Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Idiopathic intracranial hypertension (IIH) is a disorder characterized by symptoms secondary to increased intracranial pressure (ICP) with no clear identifiable cause. It is therefore a diagnosis of exclusion and necessitates the exclusion of differential diagnoses of increased ICP (i.e., intracranial mass, blockage of the ventricular system, blockage of cerebrospinal fluid [CSF] absorption, communicating hydrocephalus, obstruction of venous outflow, diffuse cerebral edema, and increased CSF secretion). The cause of IHH remains unclear. Hypothetical mechanisms include increased CSF production (secondary to abnormal function of the ependymal cells in the choroid plexus), decreased CSF absorption (secondary to the obstruction of cortical venous sinuses, and increased venous sinus pressure. Contributing factors include obesity, which leads to hormonal changes and increased intraabdominal, pleural, cardiac filling, and central venous pressures, leading to increased ICP.
Idiopathic intracranial hypertension affects 0.5 to 2 people per 100,000 of the general population, but it is significantly more prevalent in obese women of reproductive age. The ongoing worldwide obesity epidemic has increased the incidence of IIH and its impact on patients and society. Visual impairment and headaches are the most common symptoms associated with IIH. Visual deficits are secondary to the progressive atrophy of the optic disc, which is due to papilledema caused by elevated ICP, first leading to transient visual loss and visual field defects and declining color vision and diminished visual acuity. Additional symptoms include pulsatile tinnitus, back and neck pain, olfactory changes, encephaloceles, CSF leaks, and cognitive and mood changes. The clinical presentation is variable, which may lead to delays in diagnosis and management. , , In addition to its direct impact on patients and families, IIH is also associated with increased costs. In the United States, the total hospital costs per IIH admission were four times greater than for a population-based per person admission, and the total economic costs of IIH were greater than $444 million per year ( Table 17.2 ).
| Surgical Treatment | Approximate Estimated Cost ($) |
|---|---|
| LP shunt | 2716 or 4227 (programmable valve) |
| VP shunt | 4698 |
| ONSF | 873 |
| Venous stenting | 4690 |
| Laparoscopic adjustable gastric banding | 5348 |
| Laparoscopic Roux-en-Y gastric bypass | 9608 |
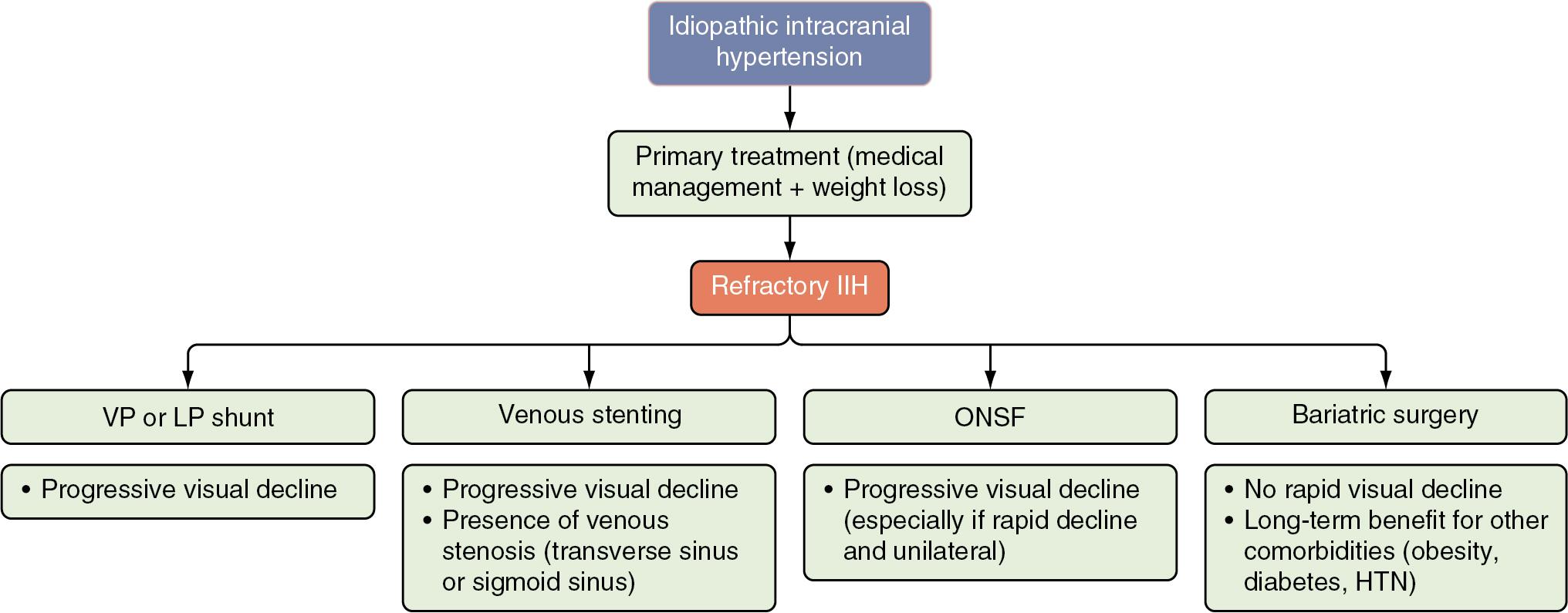
The main goals of treatment are to preserve visual function and alleviate associated symptoms. Primary treatment consists of weight reduction and medical therapy with acetazolamide, topiramate, or both. Patients who do not respond to medical therapy and present with progressive visual decline should be considered for surgical intervention. Multiple surgical approaches are available for the management of IIH, including CSF shunting, venous stenting, optic nerve sheath fenestration (ONSF), and bariatric surgery. These options have different responses and complication rates and are selected according to the patient’s symptoms, anatomic features, and preferences, combined with the treating team’s experience ( Fig. 17.1 and and Table 17.1 ). ,
| Surgical Treatment | Female | Mean Age (range) | Obese | First Surgery Performed | Outcomes (%) | Complications (Severe) (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Improved Visual Field (Worsened) | Improved Visual Acuity (Worsened) | Improved Headache (Worsened) | Improved Papilledema (Worsened) | Failure Rate | Restored CSF Pressure | ||||||
| CSF diversion | 88 | 32.68 (4–68) | 72.7 | 89.5 | 66.8 (5.8) | 55 (13.1) | 69.8 (0) | 78.9 (7) | 43.4 | 100 | 9.4 |
| ONSF | 83.3 | 31.9 (14–74) | 85.7 | 82.5 | 65.2 (5.5) | 44.1 (7.4) | 49.3 (0) | 90.5 (1.2) | 9.5 | 50 | 2.2 |
| Venous stenting | 81.8 | 36.7 (10–66) | 63.6 | 83.7 | 72.7 (5.1) | 64.6 (6.1) | 72.1 (.6) | 87.1 (.4) | 11.3 (2.6, revision) | 92.75 | 2.3 |
| Bariatric surgery | 100 | 34.1 (15–53) | 100 | 72.9 | 83.3 | 100 | 93.3 (0) | 100 | 10.8 | 100 | 29.4 |
This chapter reviews the surgical interventions currently available for the management of refractory IIH in the context of the current understanding of the pathophysiology of IIH, including the role of venous system obstruction.
The pathophysiology of elevated ICP in IHH has not been fully elucidated. Several theories have been suggested, most of them centering on increased CSF production, decreased CSF absorption, increased venous sinus pressure, and other factors such as obesity that may influence these mechanisms.
Approximately 600 mL of CSF is produced daily. This value decreases with increasing age, which may explain why IIH is a disorder of younger people. CSF is produced in the choroid plexus, located in the cerebral ventricles, by a lining of specialized epithelial tissue known as ependyma. This CSF production mechanism involves the action of Na + /K + -ATPase channels, which results in other electrolytes (e.g., K + , Cl – , HCO3 – ) following the electrochemical gradient. This leads to a large amount of H 2 O crossing the epithelium via aquaporin-1 channels. Carbonic anhydrase produces protons and bicarbonate used by the transporters and is inhibited by acetazolamide, one of the medical treatments for IIH. CSF flows out of the ventricular system through arachnoid granulations (with microscopic villi) because of pressure difference between CSF space and venous sinuses where it is resorbed.
Obesity is linked to a prothrombotic state via increased plasminogen activator inhibitor activity and therefore an increase the likelihood of obstruction in the cerebral venous sinus and consequently increases in CSF pressure. Additionally, obesity may also lead to decreased venous return and contribute to a decrease in the rate of CSF reabsorption. , ,
The observation that patients with IIH frequently have compression or stenosis of the transverse and sigmoid sinuses supports a potential role of the cerebral venous system in the primary and secondary mechanisms related to IIH. The proposed physiologic relationship between dural sinus stenosis and IIH is impaired venous drainage. Increased venous pressure gradients have been observed in this population, associated with dural venous system stenosis (DVSS) in the transverse and sigmoid sinuses, leading to decreased CSF absorption in arachnoid granulations. DVSS has been reported in the majority of the IIH patients in recent studies. ,
Aplastic or hypoplastic venous sinuses, intrinsic and extrinsic compression, and acquired stenosis likely raise CSF pressure. Bilateral transverse sinus stenosis results in more significant changes in CSF pressure than unilateral stenosis. It is important to mention, however, that there is evidence that stenosis of the sinuses may be secondary to intracranial hypertension rather than the cause of IIH itself. ICP reduction after lumbar puncture and, consequently, improvement in CSF dynamics and reduced flattening of the cerebral venous sinuses, may explain the improvement in patients who undergo venous stenting.
Surgery is recommended for medically refractory IIH, presenting with papilledema or progressive visual deficits. , Current recommendations regarding the selection of surgical approach are mostly based on retrospective single center studies and systematic reviews of these studies; therefore, the current level of evidence is low. CSF shunts (i.e., CSF diversion) are traditionally recommended for patients with IIH and progressive visual decline despite medical therapy and in those who present with rapid visual decline (<4 weeks). Lumbar drains may be considered in the short term as a temporizing measure while surgical planning occurs.
Cerebrospinal fluid diversion is one of the classic surgical approaches for the management of IIH. Ventriculoperitoneal (VP) shunt currently represents the preferential technique for CSF diversion considering its lower revision rate compared with lumboperitoneal (LP) shunts and the possibility of adjustable drainage of CSF, with use of programmable valves. , On the other hand, LP shunt remains a useful option. It does not require the transgression of cerebral parenchyma for insertion of the proximal catheter and easier access to the CSF, especially in the case of patients with slit ventricles.
Although CSF diversion does not reliably reduce headache symptoms in the long term, it does improve short-term symptoms in the majority of patients. The use of programmable valves, which allow differential drainage of CSF based on ICP and headache symptoms, allow for adjustment of drainage based on clinical status. Antisiphon devices allow the pressure in the shunt system to adjust to orthostatic variations in CSF flow. Selection of valves and shunts should be performed on a patient-by-patient basis, and management should be performed by neurosurgeons with experience in the management of patients with IIH.
In a 2021 systematic review of studies on adult patients with IIH, CSF diversion techniques improved papilledema, visual field deterioration, and headaches in 78.9%, 66.8%, and 69.8% of the cases, respectively. However, most of the available evidence on CSF diversion in IIH is retrospective in nature. The major benefit of surgical intervention is arresting the progression of visual decline, and, in fact, CSF diversion can exacerbate headaches via CSF over drainage. Most of the headache relief conferred by CSF diversion has been considered to be short term. Risk factors for treatment failure include papilledema and long-standing symptoms. As a long-term intervention, CSF diversion should ideally be used in tandem with lifestyle interventions, and improved short-term symptoms may result in enough functional improvement to permit weight loss and increased activity. Long-term management of IIH-related headache often requires specialized pain assessment and drug selection according to the characteristics of the specific characteristics of headache (e.g., migraine-like or tension headache like).
Significant differences in functional outcomes between VP and LP shunts have not been demonstrated. However, there is evidence that VP shunts are associated with fewer complications and have a lower failure rate. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here