and increase the true incidence of posttraumatic arthritis. In addition, many of the older series treated type II injuries without internal fixation, making comparison with current treatment standards difficult.
Differentiation between type II fractures with associated subtalar dislocation versus those with only displacement helps to predict the development of AVN. In one study, patients who sustained type II fractures without associated subtalar dislocation did not develop AVN.
In type III fractures, the talar body is displaced from both the ankle and the subtalar joints. The talar body usually rests posteriorly and medially and rotates around the deep fibers of the deltoid ligament. The blood supply to the talar body is completely disrupted, with the possible exception of that through the deltoid ligament. Nearly 50% of these injuries are open. If the injury is not open, however, the displaced body usually puts extreme tension on the overlying skin, which can result in necrosis unless prompt reduction is instituted.
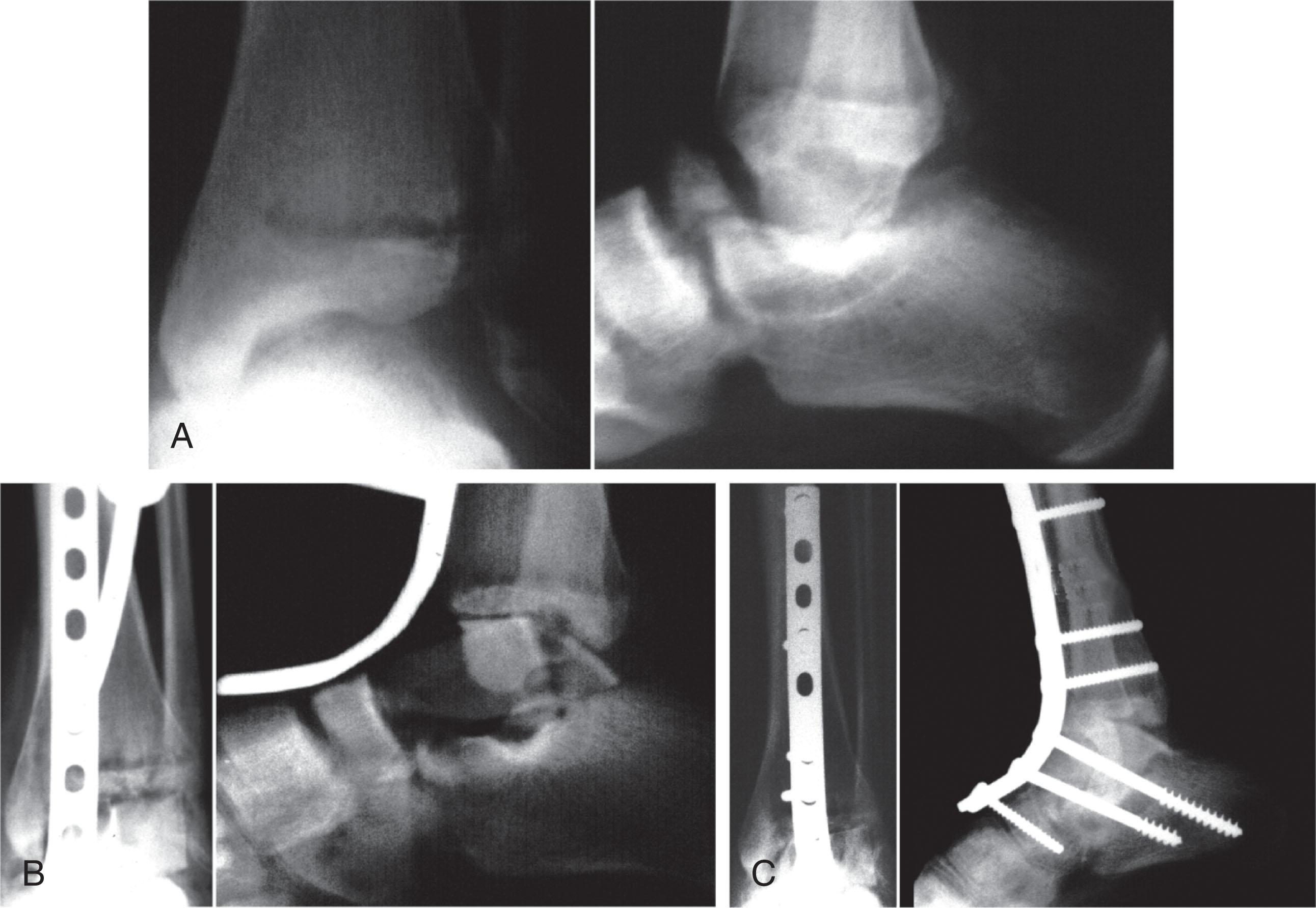
Closed reduction should be attempted in the emergency department solely to relieve tension on the overlying skin and neurovascular structures. With closed injuries (see Fig. 46-17 ), closed reduction is very challenging. Kenwright and Taylor were successful in obtaining a closed reduction in only one patient. The maneuver for reduction is similar to that described above for type II fractures but is aided by adequate patient relaxation, flexion of the knee to relax the gastrocnemius muscle, and application of transcutaneous pressure on the dislocated talar body in an anterior direction. Placement of a transcalcaneal traction pin aids in reduction and manipulation of the hindfoot.
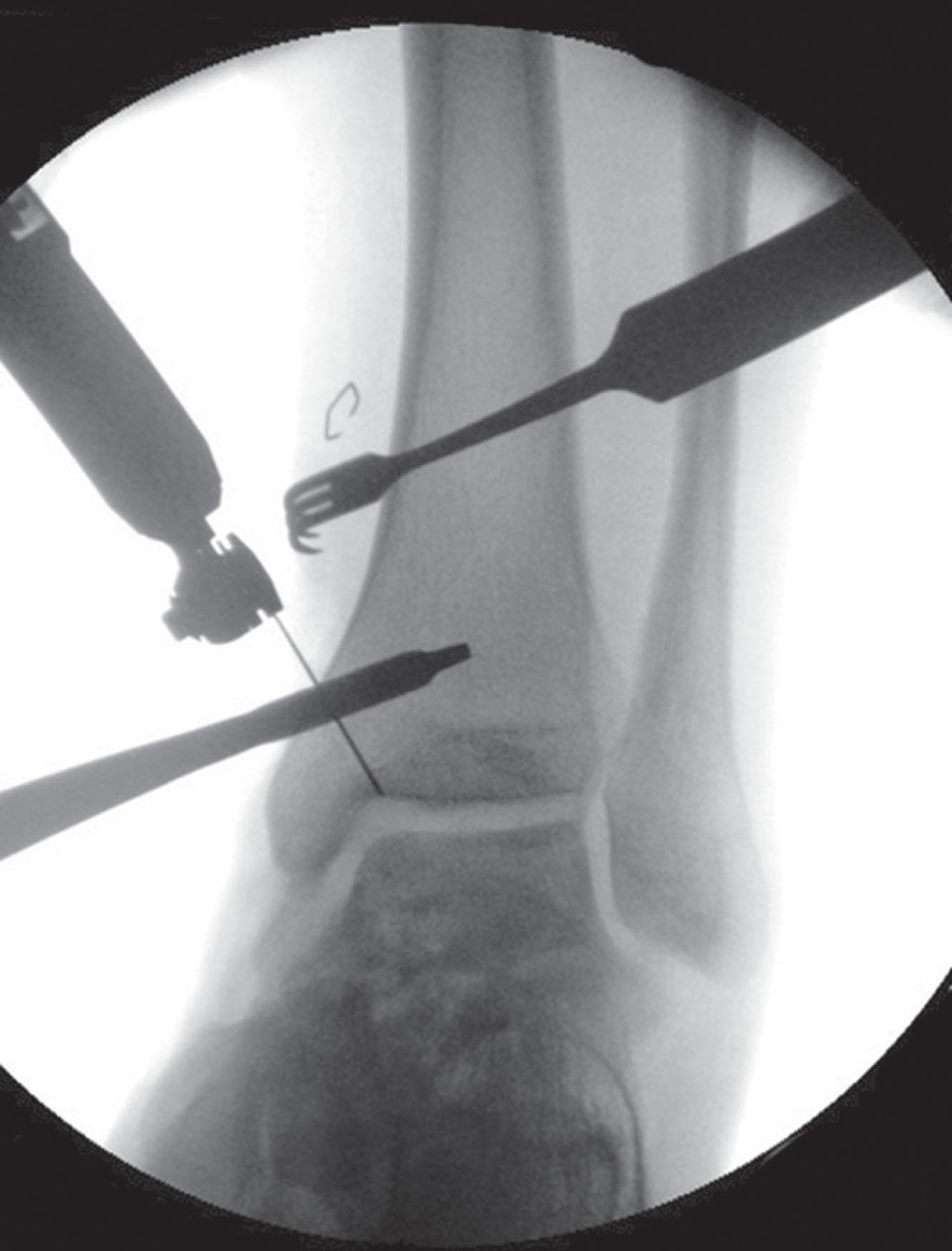
If closed reduction is unsuccessful in the emergency department, reduction should proceed in the operating room at the next available opportunity. External fixation assisted reduction can be helpful to distract the hindfoot and create space for the dislocated talar body to reduce. Alternatively, a universal distractor can be applied, with medial pins in the tibia and calcaneus. Often, percutaneous reduction aids, such as Schantz pins or shoulder hooks, can be useful to gain control of the talar body ( Fig. 46-18 ). If percutaneous reduction aids are unsuccessful, an open reduction is required. A medial ankle spanning ex-fix can be useful to help maintain the reduction until soft tissues allow for definitive fixation (see Fig. 46-12 ).
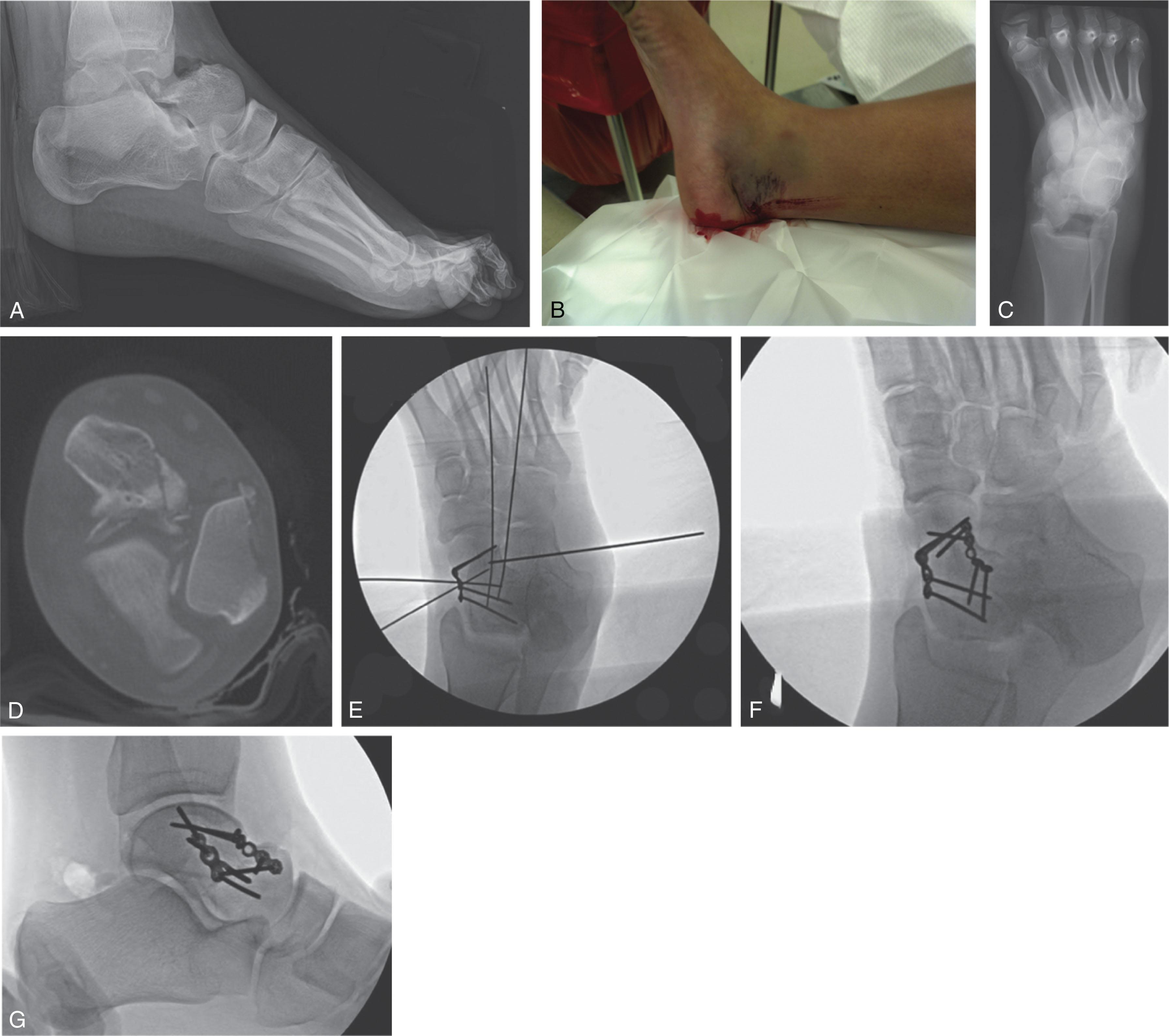
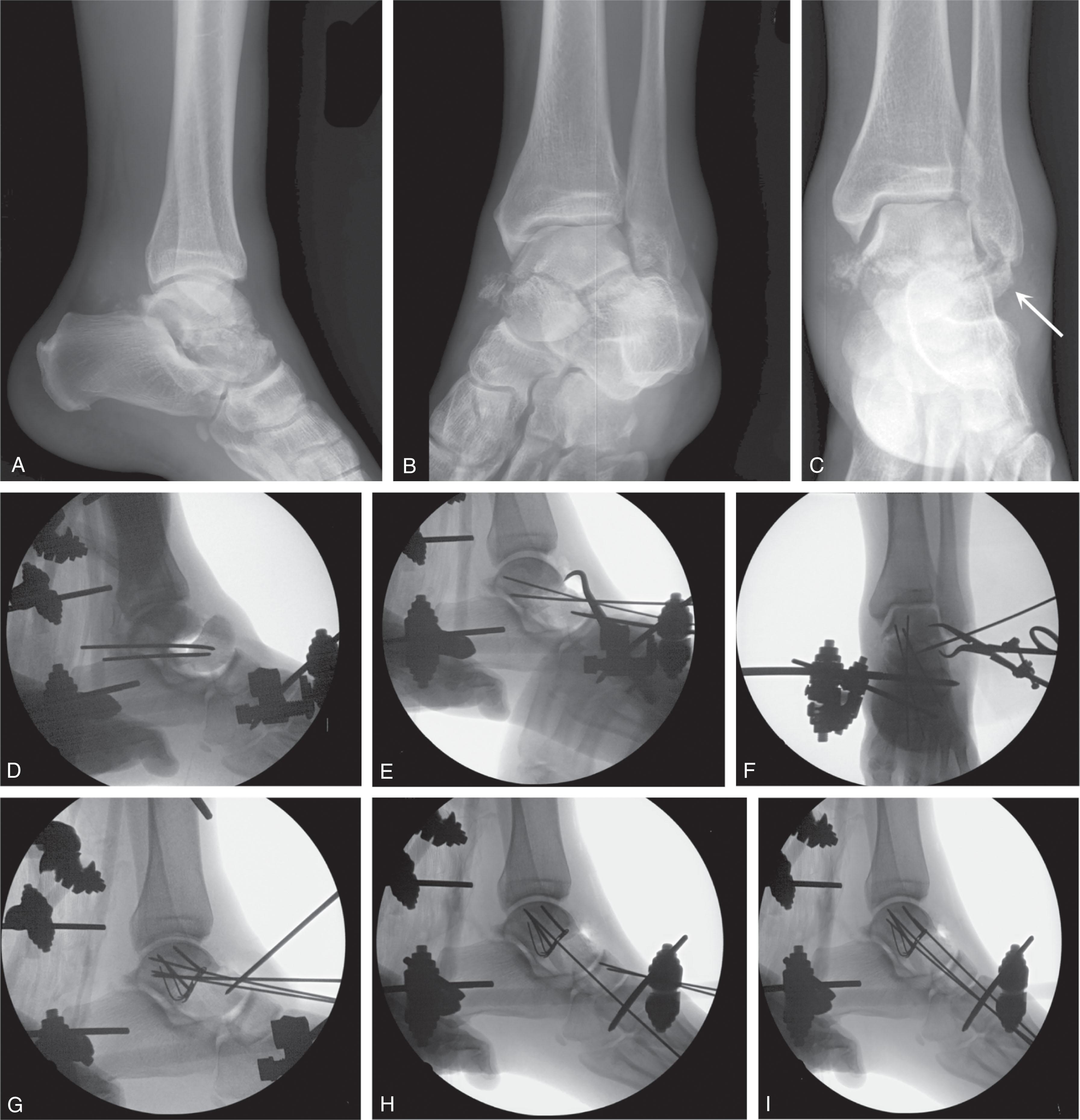
Once the talus body is reduced and the soft tissue injury is recovered, definitive surgical treatment proceeds similarly to type II fractures. An example of definitive surgical sequence after reduction of the talar body and external fixation was performed at the index procedure is demonstrated in Fig. 46-19 (this patient had a concomitant supination adduction ankle fracture that was addressed as a different stage).
The authors recommend urgent attempted reduction of these fractures in the emergency department. If the fracture can be reduced by closed means, urgent operative treatment is not required. If closed reduction cannot be achieved, the authors recommend urgent operative treatment to relieve pressure on the skin and neurovascular structures.
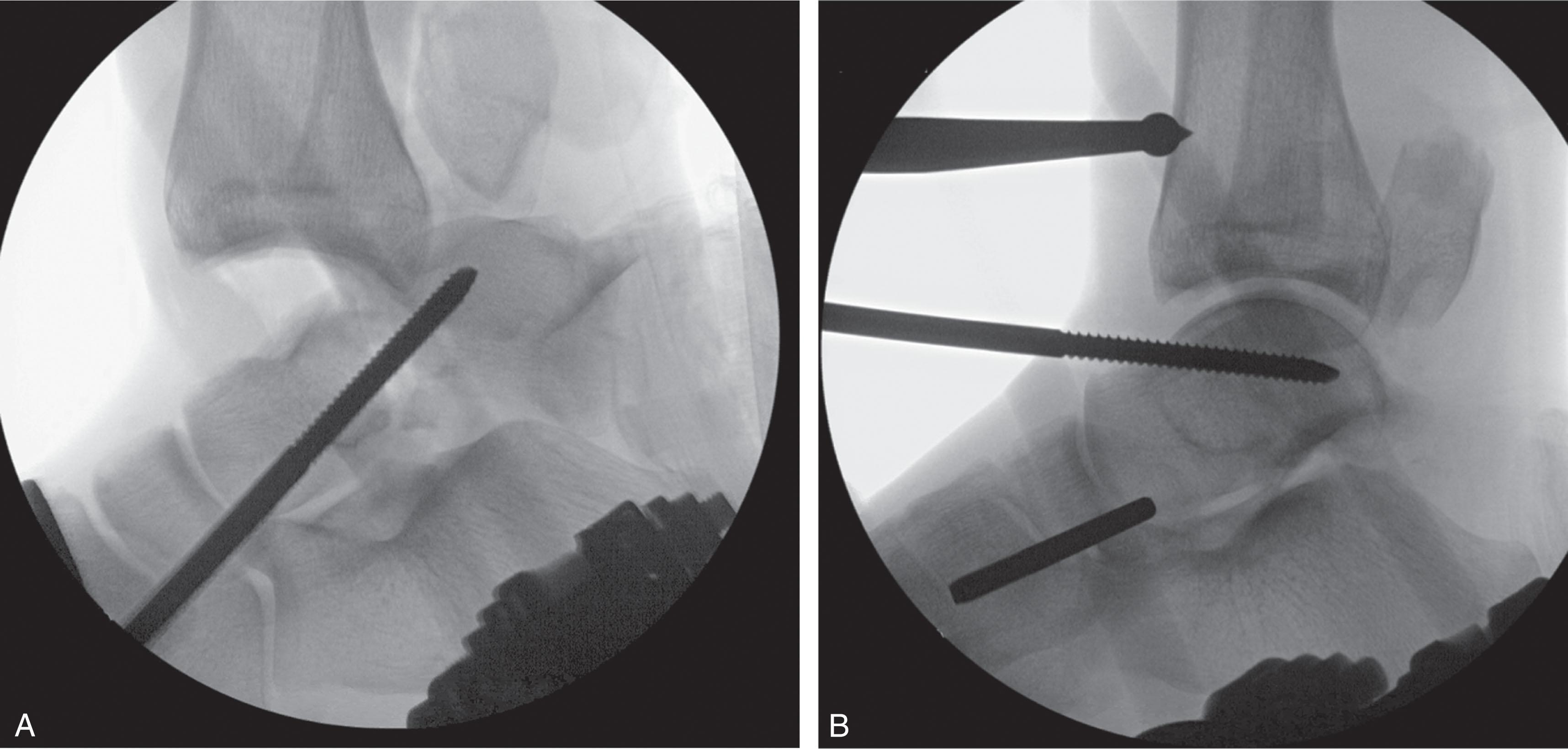
Once in the operating room, reduction is again attempted after adequate relaxation of the patient. If reduction remains difficult, the authors place a medial distractor or external fixator for traveling traction from the tibia to the calcaneus. As mentioned, percutaneous reduction techniques can be utilized. If reduction remains elusive, an open anteromedial approach is indicated. As a last resort, a medial malleolus osteotomy can be considered ( Fig. 46-20 ). At times, both the distractor and osteotomy will be required to allow reduction of the displaced fragment.
After reduction of the dislocated body, the talar neck is anatomically reduced and stabilized as described for type II fractures above. The authors typically make dual anteromedial and anterolateral approaches to the talus. If the tibiotalar joints or subtalar joints remain grossly unstable after reduction of the fracture, a temporary foot spanning external fixator may be applied, or a temporary K-wire may be placed across the unstable joints.
Postoperative care is similar to that of type II fractures, although fracture healing may be prolonged because of the severe nature of the injury. The average time for osseous union is prolonged; in Kenwright and Taylor's series, it was a minimum of 5 months, and Penny and Davis noted that it could take as long as 8 months to unite.
The long-term results of type III talar neck fractures were historically poor. With the advent of modern fixation techniques and implants, outcomes have improved. A recent systematic review found 38.9% rate of AVN and 54.2% of posttraumatic arthritis for type III injures. There is a decrease in the average AOFAS outcome score when comparing type II (86.1) to type III (68.3) talar neck injuries.
Eight years after Hawkins's landmark paper, Canale and Kelly described a variant of the Hawkins type III fracture, the type IV fracture. This injury involves a fracture of the talar neck with a subluxation or dislocation of the talar body, as in a type III fracture, but there is also an associated dislocation of the talar head.
Type IV fractures should be treated according to the principles outlined in the previous sections. An example sequence of a type IV neck fracture with an associated lateral process injury is demonstrated in Fig. 46-21 . This fracture-dislocation is significant because AVN of both the talar body and the head fragment is possible. Data from a systematic review suggest modern AVN rates are about 55% and posttraumatic arthritis is 73% for these type IV fractures.
Open fractures of the talar neck are particularly challenging because of the high degree of injury and subsequent risk of infection, AVN, and posttraumatic arthrosis. Fractures are classified at the time of surgery according to the classifications of Gustilo et al. When the skin is torn in tension secondary to talar body extrusion, irrigation and debridement with open reduction and internal fixation (ORIF) and primary skin closure are recommended. Most authors suggest that if the fractured and dislocated body fragment is attached by a thread of medial soft tissue, reduction and fixation should be attempted after thorough irrigation and debridement.
Certain authors believe that after irrigation and debridement, followed by ORIF, a primary fusion should be attempted. Grob et al suggested primary tibiotalar fusion. Kleiger, Boyd and Knight, Pennal, Canale and Kelly, and Szyszkowitz et al all performed primary subtalar fusions in at least one type III fracture in their respective series, in the hope of revascularizing the talus. Pennal noted that despite using the primary subtalar fusion in three patients, all three still developed AVN. In Hawkins’s series, three subtalar fusions were performed in the hope of increasing vascularity to the talus. Subtalar fusion neither facilitated replacement time in the dead talar body nor protected against late collapse or arthritis.
More controversial is the treatment of Hawkins type III or IV fractures that are associated with a complete separation of the talar body from all soft tissue attachments. This may be seen occasionally in a closed fracture, but it is more often seen in open injuries, with the paramedics bringing the free fragment to the hospital wrapped in ice. A decision must be made whether to reimplant or discard the fragment, based on the wound and degree of contamination. If the fragment is not available or is discarded by the surgeon at treatment, a decision also must be made about subsequent treatment of the foot.
Limited case series describe results of reimplantation of the extruded talar body. Dunn et al replaced a sterilized talar body only to have it subsequently develop osteomyelitis. Böhler and Coltart recommended that the talar body not be discarded because its removal would cause severe and lasting disability. Allgower recommended bone debridement and reinsertion unless the fragment was severely damaged or contaminated, followed by internal fixation and early motion without fusion.
Similarly, limited series describe acute talectomy with or without Blair or tibiocalcaneal fusion. Hawkins performed five primary talectomies for type III fractures; all patients had long-term pain, limb shortening, foot widening, and difficulty with footwear. Pennal performed three subtotal talectomies (body) for this injury; two were left without further treatment, and one underwent a tibiocalcaneal fusion. Patients with a talectomy alone had severely painful feet, whereas the tibiocalcaneal fusion did well functionally. Canale and Kelly had one patient who was treated with a talectomy alone and went on to a poor result. Their other patient, who had a total body extrusion and a subsequent tibiocalcaneal fusion, had a fair result. Penny and Davis, Morris et al, and Dennis and Tullos believed that early excision with subtotal or total talectomy should be performed in these patients, followed within 6 weeks by a Blair fusion. Although Penny and Davis and Morris’s group reported excellent results, Dennis and Tullos had good results (five of seven), with a 29% pseudarthrosis rate. Reckling, using the same principles, used tibiocalcaneal fusion with good results. Sanders et al, in treating 11 open Gustilo type IIIB wounds with fractures of the talus and tibial pilon, had two Hawkins type III injuries in which the talar body was lost at the scene of the accident. These patients underwent irrigation and debridement, external fixation, and free flap coverage of their wounds, followed by 6 weeks of intravenous (IV) antibiotics. Once clean, the flap was lifted, and an iliac crest bone block pantalar fusion using an anterior plate was performed ( Fig. 46-22 ). Despite complete union without infection, these patients were severely limited by their disability.
Marsh et al reported on 18 severe open talar injuries, including 13 Hawkins type III fracture-dislocations, one type IV fracture-dislocation, and four total talar dislocations. In 12 (67%) patients, the talus or talar body was totally or partially extruded through the wound. All patients were emergently treated in the operating room, internal fixation was performed in 11, and one patient was treated with a primary talectomy. Wound severity included four Gustilo type II, 10 type IIIA, three type IIIB, and one type IIIC wounds. Seven wounds were primarily closed, five closures were delayed, four were closed by secondary intention, one case required a split-thickness skin graft, and one was covered by a local rotation flap. Seven of 18 feet (38%) developed either osteomyelitis or septic arthritis. Statistical analysis comparing the infected and noninfected groups showed a significantly greater percentage of extrusion in the infected group, a greater percentage of failures in the infected group, and a significantly longer mean length of hospital stay compared with the noninfected group. Marsh et al concluded that the functional result of patients with major open injuries to the talus correlated with the occurrence of infection; of the seven noninfected cases, only one (14%) was rated a failure, whereas of the seven infected cases, five (71%) were failures. As infection negatively affected result, and several of these patients required late talar body excision as part of a reconstruction, these patients might have benefited from primary excision of the talar body to avoid infection.
Smith et al reviewed the results of 27 patients with complete open extrusion of the talus. Thirteen patients had Hawkins type III or type IV fractures, and eight patients had pure pantalar dislocations without associated talus fractures. The remainder of patients had smaller fractures of the talar head, lateral process, or body. Twenty-four of 27 patients underwent reimplantation of the extruded talus. One patient underwent below-knee amputation. One patient underwent talectomy for an unreconstructable injury because of comminution. One patient underwent primary tibiocalcaneal arthrodesis with the extruded body used as autograft. Nineteen patients had a minimum of 1-year follow-up. Of these 19, nine patients had a major fracture of the talar neck or body. Almost all of these patients developed talar collapse, AVN, and/or posttraumatic arthrosis. Only one patient in this series developed an acute infection 2 weeks after the original injury. A second patient developed a wound infection after a calcaneal osteotomy performed at 19 months after the injury. None of the patients required delayed amputation. Seven (37%) of the 19 patients followed for greater than 1 year required subsequent surgical procedures.
A pure dislocation of the talus, characterized by complete disruption of the ankle, subtalar, and talonavicular joints without concomitant talar fracture, is a rare injury and often referred to as a pantalar dislocation . The mechanism of injury is forced supination or pronation, usually coupled with plantar flexion, causing a medial or lateral subtalar dislocation, combined with a force strong enough to dislocate the ankle.
When these injuries are closed, with no open wounds, they manifest with tense anterior skin, usually on the lateral side secondary to the pressure of the dislocated talus against the soft tissue envelope. Many are associated with fractures of at least some portion of the talus or with fractures of the malleoli, but occasionally no concomitant fracture is present. Closed reduction under anesthesia with or without skeletal traction may be attempted, but if these attempts fail, open reduction should be performed at once. Kenwright and Taylor presented two such cases, with one excellent result as late as 11 years after injury. Results from other series and case reports are also surprisingly satisfactory when infection or AVN does not occur.
When these injuries are associated with an open wound, the talus often has associated fractures but usually still has some soft tissue attachment to the body ( Fig. 46-23 ). A rare subtype of this injury does exist, however, in which the talus is totally extruded or expulsed from the body without an associated fracture and without any remaining soft tissue attachments. Treatment of the open wound should include standard soft tissue debridement according to the principles of Gustilo and others.

These challenging cases provide a dilemma for the treating surgeon. Do these patients benefit from fixation and reimplantation, simple reimplantation, or reimplantation and fusion? Or does the surgeon perform a subtotal talectomy, total talectomy, or a talectomy and fusion?
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here