Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The birth of an infant initiates a series of interactions with parents (particularly the mother) designed to initiate attachment and ensure survival. Attachment is a bidirectional emotional and enduring bond that is reciprocated between infant and the caregiver, a process of synchronous coregulation that influences each other's internal state. Human development is sufficiently resilient to withstand some disturbance of the normal postpartum sequence of events that initiate attachment; however, significant problems of either the infant (prematurity; congenital anomalies; transitional problems such as asphyxia, trauma, or peripartum infection) or the mother (complications of pregnancy, depression) have more substantial capacity to disrupt normal processes. These complications carry a risk for disorganized attachment and adverse effects on long-term neurodevelopment in addition to the risks related to prematurity or underlying anomalies.
Emotional and psychological groundwork for secure attachment begins in pregnancy. Increased levels of oxytocin throughout pregnancy facilitate the formation of an emotional bond between mother and infant in humans by acting to reduce anxiety and to ameliorate responses to external stresses. Mothers who have a less anxious state of mind are more able to increase their focus on infant care and recognize and respond effectively to nonverbal infant cues. Unexpected hospitalization during pregnancy, feelings of anxiety and depression, and lack of social support interfere with the development of maternal antenatal attachment. Hospital care practices that reduce anxiety, such as avoiding unnecessary separation of an infant from parents, can contribute greatly to early attachment.
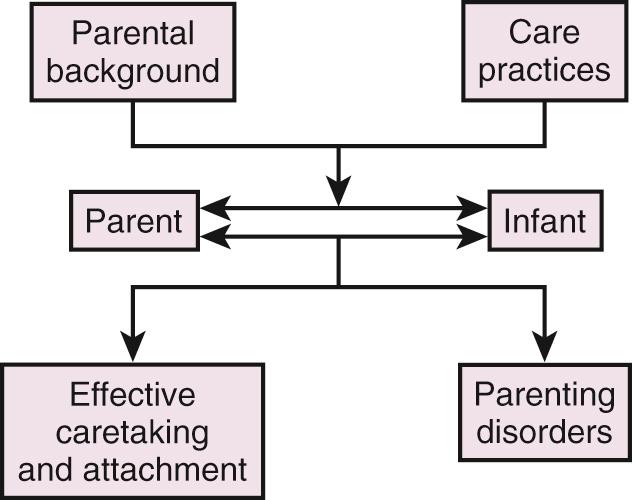
Fig. 42.1 is a schematic diagram of the major influences on parental behavior and the resulting disturbances that may arise from them. Experiences during labor, parent-infant separation, and hospital practices during the first hours and days of life are the most easily manipulated variables in this scheme.
When childbirth moved from the home to the hospital, continuous support of the mother during labor became the exception rather than the routine. Although husbands/partners and female relatives routinely accompany the mother to the delivery room, they usually have little experience in providing labor support and may need support themselves. The clinical value of continuous emotional and physical care during childbirth by a trained doula is supported by the results of the 22 randomized clinical trials conducted over more than two decades. Women allocated to continuous support were more likely to have a shorter labor and a spontaneous vaginal birth. In addition, they were less likely to have intrapartum analgesia or a baby with a low 5-minute Apgar score. Beneficial findings are consistent across the studies despite different cultural, medical, and social practices.
Nearly 90% of newborns require no special intervention at birth. Suctioning is not typically required with clear amniotic fluid, and clearing of the upper airway can be accomplished by simply wiping the infant's mouth and nose. Even nonvigorous infants with meconium-stained amniotic fluid do not need routine intubation and endotracheal suctioning. It should not be necessary to separate the newborn from the mother to administer the initial steps in stabilization. The newborn should be placed on the mother's skin immediately after birth, covered by a blanket. Early skin-to-skin care results in more rapid thermal control and decreased incidence of hypothermia in term and late preterm infants.
The sensory stimuli of touch, warmth, and odor between the mother and infant are powerful vagal stimulants resulting in release of maternal oxytocin, which aids in breastfeeding and mother–infant attachment. Oxytocin production in mothers is maintained postnatally by lactation and also in response to innate infant behaviors such as suckling, clinging, facial expressions, and vocal calls. Oxytocin levels in early pregnancy and the postpartum period are significantly correlated with the frequency of maternal bonding behaviors, including gaze, vocalizations, positive affect, and affectionate touch, as well as the degree of its coordination with the newborn's alert state, attachment-related thoughts, and frequent checking of the infant.
In a concerted effort to promote breastfeeding, the American Academy of Pediatrics, endorsing the WHO/UNICEF publication Ten Steps to Successful Breastfeeding , recommends in a policy statement on breastfeeding that for healthy infants, “breastfeeding should begin within the first hour after birth (even for Cesarean deliveries) and that infants must be continuously accessible to the mother by rooming-in.” Routine procedures including weighing, measuring, bathing, blood tests, vaccines, and eye prophylaxis should be delayed until after the first feeding is completed. These recommendations stem from a global program launched in 1991 by WHO/UNICEF as the Baby-Friendly Hospital Initiative. A recent nationwide American quality improvement initiative of maternity care hospitals showed a rise in hospitals receiving the Baby-Friendly designation, along with an increase in breastfeeding and exclusive breastfeeding rates in those hospitals compared to hospital applicants not in the program.
Immediately after birth, parents enter a unique period in which their attachment to their infant usually begins to blossom and in which events may have many effects on the family.
The first feelings of love for the infant are often instantaneous with the initial contact. However, mothers may express distress and disappointment when they do not experience feelings of love for their infant in the first minutes or hours after birth. In a study of 100 primiparous mothers interviewed within 72 hours of delivery, 39% developed positive feelings prenatally, 42% on the first day, and 19% on the second or third day. Most mothers develop affection for their infants within the first week. Delay in positive feelings until after the first day was associated with labor longer than 8 hours, a feeling of disappointment with the “bonding” experience or breastfeeding, and high depressive symptoms, whereas mothers who fell in love on the first day were likely to cite privacy and the ability to hold their newborn as contributing factors. Providers of health care to the maternal–infant dyad should be aware of the many factors that shape mothers’ affective responses to their infants.
The period of labor, birth, and the following several days has been called a sensitive period, when the mother, and likely the father, are strongly influenced by the quality of care they themselves receive. Perceived stress, social support, and coping strategies are crucial variables in mothers’ adaptation mechanisms at the time of childbirth. Social support during the antenatal or postnatal period appears to be a major factor related to mothers’ psychological health.
This beginning of parent–infant interactions has foundation in autonomic, neurologic, and endocrinologic systems in the mother and infant, and each become sensitized to the temporal patterns of the other, leading to the formation of a unique bond. Rhythmic patterns of neonatal activity such as crying, nursing, or sucking serve as the earliest means of communication. Maternal cues of her voice, touch, and body rhythms in response create a synchronized “dance” between the mother and infant. The high level of positive arousal that infants co-construct with their parents during their face-to-face interactions accelerates the maturation of the infant's relational skills and provides essential environmental inputs for the development of self-regulation and the process of attachment.
These early interactions are not limited to infants and mothers. When fathers are given the opportunity to be alone with their newborns, they not only spend almost exactly the same amount of time with the infants as mothers do, but also respond to infant cues as effectively. Additionally, when fathers had more extended postpartum hospital contact with their infants, they were more involved in infant caretaking responsibilities.
These early affectional ties can be easily disturbed and may be permanently altered during the immediate postpartum period if a newborn requires separation from the mother for care. A mother's anxieties about relatively mild conditions in the newborn (e.g., jaundice requiring phototherapy, slow feeding, mild respiratory distress) may affect her relationship with the child long afterward. Hospital routines should minimize unnecessary separation of newborns from their parents.
Feeding, as part of the mother–infant relationship, should be an enjoyable experience in which the infant feels that his or her cues are being recognized. Supporting breastfeeding promotes attachment, pleasure, and autonomy for mother and infant as they learn together the intricacies of feeding. Mothers may need support to establish breastfeeding using an electric pump. A mother may feel too self-conscious to express milk in public, be anxious about whether she has enough milk, or feel valued more for her expressed milk than for herself. She may delay breastfeeding out of ambivalence, may experience anxiety, or consider herself a failure if the infant is slow to suck, or she may feel confused between the use of breasts for nutrition and sexual intimacy. Mothers who do not wish to or cannot breastfeed also need support, whether or not they express milk. Continuing to express milk for months throughout the night is exhausting even for the most committed mother.
Infants who become exhausted while feeding, who experience painful oral interventions, or who have been forcibly fed may develop an oral aversion. Feeding difficulties may contribute to insecure parent–infant attachment, and infants may become distressed during sucking because they do not feel securely attached emotionally.
Preterm children, particularly those with neurologic impairment, have been reported to be at risk for dysfunctional attachment relationships. Early separation between infant and mother is associated with disorganized attachment and linked to increased parental stress.
Parents who live a distance from perinatal care centers may experience additional separation because of the necessity of transporting their child to a regional NICU. If the infant must be transferred to another hospital, it is important that parents be given a chance to see and touch the infant and take a picture before transfer occurs, receive contact information for the other hospital, and accompany the infant whenever possible. Transporting the mother afterward for postpartum care is beneficial; however, financial barriers and lack of insurance provider coverage are problems in some areas. Parents of transported infants often describe the separation in terms of loss and may experience a grief response even when the condition of the infant is not serious. After the initial transport, parents living far away have continued difficulty visiting their infant and may be helped with access to overnight accommodations.
The design of the NICU impacts patients and families (see also Chapter 36 ). Emphasis on family-centered care has promoted design of single-patient rooms rather than the traditional open-bay NICUs. The single-patient room design can decrease stressful stimuli and allow a private space for parents and infants to have their first interactions. Randomized controlled trials have shown single-patient rooms allow for increased hours of parental visitation and decreased length of stay. However, after controlling for social support, mothers in single-patient rooms reported more NICU stress than mothers in an open-bay NICU design. NICU design benefits from parent feedback in balancing privacy concerns and providing social support to families.
The NICU environment itself is an impediment to parent bonding with their child. The incubator is a physical barrier to the parent's comforting touch; the tubes and patches obscure the infant's cues. In addition, the parents may be hesitant to interact with preterm infants due to their immaturity and medical severity. Preterm infants have less “babyish” physical features and are less active, alert, and responsive than full-term infants. Their cry is perceived more aversive and distressing to parents. Parental bonding may be delayed until the infant's physical condition appears to be improved and parents are assured of the infant's survival.
Neonates experience a variety of stressors while in the NICU, including painful procedures, mechanical ventilation, decreased maternal care, and auditory and light stimulation. Exposure to painful stimuli causes activation of the hypothalamic-pituitary-adrenal (HPA) axis and subsequent release of glucocorticoids. Cumulative stress, such as a higher number of skin-breaking procedures, can result in altered programming of the HPA axis and decrease in cortisol release in response to stress. Such alterations to neurodevelopment following early-life pain exposure may account for adverse behavioral outcomes later in life, including poorer cognitive outcomes and increased internalizing behavior. Maternal care, especially kangaroo care (see below), can negate consequences related to neonatal pain and promote beneficial outcomes.
Staff need to be aware that if parents continue to approach their infants reluctantly, this may indicate a prolonged complicated reaction, different from a mother's reaction after birth when being close may stir mixed emotions, such as feelings of failure about the preterm birth. Parents may resist engaging with the infant because of a traumatic birth, shock at the infant's appearance, or a poor prognosis about survival and disability. When parents cannot hold their infant, they may find it hard to believe that the infant is their child, particularly with an in vitro fertilization (IVF)-conceived infant. Mothers with a very low birth weight infant may feel less effective because of the need for the nurses’ care; when a parent finds it hard to attach to a very low birth weight infant, staff can talk with him or her about the infant's personality traits. It can be pointed out to parents who feel that they have to ask permission to hold their infant, that they do not have to ask permission to be loving parents. If parents become phobic about entering the unit because of its associations or their fear of bad news, this should be explored and additional support offered.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here