Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
We are grateful to Professors Ursula Ravens, Alexander Quinn, and Niels Decher for helpful comments on the manuscript. We thank the European Research Council, the German Research Foundation, and the Ministry of Science, Research and the Arts of the Federal State of Baden-Württemberg for their generous support of research in our labs. The authors are members of the German Collaborative Research Centre SFB1425.
The heart has the vital function of rhythmically generating mechanical force to drive the circulation of blood. Its shape, structure, and physiology, from the molecular to the whole organ levels, contribute to generating the work required in a highly efficient manner. Much more than a simple pump, this fascinating organ adjusts its throughput to changes in physiologic demand and has a high capacity for adaptation when facing pathologic conditions. In addition to being a highly sophisticated and adjustable organ, its workload is considerable: 2.5 billion (10 9 ) contractions per relaxation cycles over a 75-year period (assuming 65 beats/min), it pumps the equivalent of the volume of one Olympic-size swimming pool (50 m × 25 m × 2 m) each year but also generates enough pressure work (by the left ventricle [LV] alone) to lift King Kong (assuming a weight of 10 tons) to the rooftop of the Empire State Building (381 m). One striking feature of the heart is its exquisite capability to respond to mechanical stimuli, including mechanics as part of regulatory feedback loops that fine-tune the heart’s functions in physiologic conditions and as protective mechanisms that act in response to pathologic disturbances. The processes by which passive and/or active mechanical properties affect cardiac electrophysiology are known as mechano-electric coupling (MEC). Observations of MEC date back to the 19th century in the European medical literature, when cases of sudden cardiac death caused by precordial impact were first reported. These early accounts were followed up by a large number of additional observations, highlighting the omnipresence and complexity of MEC. Ultimately, the mechanisms and sensors underlying cardiac MEC are still under investigation, even though a number of molecular candidates have been identified.
This chapter briefly reviews the variety of mechanical stimuli at play in the heart, identifies known mechanosensors, and focuses on the identity and function of a specific subclass: potassium (K + )-selective stretch-activated ion channels, whose role in physiology and pathology are discussed.
The heart functions in a highly dynamic mechanical environment and is continuously generating and exposed to a complex set of mechanical stimuli. These stimuli have three different origins: extracorporeal, intracorporeal/extracardiac, and intracardiac ( Fig. 14.1 ).
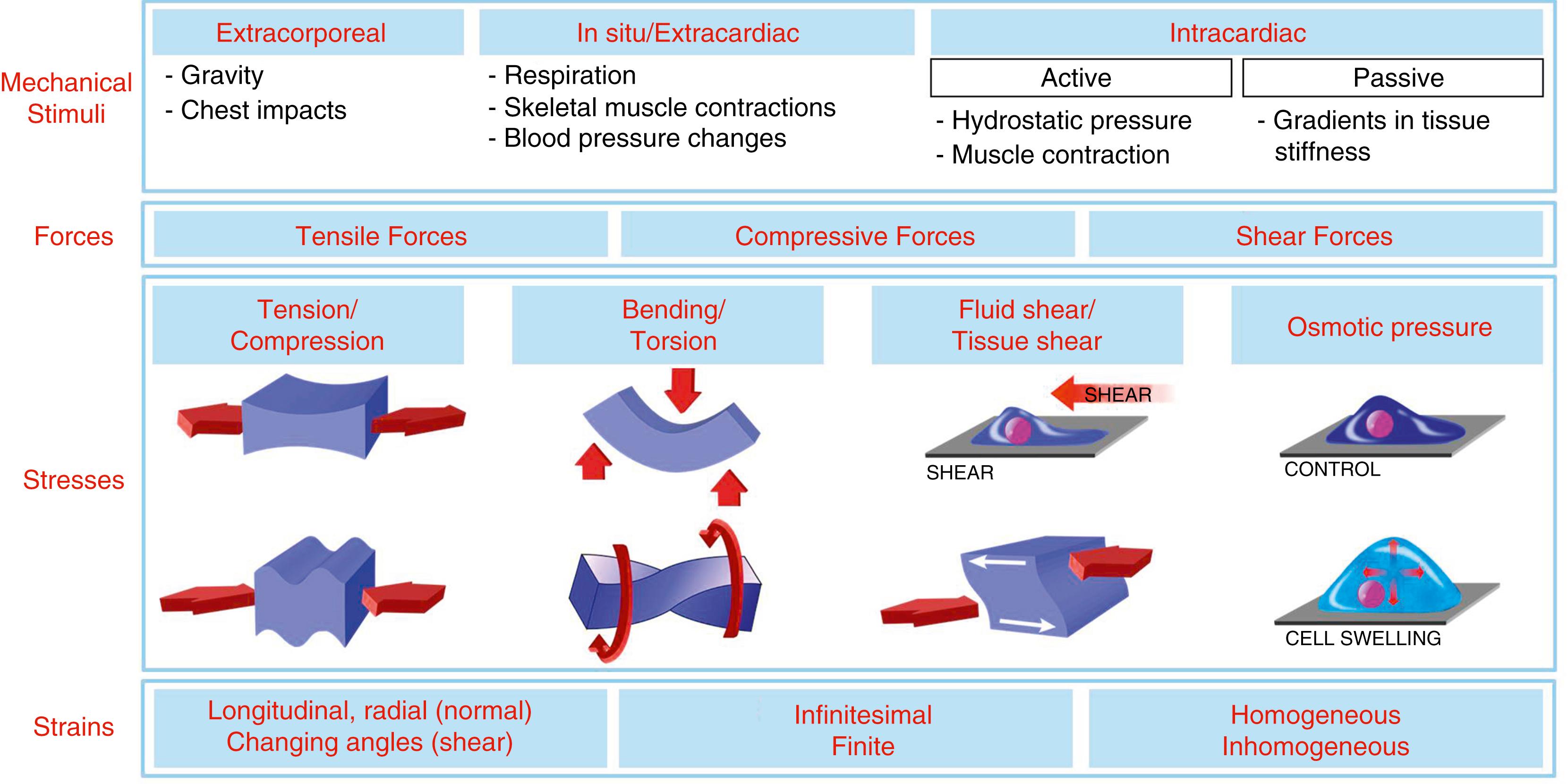
Mechanical influences that reach the heart from outside the body range from gravity-mediated changes in venous return during posture changes to anything impacting the chest.
Extracardiac in situ influences, such as breathing-associated pressure gradients and fluxes (e.g . , air in the lungs, blood in large vessels linking chest and abdomen), skeletal muscle contractions (e.g., during coughing or straining), and altered hemodynamic demand (e.g., during physical activity, at high altitude, or in pregnancy), are examples of stimuli capable of changing the in situ mechanical environment of the heart.
Mechanical cues from the heart itself can be divided into two categories: active and passive mechanics. Active forces, generated by muscle cells, involve structural alterations from nano to macro scales, involving proteins, membranous nanodomains, cells, extracellular matrix (ECM), tissue, and the whole organ. Myocytes are the principal source of active force, driving rhythmic cardiac contractions, although they are not the only cells able to contract. Smooth muscle cells and nonmyocytes such as fibroblasts are also known to contract actively, even if at orders of magnitude lower force and speed. Fibroblasts represent a nonnegligible part of the myocardial cell population, estimated to account from 20% to over 50% of the nonmyocyte population, depending on the tools used, and as chief producers of the ECM they also alter passive mechanics of cardiac tissue.
Indeed, active contraction can be impaired by mechanical properties of the tissue. These are determined in part by the ECM, which can be extensively remodeled in the course of disease. Tissue remodeling can lead to major changes in passive mechanical properties over time and/or space. After myocardial infarction (MI), for example, myocardial stiffness is initially decreased (down to a few kilopascals), but upon formation and maturation of postinfarct scar tissue, stiffness can rise to values of 50 to 100 kPa, well exceeding the stiffness of healthy tissue in the range of 5 to 10 kPa. This alters the workings of the myocardium. Pathologically soft ventricular tissue areas can bulge (paradoxical segment lengthening) during contraction of surrounding healthy myocardium, generating areas of increased stress and strain. Stiff fibrotic tissue produces less force (because of the decreased number of cardiomyocytes and the stiffened ECM, which is suspected to change myocyte contractility).
Pathologic tissue remodeling also alters force distribution, resulting in local regions of high stretch that are thought to trigger arrhythmias. Importantly, fibroblasts are not the only cell type that should be considered in the context of tissue remodeling: Immune cells, including macrophages, are also major players where mechanosensors are proposed to have important functions.
The forces present in the heart can be tensile, compressive, and shear inducing. These forces produce stresses ([force per unit of area], same unit as pressure) as illustrated in Fig. 14.1 .
Stress , if high enough, leads to deformation. The amount of deformation an object experiences, compared with its original size and shape, defines the strain (dimensionless). This parameter is, in most cases, the most easily accessible (both in experiments and by medical imaging), and it allows one to track mechanical input to a number of pathways initiated by mechanosensors.
Based on these definitions, the distinction between force, stress, and strain is clear.
In practice, the matter is much less trivial. Because of the heart’s complex histoanatomy, ventricular force generation gives rise to regionally and temporally varying shortening, thickening, sliding, bending, and twisting. Passive and active forces, as well as stresses and strains, coexist and are highly heterogeneous. In fact, it would be reasonable to suggest that no two cells in the heart undergo exactly the same mechanical cycle, that these cell-specific mechanical dynamics change with external hemodynamic demand, and that this high degree of cellular (force-length) heterogeneity is prerequired for externally homogeneous (pressure-volume) work, as expertly explained by Katz and Katz. Adding to the complexity, while deformations can often be tracked and quantified, there are no tools as of yet to report intramural forces (they can only be approximated, based on generally incomplete characterization of passive mechanics and ensemble properties such as intracavity pressure generated).
It is understandable therefore that the wording used to refer to mechanical stimuli tends to be vague and that it does not usually refer to actual physical parameters, including the phenomena activating mechanosensors. This chapter uses the term stretch , unless in contexts where stresses or strains at play can be characterized or quantified.
In spite of the omnipresence and diversity of mechanical stimuli, the heart is capable of adjusting to such dynamic settings. Manifestations of cardiac MEC are present at all levels of structural and functional integration, from in situ and ex vivo whole heart, over in vitro tissue and cells, to subcellular domains such as membrane patches, enzymes, and proteins. An extensive number of observations and experiments, reviewed in Quinn and Kohl, contributed to establishing MEC as a key mechanism regulating cardiac function.
MEC manifestations have been identified in physiologic and pathologic conditions, with positive or negative effects on cardiac function. Some prominent examples are highlighted here, with focus on acute electrophysiologic responses to mechanical stimuli because medium to long-term effects are more ambiguous, mainly because of the simultaneous structural and functional remodeling that can make the identification of causal links between mechanical inputs and electrophysiologic outputs difficult.
In physiology , one principal manifestation of MEC is the Bainbridge effect, whereby increased venous return to the heart induces a positive chronotropic response. This fundamental mechanism allows the heart to adjust its work to circulatory demand.
In pathologic conditions (e.g., in the presence of an arrhythmogenic structural substrate), increased intraventricular pressure may trigger ectopic excitation and promote reentrant excitation in animal models and patients. Even in healthy myocardium, under certain conditions, acute mechanical stimulation alone can be sufficient to give rise to both trigger and sustaining mechanisms for arrhythmogenesis. A prominent example of this is commotio cordis, where cardiac rhythm disturbances of varying type and severity are initiated by nonpenetrating mechanical impact to the precordium, in the absence of detectable structural damage to the heart.
Certain therapeutic interventions take advantage of MEC to terminate heart rhythm disturbances. Precordial fist-thumps, for example, have been used to pace asystolic ventricles, whereas acute temporary removal of ventricular overload in patients, using the Valsalva maneuver, illustrates the antiarrhythmogenic potential of normalization of ventricular-loading conditions. For comprehensive reviews on clinical relevance of MEC, see Quinn and Kohl, as well as Kohl, Sachs, and Franz. ,
While MEC includes a large number of electrophysiologic responses of the heart to mechanical stimulation, cardiac mechanosensitivity goes well beyond MEC, including mechano-mechanical and mechano-chemical coupling. In addition, cardiac nonmyocytes also respond to changes in the mechanical environment. Cardiac fibroblasts, stem cells, and progenitor cell function are, in part, controlled by matrix stiffness, composition, and topology, for example, during tissue remodeling.
Essential components underlying mechano-transduction are the structures transmitting mechanical stimuli (ECM, cytoskeleton, transmembrane structural proteins, lipid bilayers) and elements converting mechanical forces into a signal interpretable by the cell: mechanosensors. , Among them, the most well-known are kinases (Rho kinase, integrin-linked kinases, mitogen-activated protein [MAP] kinases), integrins, G protein–coupled receptors, and mechanosensitive ion channels. Mechano-transduction pathways, mediated by these molecules, can interact. The interplay between stretch-activated channels (SAC) and integrins or kinases, for example, has been well illustrated in a number of organs, including the heart.
This chapter focuses on SAC that contribute to both acute MEC responses and to mechanically induced tissue remodeling. Based on ion selectivity, cation nonselective and potassium (K + )-selective channels (SAC NS and SAC K , respectively) can be distinguished. This chapter focuses primarily on SAC K , which have received less attention in considerations of cardiac MEC. For comprehensive coverage across other SAC types, see the review by Peyronnet, Nerbonne, and Kohl.
Mechanosensitive ion channels can be subdivided into mechanically modulated channels that are not primarily gated by mechanical factors but whose activity, localization, or expression can be modified by the mechanical environment and mechanically gated channels whose open probability is directly and primarily changed by mechanical stimuli ( Fig. 14.2 ). Mechanosensitive ion channels can be found in the plasmalemma of most prokaryotic and eukaryotic cell types and in intracellular membrane systems, such as the sarcoplasmic reticulum, mitochondria, and the nuclear envelope.
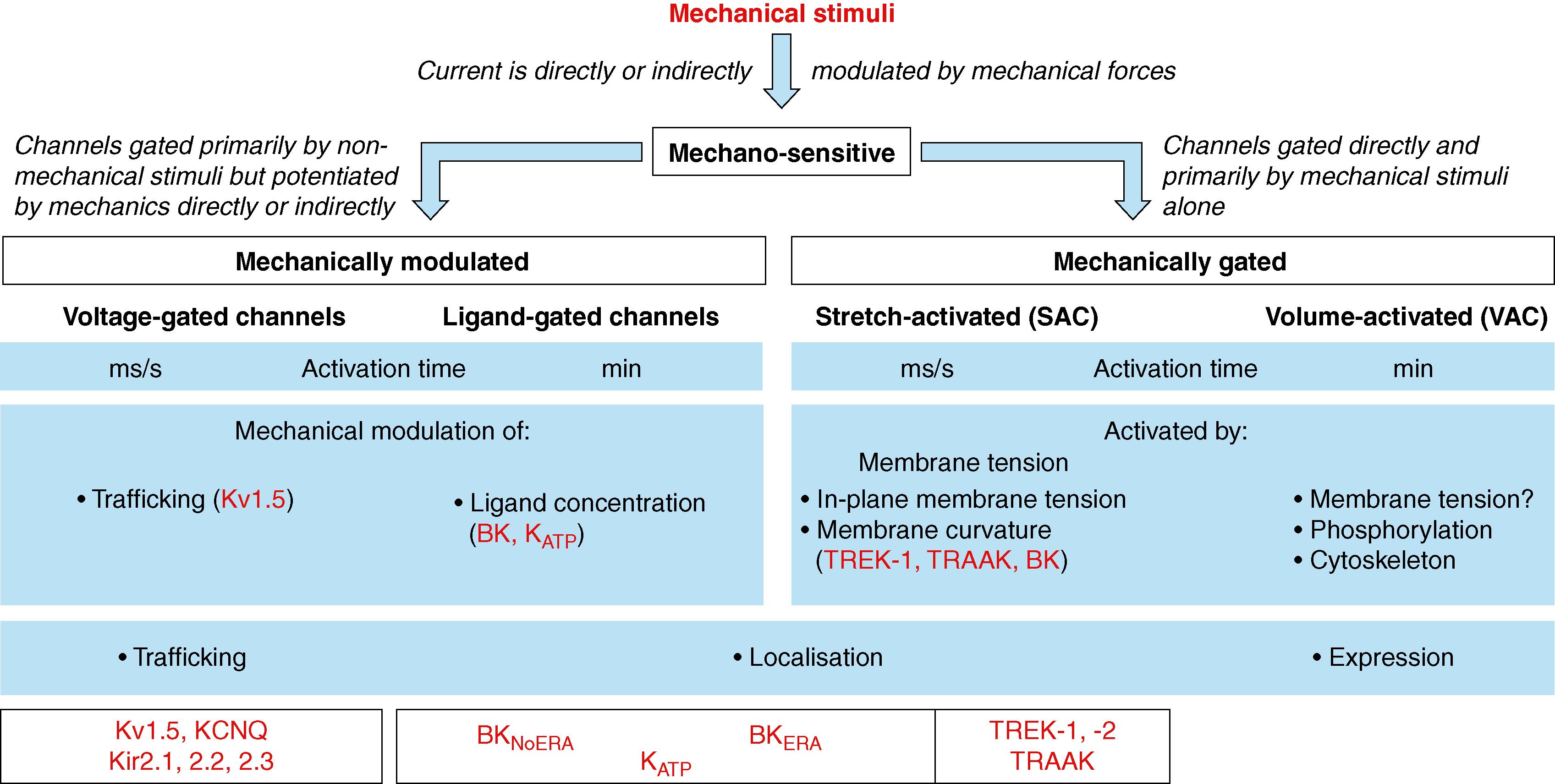
Like other phenomenologic classifications, mechanosensitive ion channel categories are not absolute, and there is overlap with other ion channel nomenclatures. Several mechanosensitive ion channels are primarily voltage and/or ligand sensitive, while MEC effects arise from mechanical modulation of channel activity, localization, or expression.
A representative of ligand-gated mechanosensitive ion channels is the adenosine triphosphate (ATP)-inactivated K + channel (K ATP ). It is primarily gated by ATP, but channel open probability is also increased by stretch in atrial , and ventricular myocytes. In fact, the range of mechanosensitive ion channels might be underestimated: Theoretically, all ion channels whose in-plane projection in the membrane increases upon opening should have their open state favored by an increase in membrane tension. Additionally, the transmembrane voltage sensors of some voltage-sensitive ion channels (as shown, in particular, for SAC K ) may be influenced directly by membrane structure (e.g., composition of membrane lipids) and mechanical state (e.g., in-plane membrane stretch).
Mechanically induced membrane deformation can change the localization of ion channels. The voltage-gated K + channel K V 1.5 is an example; this channel is primarily voltage gated, but its trafficking is modified by shear stress in atrial cardiomyocytes, involving protein relocalization from intracellular compartments to the sarcolemma. Thereby, sarcolemmal K V 1.5 current density is modulated by the mechanical environment.
Another mechanism involves mechanically induced integration of membrane invaginations, such as caveolae, into the surface sarcolemma. This can increase the number or effectivity of ion channels actively participating in transsarcolemmal ion fluxes (also known as space activation ). Mechanical activation of caveolae-based ion channels has been documented for swelling-activated chloride ion channels, increasing (by 10-fold to 50-fold) pulmonary vein sensitivity to stretch, and promoting development of atrial fibrillation (AF). Caveolin-SAC interactions have also been suggested where caveolin-1 inhibits the channels.
Mechanically induced changes in ion channel expression would be the slowest of the three modalities (the other two can principally act on a beat-by-beat time scale). Still, it would make ion channels appear mechanosensitive. This is applicable to all channels, including SAC.
The open probability of mechanically gated ion channels is primarily modulated by mechanical stimuli, such as stretch (for SAC) or cell volume changes (volume-activated channels [VAC]). The mammalian heart contains both SAC and VAC.
SAC respond within milliseconds to mechanical stimuli, , whereas VAC tend to show significant lag times (up to minutes) between the onset of cell volume changes and ion channel response. VAC are understood to be important contributors to cardiac electrophysiology in chronic disease settings, such as (post-)ischemic cell swelling and hypertrophy (where VAC are constitutionally active). For comprehensive reviews of VAC, see Okada et al. and Strange et al . , In the context of electrophysiologic responses to beat-by-beat changes in the mechanical environment, however, SAC are implied as a key mechanism underlying MEC.
The existence of SAC was first reported in 1984 by Guharay and Sachs in embryonic chick skeletal myocytes. SAC activity, initially considered by many as an artifact because of the difficulty of combining electrical recordings with membrane stretch, was quickly corroborated in other model systems, from bacteria to mammalian cardiomyocytes.
The SAC family includes SAC NS and SAC K . The ion selectivity profiles of these channels determine their transmembrane current reversal potential, which is halfway between activation potential (AP) plateau and resting potential for SAC NS (usually between 0 mV and –25 mV) and close to the K + equilibrium potential for SAC K (about –95 mV in cardiomyocytes).
SAC NS include Piezo and transient receptor potential (TRP) channels. Piezo1 and Piezo2 were shown to be involved in a number of physiologic and pathophysiologic processes in several organs, including the heart (for Piezo1). Members of the vast TRP family are involved in mechano-transduction processes, and a number of them are expressed in the myocardium, but their direct stretch activation remains controversial.
Given their depolarizing effect on resting cardiomyocytes, SAC NS have been implicated in mechanically triggered excitation and arrhythmogenesis. They have been comprehensively reviewed in the recent past and in previous editions of this textbook. Therefore the remainder of this chapter focuses on SAC K .
Most SAC K identified so far are localized at the plasmalemma ( Fig. 14.3 ), no doubt in part because of the comparative ease of access to this membrane, compared with endomembranes, using established electrophysiologic tools.
![Fig. 14.3, Subcellular localization of mechanosensitive K + channels. Red font indicates stretch-activated channels; black font indicates mechano-modulated channels. (Organelles adapted from F. Aguila [French National Centre for Scientific Research].) ER , Endoplasmic reticulum; SR , sarcoplasmic reticulum. Fig. 14.3, Subcellular localization of mechanosensitive K + channels. Red font indicates stretch-activated channels; black font indicates mechano-modulated channels. (Organelles adapted from F. Aguila [French National Centre for Scientific Research].) ER , Endoplasmic reticulum; SR , sarcoplasmic reticulum.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/StretchActivatedPotassiumChannelsintheHumanHeartPathophysiologicandClinicalSignificance/2_3s20B9780323757454000147.jpg)
The first paper on SAC K activity from cardiac cells dates back to 1987, exploring molluscan ( Lymnaea ) ventricular cells. Shortly after, SAC K were recorded from mammalian heart cells (rat atrial cells). K + ions move more easily out of the cell than into it because of the K + gradient. SAC K therefore pass so-called “outward” currents. They are usually characterized by large, single-channel conductance and the presence of inactivation. When activated, they contribute to repolarization or hyperpolarization of the plasmalemma. SAC K have been observed both in cardiac myocytes and nonmyocytes from atrial and ventricular tissue. SAC presence in cardiac nonmuscle cells is not surprising because these cell types are also mechanosensitive. Fibroblasts, for example, respond to shear stress, stretch, and changes in substrate stiffness.
TREK-1 (TWIK-related K + channel 1 [TWIK stands for tandem of two-pore K + domains in a weakly inward rectifying K + channel]), TREK-2, and TRAAK (TWIK-related arachidonic acid–stimulated K + channel) belong to the large family (15 members) of K 2P channels (i.e., channels with two pore [2P] domains). A pore domain is a signature sequence, defined as a short amino acid segment between two transmembrane helices that contributes to formation of the inner part of the pore. The assembly of four pore domains forms the selectivity filter of ion channels. Apart from TREK-1, -2 and TRAAK, no other known SAC are K 2P channels. Very little is known so far about possible roles of cardiac TREK-2 and TRAAK channels. Their expression seems significantly lower in mouse hearts compared with TREK-1, whereas in humans there are conflicting reports.
TREK-1 is one of the best characterized SAC K . It is the first mammalian SAC that was molecularly identified (cloned in 1996, recorded in a heterologous system in 1998), and it has been reported in the human heart. TREK-1 is a polymodal channel gated by a number of stimuli, including stretch, heat, protons, and a variety of lipids, such as free polyunsaturated fatty acids, lysophospholipids, phosphatidylinositol 4,5-bisphosphate (PIP 2 ), lysophosphatidic acid, and phosphatidic acid, as well as pharmacologic agents, such as volatile general anesthetics. , ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here