Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The purpose of this chapter is to discuss the general principles, challenges, and opportunities in establishing a reconstructive transplant program. The authors bring the experience of two centers in two different countries with significantly differing healthcare systems: the United States and France. The authors provide their own perspectives and experiences. L. Lantieri is a plastic and reconstructive surgeon who established a face transplant program in Paris, France, and has performed one of the largest series of face transplantations in the world. H. Amer is a transplant nephrologist and founding medical director of the first reconstructive transplant center in the United States to obtain institutional approval for both hand and face transplantation as an extension of clinical practice.
Reconstructive transplantation is the bringing together of two multidisciplinary practices, reconstructive surgery and transplantation, to benefit a very select group of patients. Reconstructive surgeons for many years have brought healing and recovery to victims of significant tissue loss or damage resulting from trauma, malignancies, or burns. Despite significant advances in the field of reconstructive surgery, major limitations exist, particularly in patients with major limb loss and those with severe facial deformities. One of the most utilized tools in reconstructive surgery involves microvascular free tissue transfers, which is essentially an autotransplant. Combining all of the conventional techniques currently available, including prosthetics, there remains an inability to restore a severely deformed face or restore function and sensation to a patient with a major limb loss. Processed biomaterial such as tendons and skin has provided additional options but still has limitations. Transplant surgery provides the patient with a procedure that is a huge leap forward in reconstruction, where restoration of normal anatomy is possible.
Transplant physicians and surgeons have, since the first successful kidney transplant in 1954, offered patients with end organ failure, the option of replacing their failed organ with a healthy organ from another individual. The field of solid organ transplantation has progressed since that first successful kidney transplant in 1954 between identical twins, to a point where it seems routine to have a kidney, heart, liver, pancreas, or lung transplant. Thousands of transplants are performed annually all over the world, some from deceased donors and some from live donors. The understanding of immunology and immunosuppression management has enabled better, more tolerated, and in some cases, tailored immunosuppression for thousands of patients who have gone on to lead productive and near normal lives.
In 1998, the collaboration between reconstructive surgeons and the transplant community resulted in the first successful hand transplant and, in 2005 the first partial face transplant.
Hand and face transplantation differs from solid organ transplantation in several ways; they require successful reinnervation to provide function (motor and sensory) and the organs are visible. They differ from previously used free flaps, grafts, and processed tissues, in that they require immunosuppression to prevent rejection.
With over 30 face transplants and over 100 hand transplants performed at the end of 2014, the concept of vascular composite allotransplantation (VCA) has become a clinical reality. Many of the cases, particularly in face transplants, have been one-shot experiences. In face transplantation, only three teams have done more than three cases. Even if this procedure is risky, it is proven to be not only feasible but also reproducible. Although there is a lack of long-term results, the initial results show that in a very select group of patients with specific indications, the benefits may outweigh the risks.
A team that intends to set up a hand or face transplant program must realize that not everything is written and standardized and it is through a trial and error process that a reconstructive surgery team can establish a sustainable program. Undoubtedly, many problems will be encountered. Therefore, a thorough and thoughtful process must be established, which will provide a standardized process that will be effective and efficient. A significant amount of administrative, clinical, and experimental work has to be completed prior to embarking on a transplant. The authorization process is generally a long process and the department needs to become involved early in the planning process. The team leader should propose a detailed plan. This plan consists of team selection and approval from the independent committees. A hand or face transplantation program requires an intricate network of physicians, nurses, technicians, and administrators to function smoothly and effectively. The idea itself can shock many people who are involved in the transplantation process from organ procurement to the final result. It is critical to convince all involved members of the value of having a reconstructive transplant program. Therefore, it is essential to organize regular meetings. The team leaders must present to all the different groups that will be involved in the care of these patients in order to get “buy-in.” All levels of leadership and personnel within the institution must become convinced that this technique is essential for an institution that wants to stay at the cutting edge of reconstructive face and limb rehabilitation.
The momentum to develop a reconstructive transplant program can begin from a variety of individuals at any institution. It should be remembered; however, that reconstructive transplantation, whether hand or face, is primarily a surgical procedure. The patients that are being helped may benefit from transplantation, but many may best be helped by non-transplant reconstructive procedures. As such, a reconstructive transplant program must have a strong reconstructive surgery program that routinely deals with severe hand and face deformities in which a multidisciplinary approach is practiced. The patient must have access to any and all necessary ancillary and complementary therapies such as physical therapy, anaplastology, and prosthetics. When a patient is evaluated, they should be considered for all possible therapies, and transplantation would be one of the options available to them if indicated. It should not be the only option considered or offered.
As such, reconstructive transplant programs should emanate from reconstructive surgery departments. Having said that, reconstructive transplantation will require extensive support and expertise not present in reconstructive surgery departments. Once there is at least one advocate for reconstructive transplantation in the reconstructive surgery department, a careful assessment of the resources present and those that are needed to bring together an expert team and develop a program is performed. As mentioned above, although the first successful hand transplant was performed in 1998, since that time there have been fewer vascularized composite transplants performed worldwide than the number of solid organ transplants performed by some single centers in 1 year. As such, the role of the reconstructive transplant program in the care of an institution's patients as well as the institution's overall operations and goals has to be assessed.
If the decision is made to establish a program, then the lead reconstructive surgeon should begin to reach out to the needed disciplines and begin making a case for the development of such a program. Education regarding the role of reconstructive transplantation in the care of severely disfigured patients is of paramount importance. This education will need to be tailored to fill anticipated gaps in knowledge and understanding of various audiences. Audiences will include fellow reconstructive transplant surgeons and other providers who care for patients with reconstructive surgery needs but who may not be fully aware of the state of reconstructive transplantation. It will also include the transplant practices with the various members and ancillary support staff who may be very comfortable with transplantation but may not be aware of the needs of these patients, or of the limitations of modern reconstructive surgery and prosthetics.
Education should extend to individuals in the institution who may not necessarily become involved in reconstructive transplantation. This could include the departments of surgery, medicine, laboratory medicine, physical therapy and rehabilitation, nursing etc. Given that no transplant can occur without a donor, rapport, education, and discussion should be started early with the local organ procurement organization.
A reconstructive transplant team comprises many disciplines: reconstructive transplant surgeons; transplant physicians well-versed in the evaluation and management of transplant recipients; oculoplastic surgeons; physical and occupational therapists; pharmacists; social workers; radiologists and radiological services; tissue typing experts; transplant infectious-disease specialists; dermatologists and dermatopathologists; surgical pathologists, preferably familiar with pathology of other organ allografts; psychiatrists and psychologists; anesthetists; ethicists; nursing staff; intensivists; and operating room personnel. From a surgical perspective, it should be noted that contrary to most conventional reconstructive surgery procedures, the surgical team has to train regularly with rehearsals on cadavers with and/or without scrub nurses and other team members. Besides the technical knowledge gained by these rehearsals, it allows for better cooperation between the different elements of the team. It is essential that the adequate surgical expertise is developed to allow simultaneous procurement and recipient preparation at remote sites. Members of the team should be cross-trained to allow easy substitution as the need arises. There should also be enough redundancy to allow for substitution in the event of extreme fatigue during the lengthy operations or unexpected absences when a donor becomes available. The team leader must structure a schedule that includes breaks for every team member. Surgeons in reconstructive transplantation can be drawn from plastic and reconstructive surgeons, oral and maxillofacial surgeons and/or head and neck surgeons, and transplant surgeons, as long as they are involved and believe in the project.
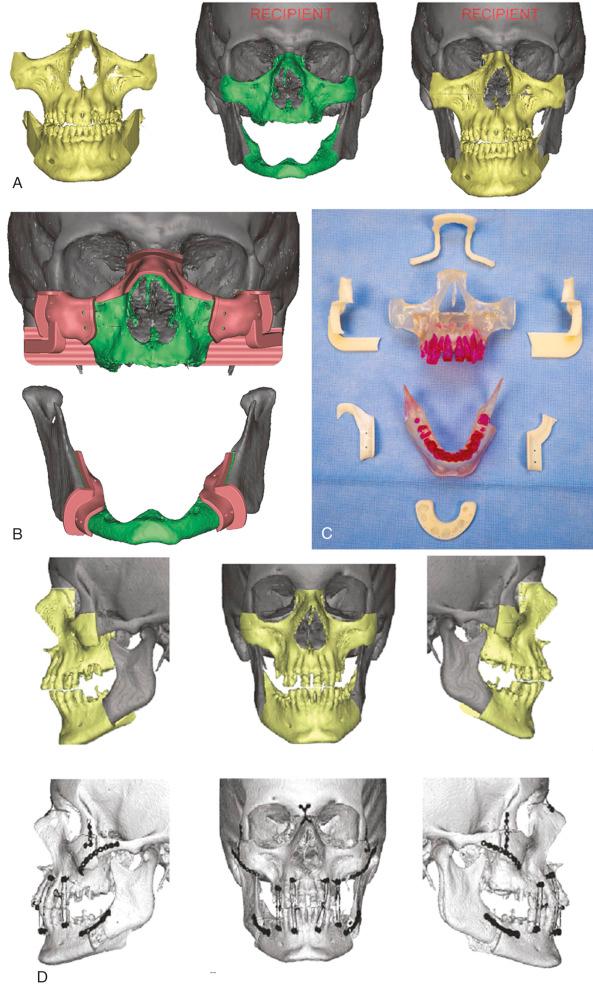
As the team comes together, it is important to meet regularly. Allow input from all team members and have frequent discussions and debates. This is important to build communication channels, bring everyone up to speed on the developments in the field, appreciate the various facets of the different specialties, and ensure trust among team members. There should be small workgroups formed to tackle particular problems. Frequent rehearsals and “walk-throughs” of the planned protocols and procedures must be undertaken. Collaboration with a company that provides cutting-edge 3-D technology-driven virtual surgical planning is critical when bone is involved in the transplant. The Mayo Clinic team has benefited from a collaboration with Medical Modeling, where a team of bioengineers receive CT data for the donor and recipient and a web meeting is undertaken with Dr. Mardini to plan the surgical procedure. Models, cutting guides, and positioning guides are provided to the surgical team in order to optimize accuracy and efficiency during the procedure ( Fig. 63.1 ). For the surgical members of the team, frequent simulated procurements and transplants reflecting the planned transplant for each patient is important. Team members should be encouraged, if not mandated to attend relevant society meetings such as the American Society for Reconstructive Transplantation biennial meeting or the International Hand and Composite Tissue Allotransplantation Society. Site visits to other reconstructive transplant programs are also beneficial. Given the relative novelty of reconstructive transplantation and the scarcity of patients transplanted, there are no standard universally approved data-driven guidelines of who to transplant or how. It will be important for each new program to gain as much knowledge and experience from other programs prior to embarking on their first transplant.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here