Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In 2017, the American College of Cardiology/American Heart Association (ACC/AHA) redefined hypertension as a sustained systolic blood pressure above 130 mm Hg and/or a diastolic pressure above 80 mm Hg. This new definition arose in response to the results of the Systolic Blood Pressure Intervention Trial (SPRINT), which found a significantly lower rate of fatal and nonfatal cardiovascular events in nondiabetic hypertensive patients with a systolic blood pressure target of less than 120 mm Hg, as compared to the standard goal of 140 mm Hg. This new definition qualifies over 100 million people in the United States as hypertensive, nearly one-half of all adults, occurring more frequently in non-Hispanic blacks (40.6%) than non-Hispanic whites (29.7%), non-Hispanic Asians (28.7%), and Hispanics (27.3%). The incidence of hypertension increases with age and is more prevalent in men until age 60, after which elevated blood pressure is present in a higher percentage of women than men.
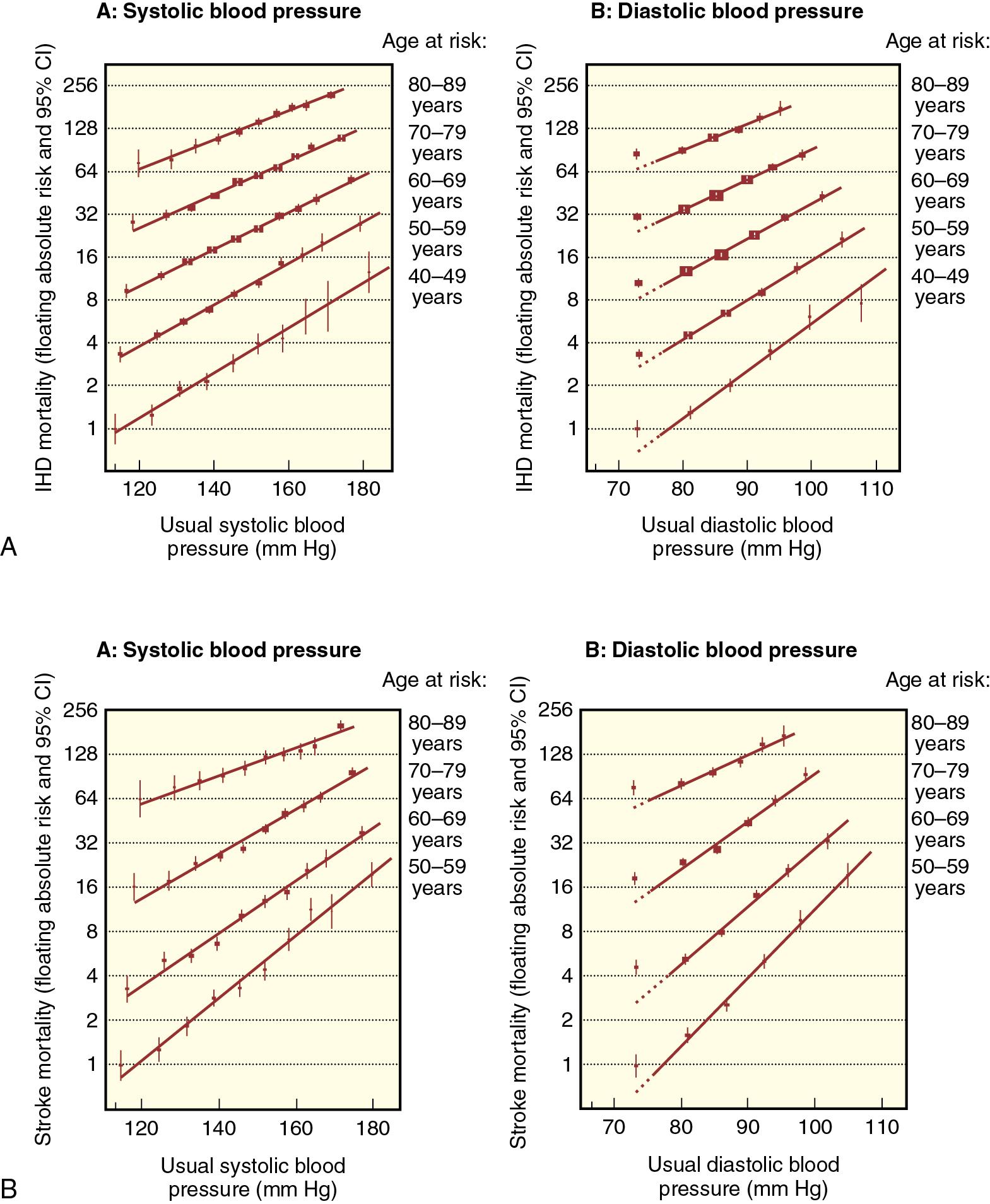
Worldwide, the burden of hypertension disproportionally affects low- and middle-income countries. It is the leading risk factor for morbidity and mortality, accounting for 7% of disability-adjusted life-years and 9.4 million deaths in 2010. It has been estimated that in the United States, the lifetime risk of developing hypertension is close to 90%. The clinical consequences of chronically elevated blood pressure have been well characterized and underscore a high age-related association with ischemic heart disease and stroke ( Fig. 9.1 ), as well as renal failure, retinopathy, peripheral vascular disease, and overall mortality. In the surgical population, multiple studies have found hypertension to be a common risk factor for perioperative morbidity and mortality, particularly with untreated or refractory hypertension. It is not clear, however, if increased blood pressure alone increases surgical risk or if normalization of blood pressure preoperatively significantly reduces these risks. Furthermore, chronic hypertension represents a dynamic spectrum spanning so-called elevated blood pressure to severe disease ( Table 9.1 ), with risk assessment often not clearly differentiating subtypes: isolated systolic hypertension (systolic >130 mm Hg and diastolic <80 mm Hg), isolated diastolic hypertension (systolic <130 mm Hg with diastolic >80 mm Hg), and combined systolic and diastolic hypertension (systolic >130 mm Hg and diastolic >80 mm Hg). As noted in the Eighth Joint National Committee Report on the Treatment of Hypertension (JNC 8), age dependence, risk association, pharmacologic therapy, and treatment goals can vary among subtypes. In addition to systolic and diastolic pressure abnormalities, an increase in their difference—pulse pressure—has been shown to be a risk factor for cardiovascular morbidity. Considered to be an index of vascular remodeling and “stiffness,” some studies have linked increased pulse pressure with intraoperative hemodynamic instability and adverse postoperative outcomes.
| Category | Systolic BP (mm Hg) | Diastolic BP (mm Hg) |
|---|---|---|
| Normal | <120 | <80 |
| Elevated | 120–129 | <80 |
| Stage 1 hypertension | 130–139 | 80–89 |
| Stage 2 hypertension | ≥140 | ≥90 |
Given the physiologic importance and complexity of blood pressure regulation, hypertension can result from a wide range of primary and secondary processes that increase cardiac output, peripheral vascular resistance, or both. The etiology of primary hypertension (also referred to as essential hypertension) is unclear, but contributing factors include sympathetic nervous system activity, dysregulation of the renin-angiotensin-aldosterone system, and deficient production of endogenous vasodilators ( Table 9.2 ). Importantly, blood pressure elevation is often coincident with other morbidities and may occur in a constellation of symptoms associated with oxidative stress and systemic inflammation. There are defined genetic and lifestyle risk factors such as obesity, alcohol consumption, and tobacco use that are associated with an increased incidence of hypertension.
Autonomic Nervous System
|
Classical Renin-Angiotensin-Aldosterone System
|
Endogenous Vasodilator/Vasoconstrictor Balance
|
A small minority of adult patients with elevated blood pressure have secondary hypertension resulting from a potentially correctable physiologic or pharmacologic cause ( Table 9.3 ). The etiology of hypertension is age dependent. In middle-aged adults, hyperaldosteronism, thyroid dysfunction, obstructive sleep apnea, Cushing syndrome, and pheochromocytoma are the most common causes of secondary hypertension. In contrast, the majority of children with elevated blood pressures have secondary hypertension from renal parenchymal disease or coarctation of the aorta (see Table 9.3 ).
| Select Drugs That May Elevate Blood Pressure | ||
| Drug Class | Example | |
| Antiinfective | Ketoconazole | |
| Antiinflammatory | Cyclooxygenase-2 inhibitors, nonsteroidal antiinflammatory drugs | |
| Chemotherapeutic | Vascular endothelial growth factor inhibitors | |
| Herbal | Ephedra, ginseng, ma huang | |
| Illicit | Amphetamines, cocaine | |
| Immunosuppressive agents | Cyclosporine, sirolimus, tacrolimus | |
| Psychiatric | Buspirone, carbamazepine, clozapine, lithium, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, tricyclic antidepressants | |
| Sex hormones | Estrogen and progesterone in oral contraceptives; androgens | |
| Steroid | Methylprednisolone, prednisone | |
| Sympathomimetic | Decongestants, diet pills | |
| Most Common Causes of Secondary Hypertension by Age a | ||
| Age Group | % of Patients With Hypertension With an Underlying Cause | Most Common Etiologies |
| Children (birth–12 yr) | 70–85 | Renal parenchymal disease |
| Coarctation of the aorta | ||
| Adolescents (12–18 yr) | 10–15 | Coarctation of the aorta |
| Young adults (19–39 yr) | 5 | Thyroid dysfunction |
| Fibromuscular dysplasia | ||
| Renal parenchymal disease | ||
| Middle-aged adults (40–64 yr) | 8–12 | Hyperaldosteronism |
| Thyroid dysfunction | ||
| Obstructive sleep apnea | ||
| Cushing syndrome | ||
| Pheochromocytoma | ||
| Older adults (≥65 yr) | 17 | Atherosclerotic renal artery stenosis |
| Renal failure | ||
| Hypothyroidism | ||
a Excluding drug causes and the risk factor of obesity. Listed in approximate order of frequency.
Regardless of the underlying cause, chronic hypertension leads to remodeling of small and large arteries, endothelial dysfunction, and potentially irreversible end-organ damage ( Table 9.4 ). Overall, disseminated vasculopathy plays a major role in ischemic heart disease, left ventricular hypertrophy, congestive heart failure, cerebrovascular disease and stroke, peripheral vascular disease and aortic aneurysm, and nephropathy. The degree to which some abnormalities are reversible is controversial, but early and effective intervention is essential. Improved diagnostic techniques may help provide a more detailed assessment than just blood pressure alone. Ultrasonic measurement of common carotid artery intimal-medial thickness and arterial pulse-wave velocity can provide early diagnosis of vasculopathy, and echocardiographic and electrocardiographic indices may track progression of left ventricular hypertrophy. Early signs of hypertensive nephropathy have become easier to detect, and magnetic resonance imaging (MRI) can be used to follow microangiopathic changes indicative of cerebrovascular damage.
Vasculopathy
|
Cerebrovascular Damage
|
Heart Disease
|
Nephropathy
|
The general therapeutic goal for hypertension treatment is a blood pressure less than 130/80 mm Hg. However, a substantial number of people with hypertension are unable to attain this goal due to nondiagnosis or misdiagnosis, minimal or adverse responses to medications, or noncompliance with prescribed treatment. In fact, approximately 28 million people in the United States alone have untreated hypertension, and a further 29 million patients on an antihypertensive medication are above their blood pressure goal. Resistant hypertension is defined as above-goal blood pressure despite three or more antihypertensive drugs of different classes given at maximally tolerated doses. Controlled resistant hypertension is defined as controlled blood pressure requiring four or more medications. Treatment of resistant hypertension typically includes a long-acting calcium channel blocker (CCB), an angiotensin-converting enzyme (ACE) inhibitor, or an angiotensin receptor blocker (ARB) and a diuretic. Refractory hypertension, defined as uncontrolled blood pressure on five or more drugs, is present in 0.5% of patients. Even more common is intolerance to antihypertensive drugs or pseudoresistant hypertension. Pseudoresistant hypertension can result from blood pressure measurement inaccuracies (including white-coat syndrome) or medication noncompliance. A study of patients with apparent treatment-resistant hypertension who had been prescribed three to five antihypertensive medications revealed that nearly a quarter of the study subjects had no detectable drug in blood or urine samples. It is important to note that currently available blood pressure devices using oscillatory techniques can be highly inaccurate for measuring either systolic or diastolic blood pressure. These devices measure the mean arterial pressure (MAP) more reliably.
Lifestyle modifications of proven value in lowering blood pressure include weight reduction, moderation of alcohol intake, increased aerobic exercise, and smoking cessation. There is a continuous relationship between increased body mass index (BMI) and blood pressure, with waist-to-hip ratio as an even stronger correlate. Weight loss is an effective nonpharmacologic intervention, through direct blood pressure reduction and synergistic enhancement of antihypertensive drug therapy efficacy. Overweight adults should aim for ideal body weight but can expect a 1 mm Hg reduction in blood pressure for every 1 kg of weight loss. Excessive alcohol consumption can be associated with increased hypertension and may cause resistance to antihypertensive drugs. Even modest increases in physical activity are associated with blood pressure decrease.
Dietary potassium and calcium intake is inversely related to both hypertension and cerebrovascular disease in the general population. Salt restriction (e.g., Dietary Approaches to Stop Hypertension [DASH] eating plan) is associated with small but consistent decreases in systemic blood pressure. Sodium restriction may be most beneficial in lowering blood pressure in blacks, older adults, diabetics, or those with metabolic syndrome, patient populations with low renin activity that, in total, constitute nearly half of all adults in the United States. Recent findings challenge previous views on salt restriction and improvement in blood pressure or cardiovascular symptoms.
With continual research regarding the physiology and public health implications of hypertension, as well as identification of new cellular and molecular targets for pharmacologic intervention, treatment guidelines remain fluid. It is clear, however, that optimal drug therapy needs to consider ethnicity, advanced age, comorbidities, and end-organ function. The most recent evidence-based guidelines for the management of high blood pressure in adults (the ACC/AHA guidelines of 2017) outlined several broad conclusions:
Out-of-office blood pressure measurements are recommended for the diagnosis of hypertension and titration of antihypertensive medications.
There is strong evidence to support treating patients with ischemic heart disease, cerebrovascular disease, chronic kidney disease, or with an elevated risk of atherosclerotic cardiovascular disease with blood pressure–lowering medications if systolic blood pressure is 130 mm Hg and above. The recommendation of treating a diastolic blood pressure of 80 mm Hg and above has more limited data but is strongly recommended.
There is limited data to support the ACC/AHA Class I recommendation to treat patients without elevated cardiovascular disease risk or cerebrovascular disease with nonpharmacologic therapy if systolic blood pressure is 130 mm Hg and above or diastolic blood pressure is 80 mm Hg and above (stage 1 hypertension) and with blood pressure–lowering medications if systolic blood pressure is 140 mm Hg and above or diastolic blood pressure is 90 mm Hg and above (stage 2 hypertension).
The same thresholds and goals are recommended for hypertensive adults with diabetes or nondiabetic chronic kidney disease as for the general hypertensive population.
ACE inhibitors, ARBs, CCBs, or thiazide-type diuretics are useful and effective in the nonblack hypertensive population, including those with diabetes.
In black adult hypertensives without heart failure (HF) or chronic kidney disease (CKD), including those with diabetes, there is moderate evidence to support initial antihypertensive therapy with a CCB or thiazide-type diuretic.
There is moderate evidence to support antihypertensive therapy with an ACE inhibitor or ARB in persons with CKD to improve kidney outcomes.
Nonpharmacologic interventions, including weight loss, sodium reduction, potassium supplementation, increased physical activity, and reduced alcohol consumption, are important components to a comprehensive blood pressure management approach.
As noted in the guidelines, first-line antihypertensive therapy consists of diuretics, CCBs, ACE inhibitors, and ARBs. Notably absent from first-line therapy are β blockers, which tend to be reserved for patients with coronary artery disease or tachydysrhythmia, or as a component of multidrug therapy in resistant hypertension. A wide range of antihypertensive drugs are in common use ( Table 9.5 ). A recent review noted that drugs in 15 different classes have been approved for the treatment of hypertension in the United States, many of which are also available in single-pill combinations with other compounds. Importantly, although all the available drugs can reduce blood pressure, their disparate pharmacology is evident in the reported relative risk reduction of hypertension-related events. For example, CCBs may lower the risk of stroke but not HF or mortality, whereas a Cochrane review found that in patients with uncomplicated hypertension, low-dose thiazides reduce mortality and cardiovascular morbidity. Nonetheless, across the range of hypertension etiology and severity, the varying pharmacology of available medications allows for combining drugs with different and potentially beneficial properties in terms of optimizing end-organ function ( Table 9.6 ). Despite the plethora of treatment options already available, the public health burden of hypertension continues to drive research into new pharmacologic targets and therapies, including vaccines and surgical interventions ( Table 9.7 ).
| Class | Generic Name | Usual Dose Range (mg/d) | Notes |
|---|---|---|---|
| Primary Agents | |||
| Thiazide-type diuretics | Chlorthalidone Hydrochlorothiazide Indapamide Metolazone |
12.5–25 25–50 1.25–2.5 2.5–5 |
Monitor sodium, potassium, calcium, and uric acid levels. |
| Angiotensin-converting enzyme (ACE) inhibitors | Benazepril Captopril Enalapril Fosinopril Lisinopril Moexipril Perindopril Quinapril Ramipril Trandolapril |
10–40 12.5–150 5–40 10–40 10–40 7.5–30 4–16 10–80 2.5–20 1–4 |
Do not use in combination with ARBs or a direct renin inhibitor. Avoid in pregnancy. Do not use if history of angioedema. Risk of renal failure with severe bilateral renal artery stenosis. |
| Angiotensin receptor blockers (ARBs) | Azilsartan Candesartan Eprosartan Irbesartan Losartan Olmesartan Telmisartan Valsartan |
40–80 8–32 600–800 150–300 50–100 20–40 20–80 80–320 |
Do not use in combination with ACE inhibitors or a direct renin inhibitor. Avoid in pregnancy. Do not use if history of angioedema. Risk of renal failure with severe bilateral renal artery stenosis. |
| (CCBs): dihydropyridines | Amlodipine Felodipine Isradipine Nicardipine SR Nifedipine LA Nisoldipine Clevidipine (IV) |
2.5–10 2.5–10 5–10 60–120 30–90 17–34 1–32 (mg/hr) |
Avoid in heart failure with reduced ejection fraction (HFrEF). |
| (CCBs): nondihydropyridines | Diltiazem ER Verapamil (IR/SR) Verapamil ER |
120–360 120–360 100–300 |
Avoid routine use with β blockers. |
| Do not use in HFrEF. | |||
| Secondary Agents | |||
| Diuretics: loop | Bumetanide Furosemide Torsemide |
0.5–2 20–80 5–10 |
Preferred in symptomatic HFrEF. Preferred over thiazides with glomerular filtration rate (GFR) <30 mL/min. |
| Diuretics: potassium sparing | Amiloride Triamterene |
5–10 50–100 |
Avoid in patients with GFR <45 mL/min. |
| Diuretics: aldosterone antagonists | Eplerenone Spironolactone |
50–100 25–100 |
Preferred in primary aldosteronism and resistant hypertension. |
| β blockers | Atenolol Betaxolol Bisoprolol Metoprolol tartrate Metoprolol succinate Nadolol Nebivolol Propranolol (IR/LA) |
25–100 5–20 2.5–10 100–200 50–200 40–120 5–40 80–160 |
β blockers not first line unless concomitant ischemic heart disease (IHD) or HF. Bisoprolol and metoprolol succinate are preferred in patients with HFrEF. Avoid nadolol and propranolol in patients with reactive airways disease. Nebivolol also has vasodilatory effects. Avoid abrupt cessation. |
| α 1 blockers | Doxazosin Prazosin Terazosin |
1–16 2–20 1–20 |
Association with orthostatic hypotension. Second-line agents in patients with bronchopleural fistula. |
| Combined α and β blockers | Carvedilol Carvedilol phosphate Labetalol |
12.5–50 20–80 200–800 |
Carvedilol is preferred in patients with HFrEF. |
| Centrally acting | Clonidine oral Clonidine patch Methyldopa |
0.1–0.8 0.1–0.3 250–1000 |
Last-line agents. Significant central nervous system (CNS) adverse effects in older adults. Abrupt discontinuation may induce a hypertensive crisis. |
| Vasodilators | Hydralazine Minoxidil |
100–200 5–100 |
Use with a diuretic and β blocker. Associated with water retention and reflex tachycardia. |
| Direct renin inhibitor | Aliskiren | 150–300 | Do not use with ACE inhibitors or ARBs. Avoid in pregnancy. Do not use if history of angioedema. Risk of renal failure with severe bilateral renal artery stenosis. |
| Subclinical End-Organ Damage | |
| Left ventricular hypertrophy | ACEIs, ARBs, CCBs |
| Elevated albuminuria | ACEIs, ARBs |
| Renal dysfunction | ACEIs, ARBs |
| Irreversible Hypertensive End-Organ Damage | |
| Prior stroke | Any antihypertensive |
| Prior MI | BBs, ACEIs, ARBs |
| Angina pectoris, CHD | BBs, CCBs |
| Heart failure | Diuretics, BBs, ACEIs, ARBs, MR antagonists |
| Left ventricular dysfunction | ACEIs, ARB |
| Atrial fibrillation | |
|
|
|
ARBs, ACEIs, BBs, nondihydropyridine CCBs |
| Tachydysrhythmia | BBs |
| Chronic renal insufficiency, proteinuria | ACEIs, ARBs, loop diuretics |
| Peripheral arterial occlusive disease | CCBs |
| New Drugs Mineralocorticoid receptor antagonists Aldosterone synthase inhibitors Activators of the ACE2/angiotensin-(1–7)/Mas receptor axis Centrally acting aminopeptidase inhibitors Vasopeptidase inhibitors Dual-acting angiotensin receptor–neprilysin inhibitors Dual-acting endothelin-converting enzyme–neprilysin inhibitors Natriuretic peptide receptor agonists Vasoactive intestinal peptide receptor agonist Soluble epoxide hydrolase inhibitors Intestinal Na + /H + exchanger 3 inhibitor Dopamine β-hydroxylase (DβH) inhibitor |
| Vaccines Vaccine against angiotensin II Vaccine against angiotensin II type 1 receptor |
| Novel Approaches to Preeclampsia Treatment Antidigoxin antibody fragment Recombinant antithrombin |
| Interventional Procedures Renal denervation Baroreflex activation therapy Carotid body ablation Arteriovenous fistula creation Neurovascular decompression Renal artery stenting (revascularization) |
Treatment of secondary hypertension is often interventional, including correction of renal artery stenosis via angioplasty or direct arterial repair, and adrenalectomy for adrenal adenoma or pheochromocytoma. For patients in whom renal artery repair is not possible, blood pressure control may be accomplished with ACE inhibitors alone or in combination with diuretics, although ACE inhibitors, ARBs, and direct renin inhibitors are not recommended in patients with severe bilateral renal artery stenosis as they can hasten progression to renal failure. Primary hyperaldosteronism in women can be treated with an aldosterone antagonist such as spironolactone, whereas amiloride is often used in men owing to the potential for spironolactone-induced gynecomastia. Certain disease entities, such as pheochromocytoma, require a combined pharmacologic and surgical approach for optimal outcome.
Assessment of blood pressure in the preoperative area or clinic is often complicated by an anxiety-related hypertensive response (white-coat hypertension). Furthermore, patients are often instructed to interrupt prescribed antihypertensives, such as ACE inhibitors and diuretics, on the day of surgery. Assessing blood pressure in a single moment in time does not give an accurate picture of overall blood pressure optimization and, according to current guidelines, multiple elevated blood pressure readings over time are necessary for a diagnosis of hypertension. Firstly, appropriate blood pressure technique should be confirmed, and, if still elevated, a pressure on the contralateral arm should be obtained. A careful review of prior clinic data, home blood pressure readings, and a thorough patient history are necessary to gain a better overall picture of cardiovascular health. Therefore, in general, elevated blood pressure per se is not a direct prompt to delay surgery in asymptomatic patients without other risk factors. In fact, unless there is marked hypertension (systolic >180 mm Hg and/or diastolic >110 mm Hg) or end-organ injury that can be ameliorated by aggressive blood pressure control, delaying surgery is not generally recommended.
While secondary hypertension is rare, suspicion of such should prompt a workup. A secondary etiology may be indicated by symptoms (e.g., flushing, sweating, palpitations suggestive of pheochromocytoma), physical examination (e.g., a renal bruit suggestive of renal artery stenosis), laboratory abnormalities (e.g., hypokalemia suggestive of hyperaldosteronism), or age (most hypertension in children <12 years of age is secondary). These patients often present as severely hypertensive with no prior diagnosis of hypertension, and they would be exception to the “no delay” approach to preoperative hypertension. In fact, there have been multiple reports of a pheochromocytoma being “diagnosed” by induction of general anesthesia for an incidental procedure.
Once the decision is made to proceed with surgery, it is now common practice to continue antihypertensive medications, with the possible exception of high-dose ARBs and ACE inhibitors. Some authors advocate discontinuing these drugs at least 10 hours prior to surgery owing to concerns about refractory hypotension. In contrast, others believe there is little direct association between chronic use of ARBs and ACE inhibitors and sustained hypotension and therefore support continuing these drugs up to the time of surgery, especially in ambulatory patients. In addition, cessation of β-adrenergic antagonists or clonidine can be associated with rebound effects. Interruption of CCBs is associated with increased perioperative cardiovascular events.
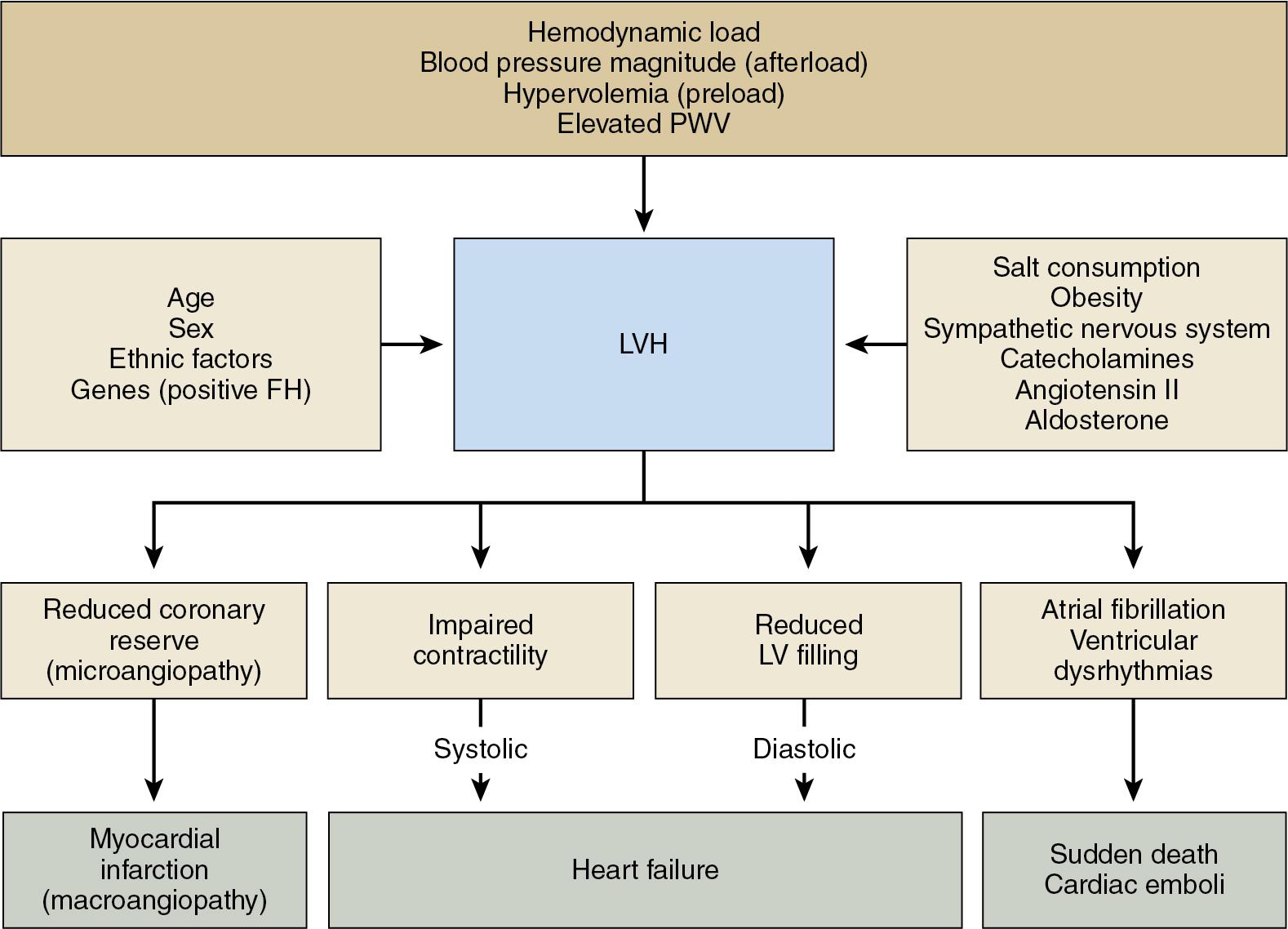
Although guidelines do not support delaying surgery for poorly controlled blood pressure, perioperative hypertension increases blood loss as well as the incidence of myocardial ischemia and cerebrovascular events. Furthermore, owing to a combination of physiologic factors (volume depletion, loss of vascular elasticity, baroreceptor desensitization) in combination with antihypertensive treatment, hypertensive patients are prone to intraoperative hemodynamic volatility. When superimposed on organ damage from chronic hypertensive disease, even brief periods of hypotension are associated with acute kidney injury, myocardial injury, and death. Ultimately, regardless of treatment efficacy at the time of surgery, hypertension as a disease entity has long been known to be an independent predictor for adverse perioperative cardiovascular events, especially when combined with other risk factors. Accordingly, clinicians need to consider acute intraoperative changes in blood pressure in the context of alterations in end-organ functional reserve brought about by chronic disease. Particular emphasis has been placed upon ischemic heart disease and the implications of left ventricular hypertrophy on cardiac relaxation and filling during diastole ( Fig. 9.2 ). Nevertheless, guidelines for optimal systolic and diastolic blood pressures and MAP are lacking and impossible to derive, as blood pressure itself provides little guidance about microvascular blood flow and resistance.
As already noted, hypertensive patients can be hemodynamically volatile, with induction of anesthesia producing hypotension and subsequent laryngoscopy and tracheal intubation eliciting hypertension and tachycardia. To lessen this risk it has been suggested that placement of an intraarterial catheter followed by a multimodal induction that includes transient β blockade with esmolol may be beneficial. Poorly controlled hypertension is often accompanied by relative volume depletion, especially if a diuretic is part of chronic therapy. In some patients, modest volume loading prior to induction of anesthesia may provide hemodynamic stability, although this approach may be counterproductive in patients with marked left ventricular hypertrophy and significant diastolic dysfunction.
As with any procedure, a management plan for hemodynamic monitoring and vasoactive drug therapy for hypertensive patients should consider age, functional reserve, preoperative pharmacotherapy, and the planned operation. For example, intention-to-treat thresholds for patients undergoing repair of aortic dissection or women with peripartum hypertension will be lower than for the general surgical population. While arterial catheterization provides useful continuous information, the decision to use invasive monitoring is typically reserved for select patients based on magnitude of surgery, severity of disease, functional capacity, and comorbidities. Assessment of fluid status can be challenging in patients with long-standing hypertension, especially those with a history of heart failure with preserved ejection fraction (HFpEF). Left ventricular hypertrophy reduces chamber compliance such that with volume infusion, right heart pressures rise despite the fact that the left ventricle is relatively underfilled. Ultimately, intraoperative use of a pulmonary artery catheter is controversial, and pressure measurements from a central venous catheter may not provide a clear representation of volume status. Overall, echocardiographic evaluation of cardiac volumes may be the most useful in patients with HFpEF, but this has its own inherent risks and requires specialized personnel.
Achieving hemodynamic stability may be more important than targeting an arbitrary intraoperative blood pressure, especially given the influence of other comorbidities, surgical procedure and position, volume status, mechanical ventilation, and depth of anesthesia. The management of intraoperative blood pressure over the wide range of potential clinical scenarios is beyond the scope of this review. However, it is important to consider that although high-dose anesthetics can acutely control blood pressure in many patients, this approach can have side effects, slows emergence, and cannot be continued into the postoperative phase. Accordingly, addition of sympathomodulators (esmolol, metoprolol, labetalol) or titrated calcium channel blocker therapy (nicardipine or clevidipine) can facilitate transition from the operating room to postanesthesia care unit (PACU) or intensive care unit (ICU).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here