Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
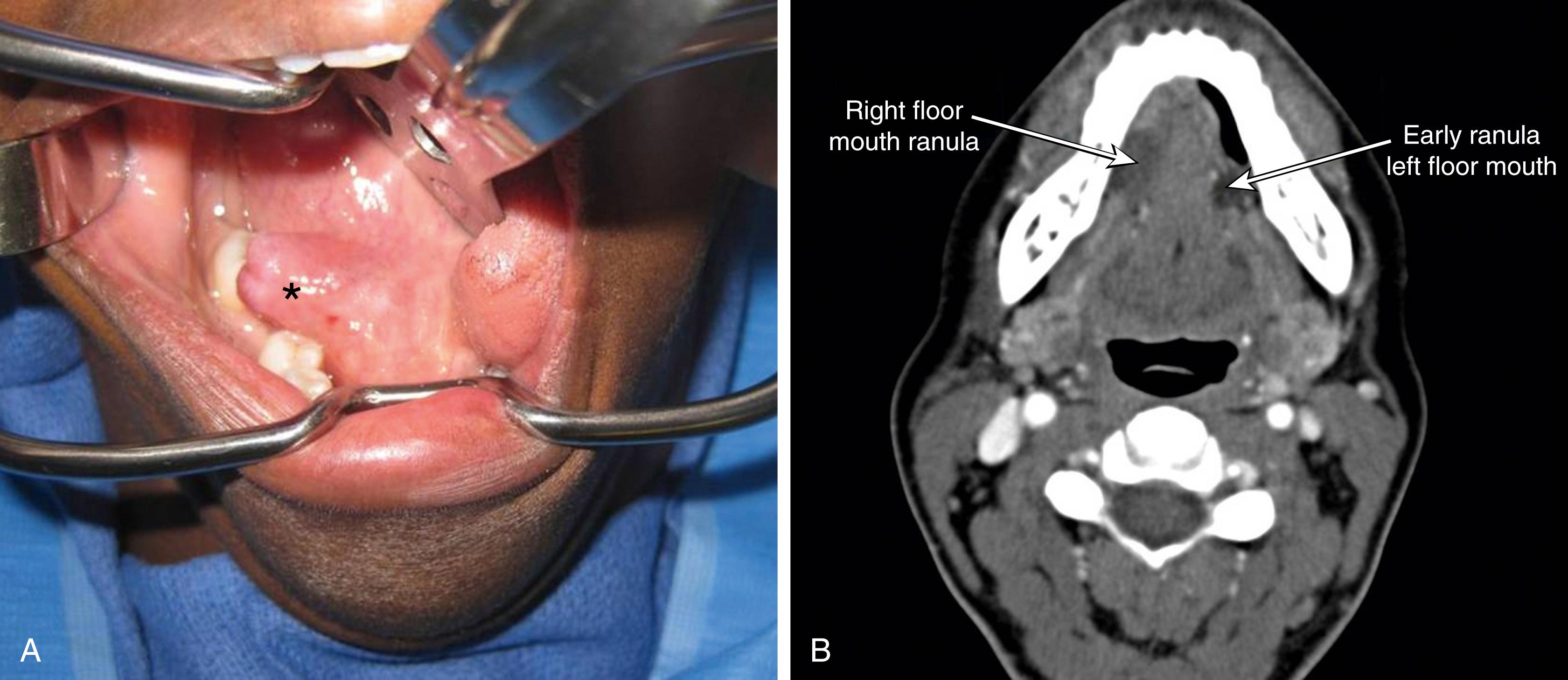
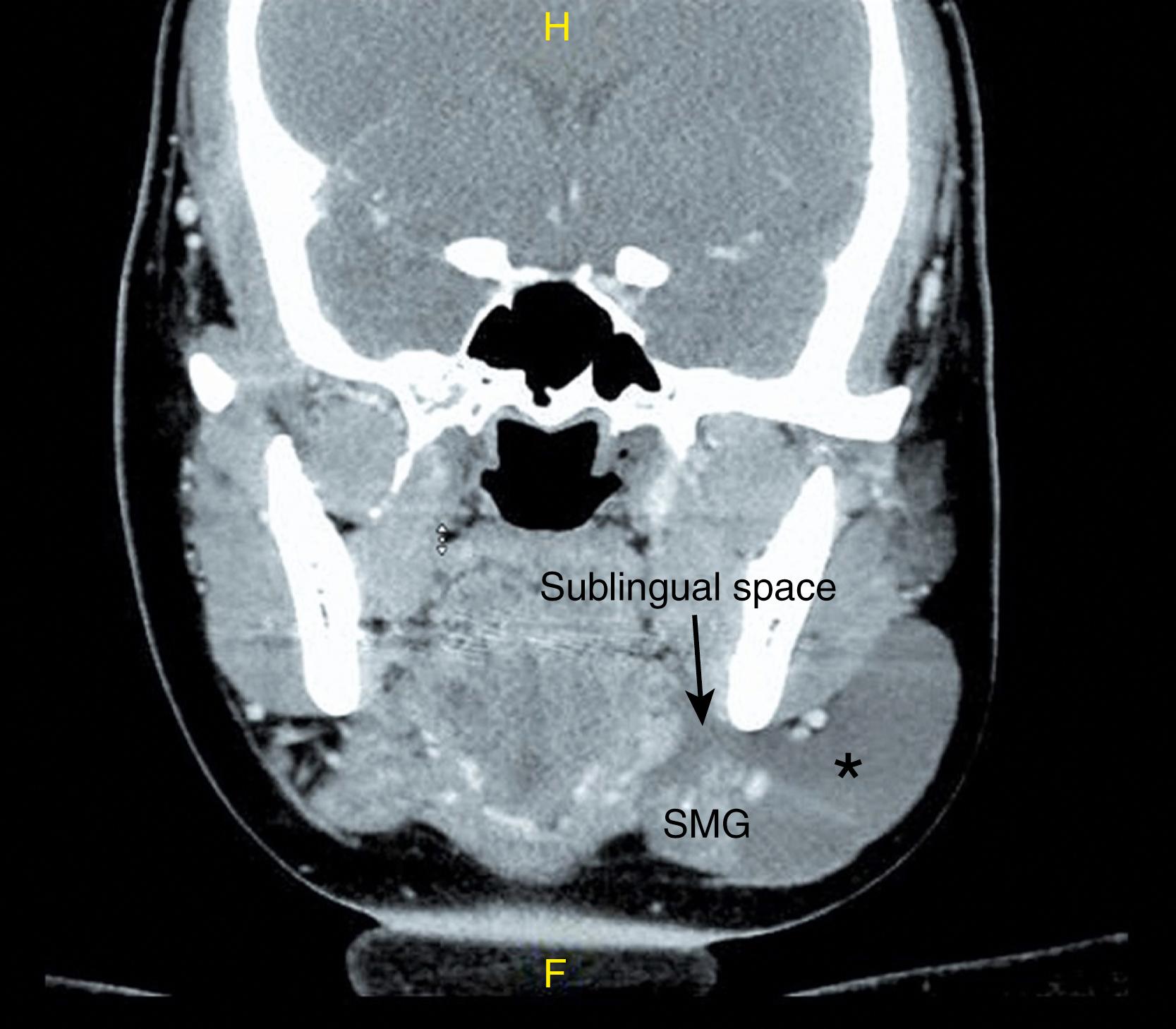
A ranula is an extravasation mucocele that arises in the floor of mouth secondary to trauma to the sublingual gland or obstruction of the salivary ducts. The term ranula is derived from the Latin word rana , meaning frog, which describes the bluish floor of mouth swelling that resembles a frog’s underbelly. These lesions are classified into two types: oral or simple ranulas and cervical or “plunging” ranulas. Oral cavity ranulas present only in the floor of mouth and are located above the mylohyoid sling, while the plunging ranula presents as swelling in the neck and arises from herniation of the ranula through or around the mylohyoid muscle ( Figs. 89.1 and 89.2 ). Plunging ranulas are pseudocysts, meaning that the wall of the ranula is lined with granulation or connective tissue and lacks an epithelial lining.
While surgical therapy is the recommended treatment modality for both oral and plunging ranulas, the preferred approach has evolved over the years. Various methods have been described, including marsupialization and excision of the ranula with or without excision of the sublingual gland for oral ranulas. Others have described a transcervical approach and excision of the submandibular gland in the management of a plunging ranula. More recent literature supports the excision of the sublingual gland with transoral drainage of the plunging component as the modality with the fewest complications and recurrences.
A comprehensive knowledge of anatomy of the sublingual gland is essential to avoid injury to the lingual nerve and Wharton’s duct.
Surgical management of plunging ranulas has shifted from combined approaches with excision of transcervical ranula, and sometimes excision of the submandibular gland, to intraoral excision of the sublingual gland with evacuation of the ranula.
Complete excision of the sublingual gland is associated with the fewest recurrences of ranulas.
History of present illness
Painless swelling of the floor of the mouth
History of recurring lesions with formation of cysts with resolution being pathognomonic of a ranula.
Larger lesions can lead to difficulty with speech, swallowing, and breathing.
Mass effect can cause impairment of submandibular salivary flow, leading to swelling and pain in the gland after eating.
Plunging ranulas present with an enlarging, painless mass in the neck, with or without accompanying swelling of the floor of the mouth.
Past medical history
Trauma to the floor of the mouth or neck
History of surgical procedures to the floor of the mouth or salivary glands
Family history
Bleeding disorders
Medical illness
Medical comorbidities that may impact eligibility for or viability of surgical intervention
Medications
History of anticoagulant therapy or the use of herbal products
Allergies
Antibiotics
Local anesthetics
Oral cavity
Unilateral bluish mass beneath the mucosa of the anterior floor of the mouth
If large, the lesion may cross the midline.
Bimanual palpation of the floor of the mouth must be performed to rule out coincidental salivary calculi. In the case of a plunging ranula, external pressure on the neck mass often makes the corresponding sublingual fossa prominent.
An effort must be made to identify and check the function of the submandibular duct. Location of the papilla of the submandibular duct must be recorded. These steps facilitate cannulation of the submandibular duct if placement of a stent is considered and also facilitates early decision making to perform a marsupialization of the submandibular duct if the submandibular papilla is stenotic.
Patency of all four salivary ducts must be examined and documented
Neck
Fluctuant, nontender, unilateral mass in the submandibular region
Giant ranulas can extend to also involve parapharyngeal space or to the level of the clavicles.
Can have neck mass without oral cavity component
Computerized tomography (CT) scan of neck with contrast and without contrast, 1 mm cuts
Essential in cases of plunging ranula to determine cervical extent and relationships prior to operative management
Appears as a nonenhancing, homogeneous, unilocular lesion in the sublingual space with extension to the submandibular and sometimes the parapharyngeal spaces in plunging ranulas (see Fig. 89.2 )
Sublingual gland or space may be replaced by radiolucent material suggestive of extravasated saliva, typical of ranula formation. The submandibular gland is often displaced or surrounded by the radiolucency making it difficult at times to decipher if the gland is the origin of the pathology or is being affected as a consequence of it.
Magnetic resonance imaging (MRI)
Not required, can complement or replace CT scan
Hyperintense cystic lesion on T2-weighted images, low to intermediate intensity on T1-weighted images
Ultrasonography
Ultrasound has also been shown to successfully evaluate cystic lesions in the submandibular space, as well as evaluate areas of dehiscence in the mylohyoid muscle.
Ultrasound can be a valuable tool intraoperatively as well as to ensure complete drainage of the plunging component of the ranula.
Laboratory tests
Serum amylase: The diagnosis of a ranula is a clinical and radiological diagnosis; however, in cases where there is a question regarding the origin of the cyst, a raised serum amylase level in cyst aspirate can confirm salivary origin.
Ranulas causing airway obstruction or compromise require immediate treatment with either incision and drainage or excision.
Recurrent ranula with infection
Partial obstruction of Wharton’s duct with obstructive sialadenitis
Interference with speech and articulation
Asymptomatic patients who want to avoid progression to the above
Cosmesis
Patient with medical comorbidities precluding administration of general anesthesia
Active infection is considered a relative contraindication.
Evaluation by
Head and neck surgeon
Anesthesiology
A coordinated effort is important to plan the management of the airway for large obstructing ranulas that may distort the anatomy or make for a difficult airway.
If there is a concern, an awake fiberoptic oral or nasal intubation is preferred. Use of video laryngoscopes are also advocated for better visualization.
Discontinue antiplatelet drugs if possible 5 to 7 day prior to surgery.
Preoperative imaging
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here