Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patients with cirrhosis are at highest risk of developing hepatocellular carcinoma (HCC) and screening with sonography every 6 months is recommended.
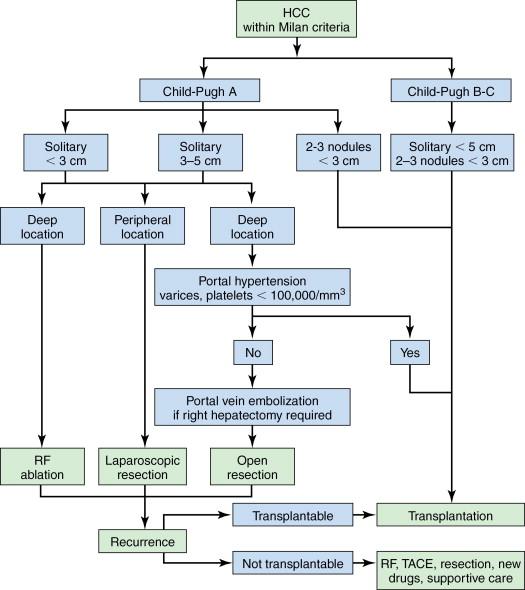
Early-stage HCC should be treated by resection, liver transplantation, or ablation. The best modality depends on tumor size and location, number of tumors, liver function status, future liver remnant, organ availability, as well as patient’s fitness for surgery.
Curative anatomic liver resection is the optimal treatment for HCC in noncirrhotic patients and in selected patients with Child-Pugh Class A cirrhosis, with small solitary tumors. Laparoscopic liver resection has benefits in selected cases.
Patients who are not suitable for resection and meeting the Milan criteria should be considered for liver transplantation (living or cadaveric). Bridge therapy with locoregional treatments should be utilized during transplant evaluation and waiting time.
Patients who are not surgical candidates should be treated with loco-regional approaches such as ablation and transarterial therapies. Transarterial therapies include bland embolization, chemoembolization, and radioembolization.
Inoperable patients may be offered systemic treatment with antiangiogenic drugs, such as sorafenib. The role of systemic treatment in an adjuvant setting remains to be determined. Inclusion in trials of new drugs should be encouraged.
Because of multiple treatment options, multidisciplinary team/conference is the indispensable platform for best comprehensive care.
Hepatocellular carcinoma (HCC) is the most common primary malignancy of the liver. Surgical management of this deadly cancer remains a challenge for all involved in the care of patients diagnosed with it. It is the second most common cause of cancer-related death in the world in men and sixth in women. , The mortality per year in HCC is close to its incidence worldwide, emphasizing the high fatality rate of this aggressive disease. Liver cirrhosis, irrespective of the etiology, is an established major risk factor for HCC. Chronic hepatitis B and C are recognized as the main risk factors for HCC, with risk being escalated in the presence of coinfection with hepatitis B virus (HBV) and hepatitis C virus (HCV).
The Barcelona Clinic Liver Cancer (BCLC) classification is one of the widely used and accepted classification; it stratifies patients according to outcome, avoids the use of a single scoring system for all patients, and simultaneously links it with treatment strategy ( Figure 7-1 ). The BCLC classification is constructed in the setting of cohort and randomized controlled studies; it has also been validated in different settings and establishes treatment recommendations for all stages of HCC. , Patients with early-stage HCC are treated by resection, liver transplantation, or ablation, and prognosis can be refined for all these procedures according to different variables. It considers variables related to tumor size, liver function status, physical status, as well as cancer-related symptoms.
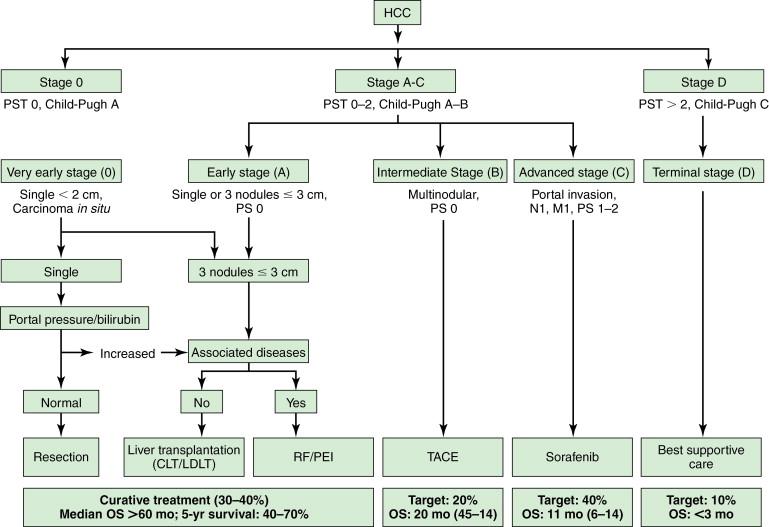
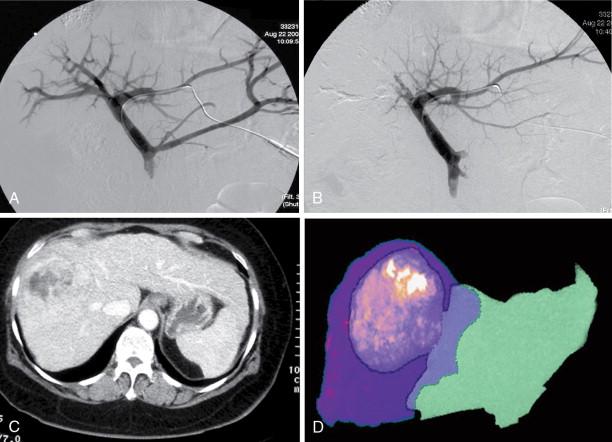
Surgery, including surgical resection and liver transplantation, is currently the mainstay and treatment of choice for HCC. In general, the principles of surgery for HCC after the patient is evaluated to be medically fit for general anesthesia and major surgery are as follows. Liver resection is indicated as a potentially curative procedure if the patient has an adequate liver function (generally Child-Pugh Class A without portal hypertension) and the tumor is resectable with an adequate future liver remnant of at least 20% in a noncirrhotic liver or at least 30%–40% in patients with Child-Pugh Class A cirrhosis. For patients with chronic liver cirrhosis being considered for major resection, preoperative portal vein embolization (PVE) should be considered as an option to induce hypertrophy in the future liver remnant, to minimize risk of postoperative liver failure ( Figure 7-2 ). Patients with HCC meeting the United Network for Organ Sharing (UNOS) criteria should be considered for liver transplantation (living or cadaveric). Situations that are beyond these criteria are controversial (e.g., resectable multifocal disease, patients with resectable tumors who are Child-Pugh Class A within the UNOS criteria) such that a multidisciplinary tumor board should be the platform for decision making.
Patients who are not candidates for potential cure or not medically suitable for major surgery, should be treated with loco-regional approaches. These are broadly classified into ablation techniques and transarterial embolization. Systemic chemotherapy should only be recommended to patients with unresectable HCC in a context of a clinical trial. There are modest but promising results in phases III trials using sorafenib (Nexavar) in both the Western and Asia Pacific regions when compared to best supportive care. , The details of loco-regional treatment and systemic treatment for advanced HCC are beyond the context of this chapter, and only surgical management will be discussed.
A general approach to treatment of HCC within Milan criteria is shown in Figure 7-3 . Our suggested approach is one example and is useful for conceptualizing the various treatment options that are available for individual patients but not negating the importance of a multidisciplinary HCC tumor board decision. Attempts to generate algorithmic approaches to the treatment of HCC are difficult because new treatments and indications for various treatments are evolving rapidly. A discussion of these issues and an overview of surgical therapies for HCC are summarized.
Considering the complexity of the disease and the armamentarium of treatment options available, a multidisciplinary team should be the platform for all decision making in patients with HCC. The multidisciplinary HCC team should be inclusive of hepatobiliary/liver transplant surgeons, hepatologists/gastroenterologists, medical oncologists, dedicated liver radiologists, interventional radiologists and pathologists, and all relevant allied health care professionals. The team should meet regularly at a tumor board and liver transplant meeting with a review of the patients’ clinical status, radiologic images for surgical planning, and histopathology if available, after which an individualized treatment plan is decided by consensus. The meeting also provides an opportunity for the multidisciplinary HCC team to periodically review the latest relevant literature for an evidence-based management. Recommendations may be adapted to local regulations, team’s experience and ability as well as consideration of balancing cost and benefits.
Patient assessment is key in the selection of candidates for liver resection or liver transplantation. As HCCs often present at a late stage, surgical resectability is a primary concern. Once it has been established that curative resection is indicated, resectability can be determined by various factors, including patient, disease, and technical factors. General patient factors include assessment of comorbidities for medical fitness for general anesthesia and major surgery. Specific patient and disease factors determined from two aspects: anatomic feasibility and volumetric tolerance. The main principle lies in the technical ability to leave a liver remnant with adequate function for sustaining life but consistent with low perioperative morbidity and mortality, acceptable long-term outcome in survival, and good quality of life. Relative contraindications to partial hepatectomy include significant medical comorbidities and/or extrahepatic disease. The golden rule for partial hepatectomy is to ensure enough liver parenchyma with a satisfactory blood supply (hepatic artery, portal vein, and hepatic vein), and biliary drainage remains after resection so that the patient does not develop postoperative liver failure. Contraindications of liver resection are situations in which the tumors have invaded the biliary confluence or invaded the three hepatic veins or the portal bifurcation. Any scenario in which bilioenteric anastomosis to the remaining bile ducts cannot be constructed is also considered as a relative contraindication to resection. A multidisciplinary team approach is recommended to validate the decision.
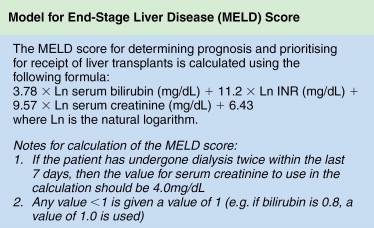
The ability of the nonpathologic liver to regenerate after liver resection is good and a remnant functional normal liver tissue as little as 20% to 25% may be sufficient. , The ratio of remnant functional liver to the initial total liver tissue may be difficult to estimate because of the size of the tumor or number of tumors (e.g., satellite nodules); the volume of these tumors should be excluded when determining the volume of the total liver. There are studies that utilize volumetric ratio without considering the total liver volume, but uses the percentage of total body weight instead. It has been shown that there is a risk of postoperative liver failure when the remaining functional liver ratio falls to less than 0.5% of total body weight. Computed tomography (CT) of the liver is usually applied to measure liver volumes. Most surgeons will not advocate resection if the estimated volume of functional remnant liver is either less than 20%–25% of the total liver volume or less than 0.5% of total body weight. In the West, many centers rely mainly on the Child-Pugh classification ( Table 7-1 ), but as a single assessment, it has significant variations and may underestimate the degree of cirrhosis. As a result, some centers include the clinical signs and radiologic evidence of portal hypertension to guide risk, and a study has shown that hepatic vein pressure of more than 10 mm Hg is a predictor of postoperative liver decompensation. Model for End-stage Liver Disease (MELD) is a prospectively developed and validated chronic liver disease severity scoring system that uses a patient’s laboratory values for serum bilirubin, serum creatinine, and the international normalized ratio for prothrombin time (INR) to predict survival ( Figure 7-4 ). It has been universally adopted by UNOS in 2002 and many parts of the world as a prioritizing tool for liver transplantation. Other than Child-Pugh scoring, MELD and liver function test, some studies have validated the use of indocyanine green clearance (ICG) as an objective adjunct in assessing liver function; in Asia, some institutions use ICG selectively for patient with tumors that are borderline resectable. In patients with “borderline resectability,” one safer option is to induce hypertrophy in the remaining functional liver via PVE to reduce the risk of postoperative liver failure. Compensatory hypertrophy of the contralateral lobe is generally observed in a period of 3–6 weeks (see Figure 7-2 ). Some studies report a high feasibility rate for this strategy and report a mean gain in liver volume of more than 40%, thus increasing the volumetric feasibility for liver resection.
| 1 Point | 2 Points | 3 Points | |
|---|---|---|---|
| Albumin (g/L) | >35 | 28–35 | <28 |
| Bilirubin (μmol/L) | <34 | 34–50 | >50 |
| INR | <1.7 | 1.71–2.20 | >2.20 |
| Ascites | None | Slight | Moderate |
| Encephalopathy | None | Grade 1–2 | Grade 3–4 |
| Points | Class | 1-y Survival | 2-y Survival |
| 5–6 | A | 100% | 85% |
| 7–9 | B | 81% | 57% |
| 10–15 | C | 45% | 35% |
Patients with significant comorbidities should be reviewed by the anesthetic team for evaluation of preoperative risk factors related to general health status (American Society of Anesthesiologists [ASA] score) or associated significant comorbidities to optimize preoperative status.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here