Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Posterior
Midline
Anterior
Transoral approach
Extra/lateral/retropharyngeal approaches
Anterolateral (Smith-Robinson) approach
Posterior occipital prominence : Inion (external occipital protuberance)
First palpable spinous process : C2 spinous process
Most prominent spinous process at cervicothoracic junction : Vertebra prominens (C7)
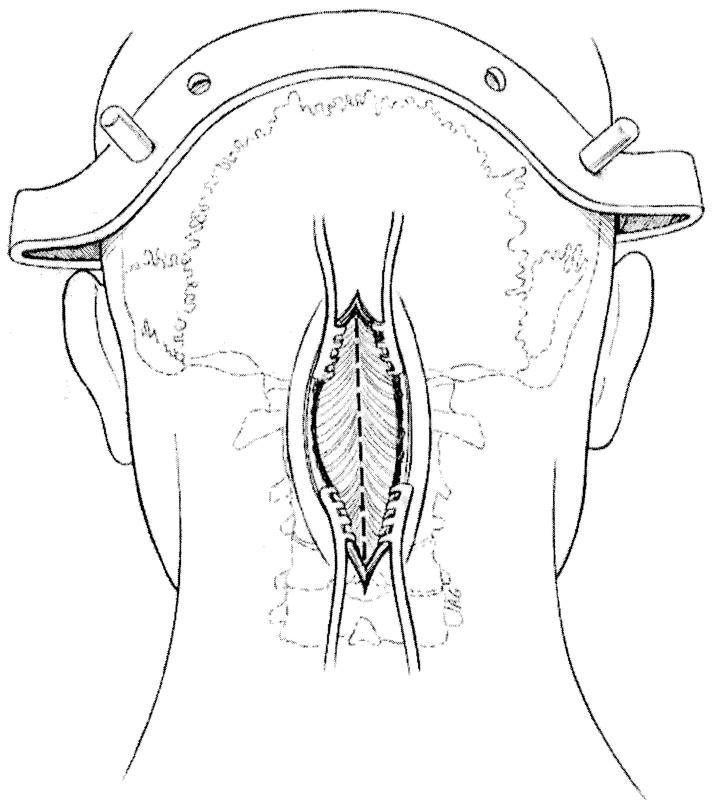
The patient is placed into a reverse Trendelenburg position with a midline incision made from the external occipital protuberance to the spinous process of C2. The C2 vertebra (axis) has a large lamina and bifid spinous process that provides attachments for the rectus major and inferior oblique muscles. The bony topography between the lamina and the lateral mass of the axis is indistinct. Surgical dissection on the occiput and the ring of the atlas should be done in a careful manner. It is advisable to use gentle muscle retraction and Bovie (monopolar and bipolar) cauterization rather than any forceful subperiosteal stripping.
The ligamentum nuchae ( Fig. 26.1 ) represents the midline fascial confluence. Dissection should be carried through this ligament to decrease blood loss and to maintain a stout tissue layer for closure.
The vertebral artery lies lateral to the ring of the atlas ( Fig. 26.2 ); therefore, the dissection should not be carried more than 1.5 cm lateral to the posterior midline and 8–10 mm laterally along the superior C1 border to avoid injury to the vertebral artery. Once the greater occipital nerve is encountered and the fragile venae comitantes of the paravertebral venous plexus are exposed, further lateral dissection endangers the vertebral artery. If bleeding is encountered from disruption of the venous plexus between C1 and C2, packing and hemostatic agents are usually adequate to control bleeding. If vertebral artery injury occurs, direct repair, manual pressure, endovascular treatment, and ligation are options for control of hemorrhage.
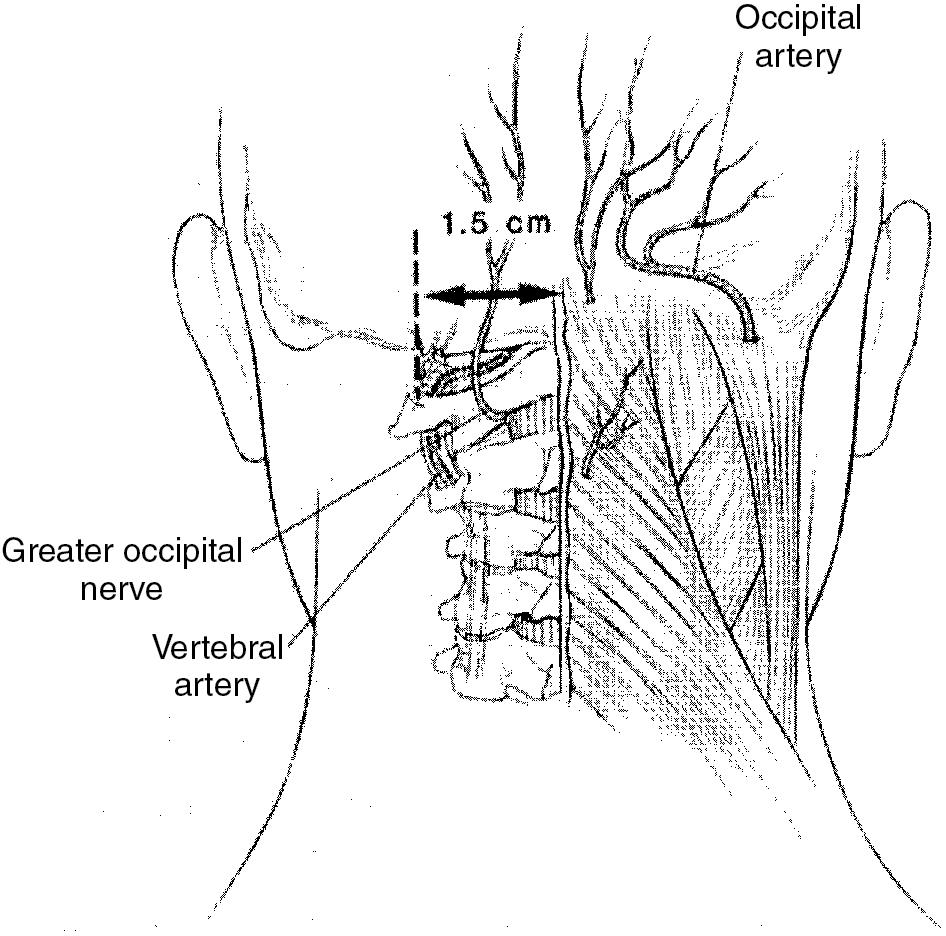
The vertebral artery arises from the subclavian artery. It enters the transverse foramen at C6 in 95% of people and courses upward through the foramina above. At C1, the vertebral artery exits from the foramen, courses medially on the superior groove of the posterior ring of the atlas, and enters the foramen magnum to unite with the opposite vertebral artery to form the basilar artery.
The vertebral artery is injured most frequently just lateral to the C1–C2 facet articulation and at the superior lateral aspect of the arch of C1.
The reverse Trendelenburg position allows venous drainage away from the surgical field and toward the heart, which decreases bleeding during the procedure.
The midline posterior exposure is the most common approach used in the cervical spine. Care is taken to carry dissection through the ligamentum nuchae to minimize blood loss. Once the tips of the spinous processes are identified at the appropriate levels through radiographic confirmation, subperiosteal dissection of the posterior elements is then carried out. The posterior approach is extensile and is easily extended proximally to the occiput and distally to the thoracic spinal region.
Lateral dissection carries the potential risk of denervation of the paraspinal musculature. Inadequate approximation of the posterior cervical musculature may lead to a fish gill appearance of the posterior paraspinal muscles and possible loss of the normal cervical lordosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here