Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The first modern practical application of neuroprostheses to move paralyzed limbs was to correct foot drop in hemiplegic subjects ( ). Based on the success of the Lubjliana foot-drop system, became the first to apply electrical stimulation in spinal cord injury (SCI) for functional purposes. Long and Masciarelli used a splint that passively held the fingers closed and achieved finger opening by electrical activation of the finger extensors. This work led directly to the work of with C5 tetraplegic subjects. The first implanted motor neuroprosthetic systems in SCI were used by researchers in Cleveland ( ) and London ( ).
A critical development in the application of functional electrical stimulation (FES) in SCI was the discovery that electrical stimulation of muscle results in muscle conditioning, increased strength, and increased fatigue resistance. Early applications of FES had little success because not enough muscle force could be generated and maintained for functional tasks, especially in SCI where atrophy can be quite severe. and showed that chronic application of electrical stimulation to paralyzed muscles not only conditioned the muscle but actually changed the muscle fiber from type 2 (fast twitch, fast fatiguing) to type 1 (slow twitch, slow fatiguing). Protocols for muscle conditioning are now part of the standard implementation of any motor neuroprosthesis.
Traumatic SCI can result in paralysis below the level of the spinal cord lesion. The American Spinal Injury Association (ASIA) defines the neurological level of injury as the most caudal segment of the spinal cord with normal motor and sensory function on both sides ( ). Tetraplegia is defined as the impairment or loss of motor and/or sensory function in the cervical segments of the spinal cord due to damage of neural elements within the spinal canal ( ).
A key physiological factor in SCI is the muscle denervation and atrophy that results from lower motor neuron damage ( ). Although SCI is considered primarily an upper motor neuron disease, there is typically a region of lower motor neuron damage within the spinal cord. If this region is extensive, it severely limits the ability to utilize FES to produce movement. In some cases it is possible to use electrical activation of paralyzed but innervated agonists to make up for the inability to activate denervated muscle ( ).
Upper-extremity systems have been primarily applied to individuals with C5 and C6 ASIA SCI. These individuals have the ability to position the hand in space, flex the elbow, and, for the C6 level, extend the wrist. For more severe injuries (C4 and above) the difficulties in producing useful whole-arm movements have not been completely solved, and this is an area of current research.
Historically, neuroprostheses have been implemented in individuals who had complete (ASIA A) SCIs. In a complete injury it is usually straightforward to separate the function provided by the electrical stimulation and the function under voluntary control. In many incomplete injuries stimulated and voluntary functions are intertwined, making outcome assessment more difficult. Despite this, recent advances in system design have made neuroprostheses more applicable to incomplete injuries ( ).
Electrical activation of paralyzed muscles takes maximum advantage of the remaining physiological function for an individual with SCI. Stimulation of paralyzed muscles is placed under the direct control of the individual and coordinated with any remaining voluntary movement that the individual retains. The control signal is derived from an action over which the user has retained voluntary control, which can include hand function (for paraplegic individuals), shoulder movement, recorded muscle activity, respiration, or voice control. A coordinated stimulation pattern is developed so that the muscles are activated in a sequence that produces the desired function. Individuals with these devices appreciate the fact that they can still use their own limbs to enable them to stand or eat, even though the direct connection to the central nervous system has been disrupted.
Although many researchers have demonstrated that closed-loop control incorporated into a motor neuroprosthesis results in improved results, to date there are no clinically deployed implanted systems that include closed-loop control. This is primarily due to the difficulty in creating reliable sensors and robust feedback loops.
Implanted upper neuroprostheses are applied to individuals with SCI who are otherwise in good health and are good surgical candidates. It is common practice to wait until at least 1 year after injury before implementing an implanted neuroprosthesis to ensure that any recovery from the injury is complete. The subject must not have excessive limitations in the range of motion of the joints to be activated. Spasms, if present, must be controlled pharmacologically.
The subject must have sufficient integrity of the lower motor neuron (peripheral nerve) to the muscles to be stimulated (see Pertinent Anatomy, Physiology, and Disease Pathophysiology section). Thus individuals with lower motor neuron disease, such as brachial plexus injury or amyotrophic lateral sclerosis, are generally not candidates for neuroprostheses. Most candidates for neuroprosthetic implantation are skeletally mature because of the concern that skeletal growth would result in stretching of the leads in the extremities, possibly resulting in tension failure in the leads or connectors of the system. However, research by has shown that appropriate routing of leads can accommodate significant growth.
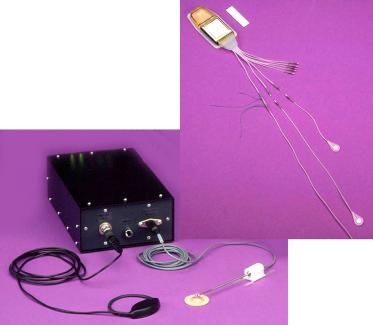
Clinically deployed neuroprostheses for grasp and release utilize an active implantable device delivering stimulus pulses through electrodes implanted in the paralyzed upper extremity muscles, as shown in Fig 96.1 . A first-generation implantable neuroprosthesis for control of hand grasp/release was developed by the Cleveland FES Center and first implemented in a human volunteer in 1986 ( ). This was known as the Freehand System, and used an eight-channel receiver–stimulator (IRS-8), eight epimysial or intramuscular electrodes, leads, and connectors. A radio-frequency (RF) inductive link provided the communication and power to the IRS-8. The external components of the neuroprosthesis were an external control unit, a transmitting coil, and an external shoulder position transducer ( ). The external control unit performed the signal processing of the control inputs and generated the output signal (modulated RF) delivered to the implanted receiver–stimulator. The RF transmitting coil was taped to the individual’s chest directly over the implant receiver–stimulator to make the inductive powering and communication link.
To operate the neuroprosthesis the user depressed a switch on the chest that activated the system, and the user’s hand opened into full extension in a lateral pinch mode ( ). Graded elevation of the user’s contralateral shoulder resulted in graded grasp closure ( ). A quick movement of the shoulder “locked” the hand so that it remained closed at the desired degree of closure, until another quick movement of the shoulder released the lock command. Depressing the chest switch briefly caused the system to switch to a palmar grasp. Depressing the switch for a longer time turned the system off.
A second-generation platform technology was subsequently developed that allowed stimulation of additional channels and control with implanted sensors, known as the Implantable Stimulator–Telemeter (IST) Platform. The key feature of the IST Platform was bidirectional telemetry that allowed the use of implanted control signals, thus freeing the user of all externally donned components beyond a single transmitting coil ( ). Additional stimulation channels provided advanced functions, including better hand and arm control.
The IST Platform was designed to allow implanted stimulation and control while still utilizing external computational processing and power ( ). This system provided a command control structure, an inductive RF link providing power to the implant device, two-way transcutaneous communication, an application-specific integrated circuit (ASIC) for decoding the command and giving functional control within the implant, and modular circuitry providing the application-specific implant functions. Two implant configurations were realized from the IST Platform. The first, the IST-10, had 10 channels of stimulation and one channel of telemetry used to transmit power and receive joint-angle information from the transducer implanted in the radial carpal joint of the wrist ( ). The second configuration of the IST Platform, the IST-12, had 12 stimulation channels and acquired implanted myoelectric signals (MESs) for control ( ).
The control algorithm developed for the IST-12 used a common controller template but was customizable for each user. Typically, two successive high-level bursts of muscle activity in the shoulder or neck were generated to turn the system on. The user selected the desired grasp pattern using bursts of activity from the same muscle. Once the pattern was selected, the user had direct proportional control of the degree of hand opening and closing through the MES level from the voluntary forearm musculature (either brachioradialis or extensor carpi radialis longus). Strong contraction of this muscle resulted in hand closing, while relaxation of the muscle resulted in hand opening. If the user desired to hold an object for a long period of time, he/she could initiate a “lock” command which disengaged the grasp stimulation from control by the forearm MES. The lock command was initiated by holding the MES above a high threshold for 2 s. Once the hand was locked, it remained locked until an “unlock” command was given. The unlock command could consist of two quick bursts of activity from the forearm (referred to as a “double-click”) or a quick burst of activity from the shoulder. The user could also independently activate other functions, such as elbow extension or forearm pronation, by producing a specific pattern of myoelectric activity in the shoulder. The significant advantage of the myoelectric control, in addition to eliminating the need for external switches, was that all control signals are derived ipsilaterally, so the opposite arm was free to be utilized as a helper hand. Thus myoelectric control is ideally suited for bilateral implementation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here