Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Participation in sports is associated with foot and ankle injuries; however, one does not need to be an athlete to experience a twisting, impaction, contusive, or repetitive traumatic event. In addition, some conditions are initiated by antecedent trauma; the history of the condition may be nonspecific, and symptoms of injury may have subsided (e.g., chondromalacia or osteochondritis dissecans of the ankle). Other than fractures or dislocations, trauma produces at least three kinds of joint affections: (1) acute severe ligamentous injuries with joint disruptions, (2) ligamentous injuries of lesser magnitude from a single episode or from repetitive “overuse” producing nondisruptive and microscopic abnormalities of the joint, and (3) aggravation of preexisting joint abnormalities. Miscellaneous affections of joints probably not caused by trauma but possibly aggravated by athletic, recreational, or occupational activities are discussed in Chapter 48 .
Sprains constitute 85% of all ankle injuries, and 85% of those involve a lateral inversion mechanism. Ankle injuries account for 14% to 21% of all sports-related injuries; approximately 40% of basketball injuries and 25% of soccer injuries involve the ankle. Volleyball and football also have especially high risks of ankle ligament injury. Compared with men, women have a slightly higher overall incidence of ankle injuries in similar sports activities. Men, however, have a higher incidence of medial ankle and syndesmotic sprains. Greater mean height and weight, increased body mass index, and certain athletic activities (e.g., basketball, cheerleading, rugby) may be risk factors for ankle sprains as well.
Ankle ligamentous injuries, as classified by O’Donoghue, occur as minor ligamentous “stretch” injuries (type I sprain), incomplete ligamentous tears (type II sprain), or complete disruption of the ligament or ligaments (type III sprain). A more practical approach is based on the stability of the ankle as determined by stress testing and the functional level of the patient ( Box 90.1 ). Eversion and abduction of the foot may result in disruption of the deltoid ligament; however, more commonly the inversion stress results in ligamentous disruption on the lateral side of the ankle (usually the anterior talofibular ligament or calcaneofibular ligament). Diagnosis and treatment depend on an understanding of the ligamentous and muscular structures around the ankle.
Stable ankle (clinical and radiographic studies with anesthesia as needed)
Symptomatic treatment
Unstable ankle (+ anterior drawer or talar tilt clinically and radiographically)
Low-demand patient
Functional treatment
High-demand patient
Surgical intervention
Continued pain or functional instability
Surgical intervention based on examination and imaging studies
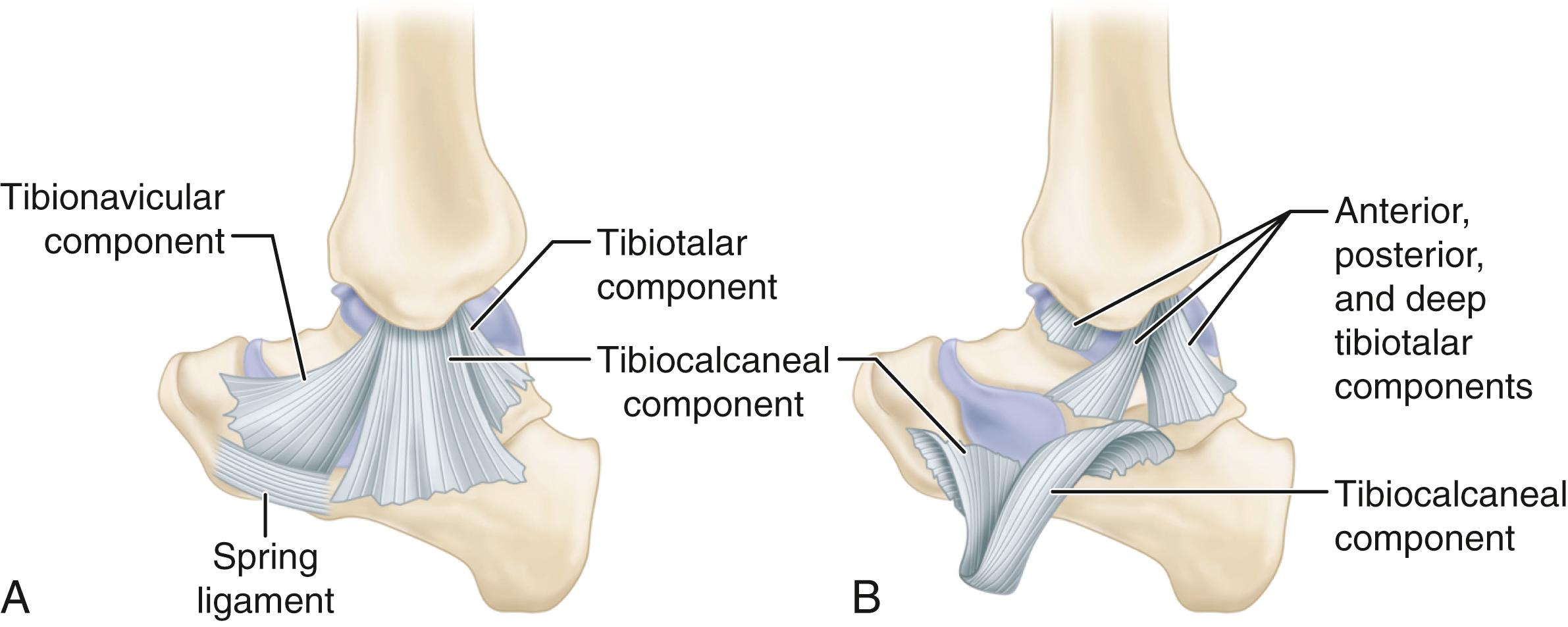
Stabilizing the medial side of the ankle anteriorly and posteriorly is the strong, flat, triangular deltoid ligament consisting of five components. The deep portion of the deltoid ligament is probably the most important and provides the greatest restraint against lateral translation. The two components, the anterior and posterior deep tibiotalar ligaments, attach to the undersurface of the medial malleolus and the body of the talus ( Fig. 90.1 ). Both deep components are intraarticular but extrasynovial. The posterior deep tibiotalar ligament is the strongest of the entire deltoid complex. The superficial portion of the deltoid ligament consists of the other three components: the tibionavicular component anteriorly, the tibiocalcaneal component in the middle, and the posterior tibiotalar component posteriorly. Both the superficial and deep components resist valgus tilting of the talus and are secondary restraints against anterior translation of the talus.
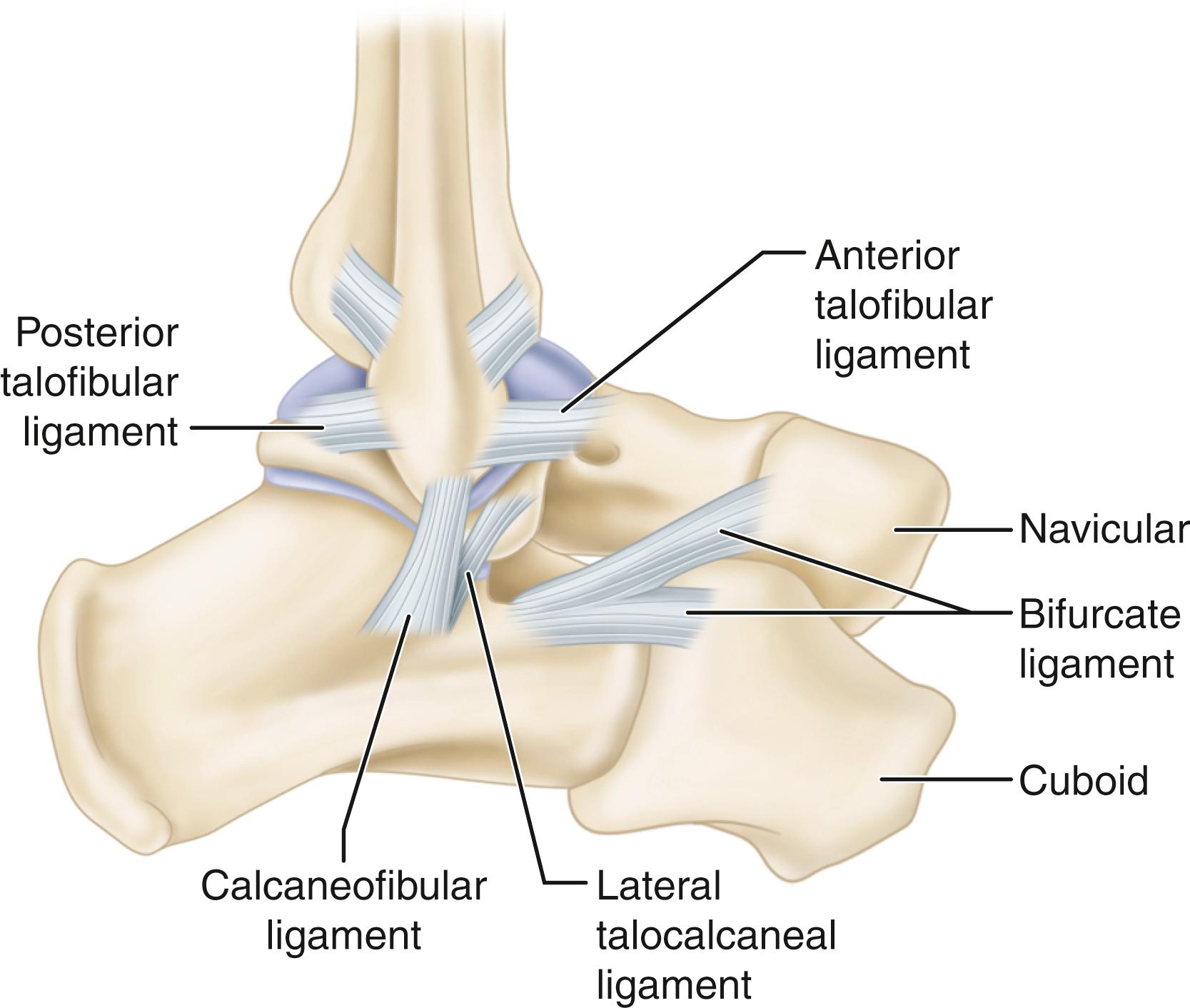
Laterally, the three primary ligaments that stabilize the ankle vary in structure ( Fig. 90.2 ). The anterior talofibular ligament is 2.0 to 2.5 mm thick, 15 to 20 mm long, and 6 to 8 mm wide and is attached posteriorly to the anterior border of the lateral malleolus and anteriorly to the neck of the talus, where it blends with the anterolateral joint capsule. It is the weakest and most often injured of the lateral ligaments. It primarily functions to resist anterior translation of the talus when the ankle is in a relatively neutral position. The calcaneofibular ligament is 20 to 25 mm long, 6 to 8 mm wide, and 3 to 4 mm thick and is stronger than the anterior talofibular ligament. It is attached superiorly to the tip of the lateral malleolus, extends deep to the peroneal tendons, and inserts inferiorly on the lateral surface of the calcaneus (it is the only lateral ligament that is extracapsular). The posterior talofibular ligament is 30 mm long, 5 mm wide, and 5 to 8 mm thick and is the strongest of the lateral ligaments. It is attached anteriorly to the digital fossa of the fibula and posteriorly to the lateral tubercle on the posterior aspect of the talus. The bifurcate ligament does not assist in maintaining stability of the ankle, but injury to this ligament often is misdiagnosed because of its proximity to the lateral ankle ligaments. The bifurcate ligament is attached to the anterior process of the calcaneus. Just distal to the origin, the ligament divides in a Y-shaped manner to insert on both the dorsomedial aspect of the cuboid and the dorsolateral aspect of the navicular.
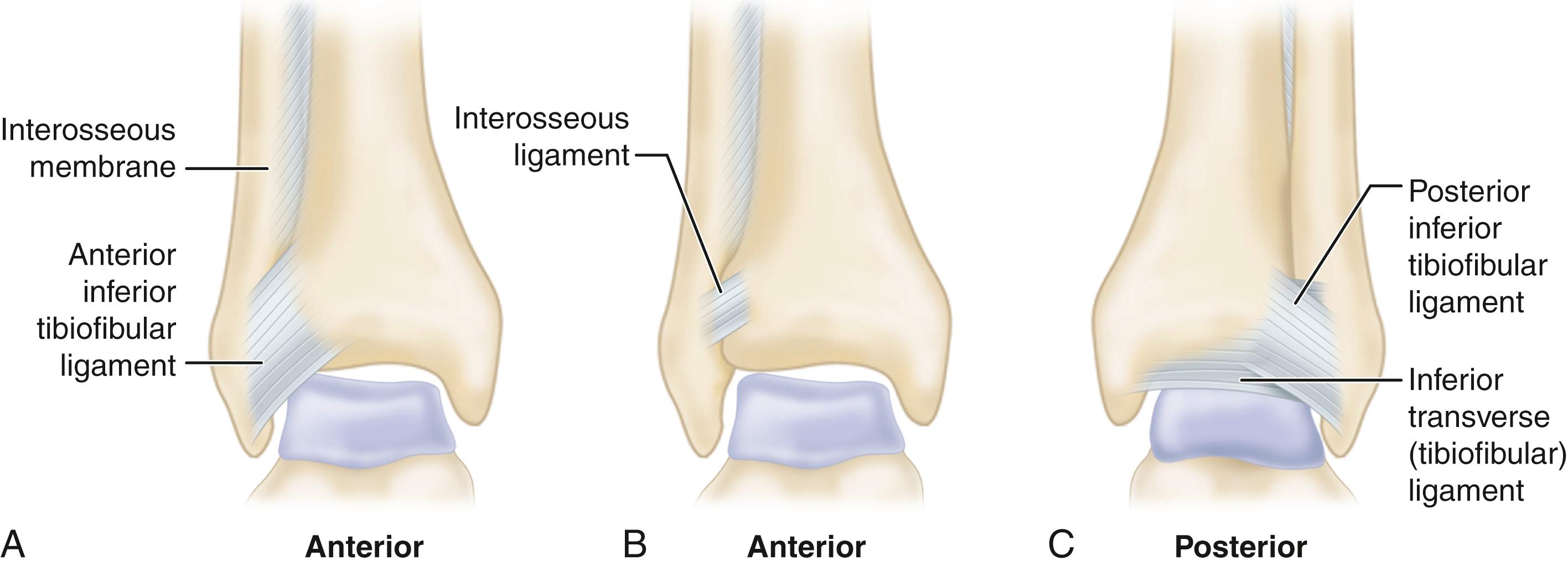
The relationship of the distal tibiofibular syndesmosis is maintained by four ligaments ( Fig. 90.3 ). The anterior inferior tibiofibular ligament attaches medially to the anterior tibial tubercle, extends inferior and lateral, and inserts on the anterior fibula. Occasionally, a slip of this ligament (Bassett’s ligament) inserts distally on the fibula and may cause impingement symptoms at the anterolateral aspect of the talus (see Fig. 90.36 ). The posteroinferior tibiofibular ligament is the strongest component (the interosseous membrane is not part of the distal tibiofibular syndesmosis) and runs in a similar direction as the anteroinferior tibiofibular ligament. The inferior transverse tibiofibular ligament is deep and inferior to the posteroinferior tibiofibular ligament. On its anterior surface, the inferior transverse tibiofibular ligament forms a labrum that articulates with the posterolateral talus, effectively deepening the tibiotalar joint. The interosseous tibiofibular ligament attaches to the contiguous rough surfaces of the tibia and fibula and is continuous with the interosseous membrane proximally. With dorsiflexion of the ankle, the syndesmosis allows the fibula to translate, rotate, and proximally migrate. This ligamentous complex also allows the fibula to share approximately 16% of the axial load.
A careful physical examination is essential to avoid misdiagnosis. The following structures must be palpated because they may be associated with a complaint of ankle pain: the anterior talofibular, calcaneofibular, bifurcate, syndesmotic, and deltoid ligaments; the medial and lateral malleoli; the fifth metatarsal base and the insertion of the peroneus tertius onto the dorsal fifth metatarsal base; the anterior process of the calcaneus and lateral process of the talus; and the Achilles, peroneal, posterior tibial, flexor hallucis longus, and flexor digitorum longus tendons. Frey et al. found that physical examination was 100% accurate in the diagnosis of grade III ligament injuries but only 25% accurate in the diagnosis of grade II injuries compared with MRI findings. Clinicians most often underestimate the damage with a grade II ligament tear. Van Dijk et al. suggested that a more accurate diagnosis is possible if physical examination is performed 5 days after injury rather than within 48 hours.
In acute injuries, diagnosis by stressing the ankle for instability is often difficult but may be improved with an appropriate regional block. Injection of local anesthetic into the peroneal sheath and lateral gutter of the ankle before provocative maneuvers of the ankle often improves the examination of the lateral ligaments by decreasing guarding and muscle spasm. Inversion-eversion and anteroposterior stress testing (anterior drawer sign) can be used to evaluate acute and chronic instability and to help determine the extent of the injury, but stress tests must clearly show a significant difference between the abnormal and normal ankles before they can be considered diagnostic.
Complete rupture of the deltoid ligament, including the deep portion, is less common. When the deltoid ligament is completely disrupted with rupture of the tibiofibular syndesmosis or fracture of the lateral malleolus, the talus can shift laterally with eversion stress. External rotation stress radiographs allow the accurate diagnosis of deltoid incompetence in patients with supination-eversion (Lauge-Hansen) fibular fractures with a reduced mortise. Direct examination around the medial malleolus for tenderness, swelling, and ecchymosis are poor predictors of instability. Some shift of the talus laterally may occur when the syndesmosis alone has been ruptured. Eversion stress radiographs of normal ankles have been reported to reveal little talar shift or tilt.
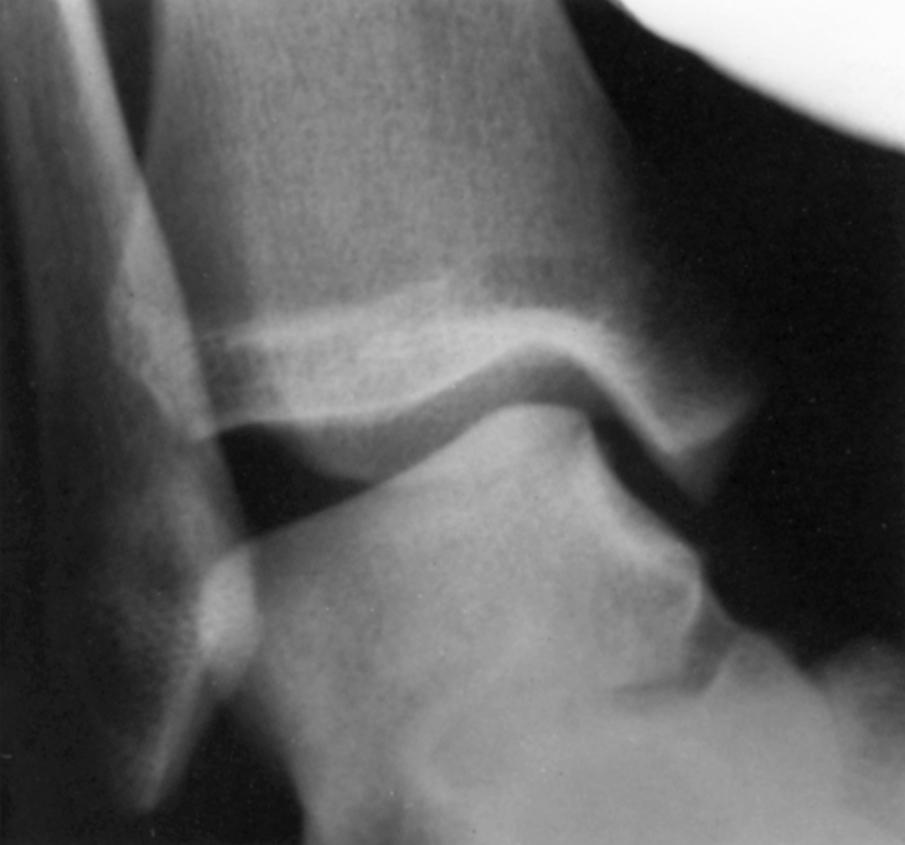
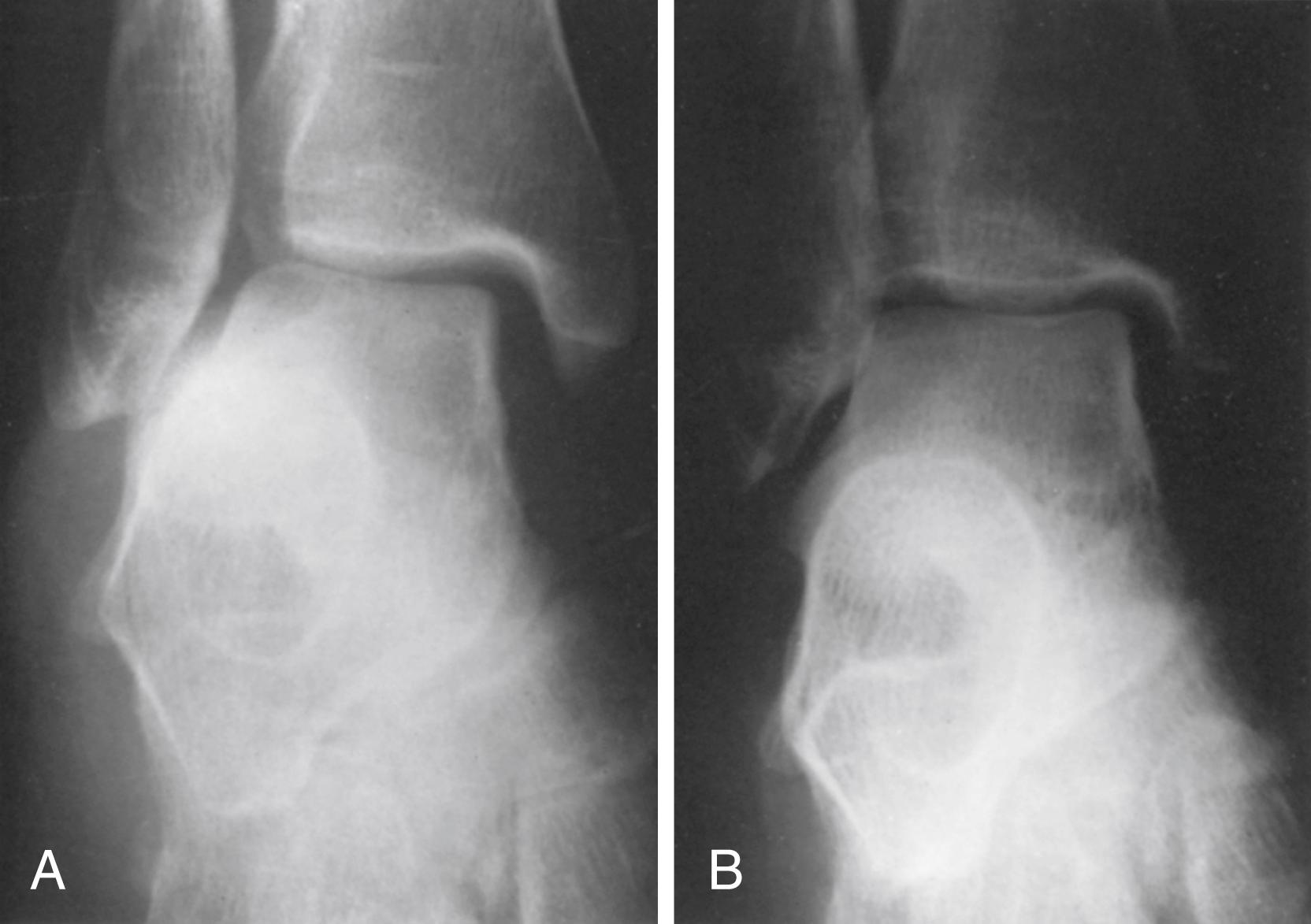
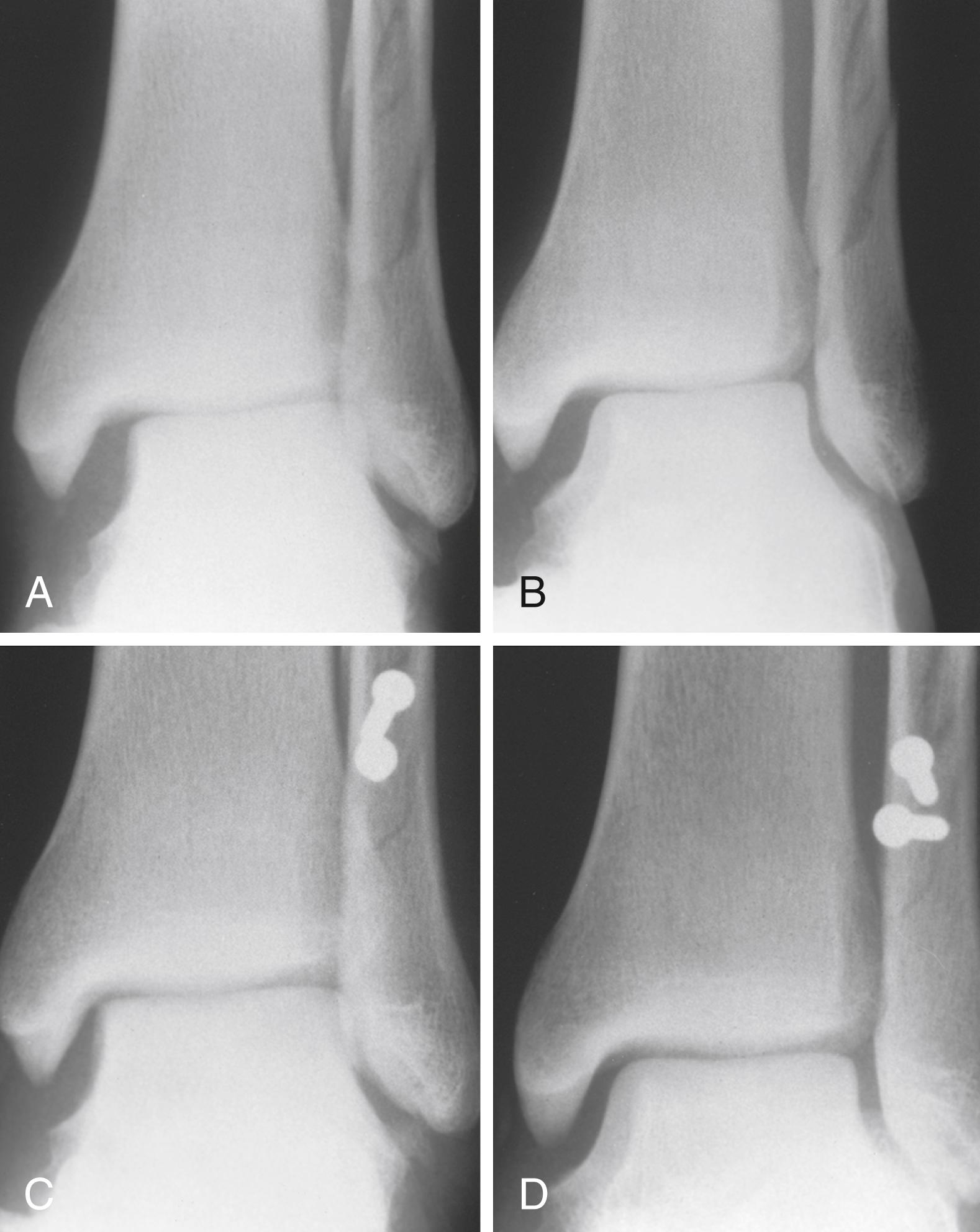
If the lateral ligaments are completely disrupted, the talus tilts with inversion stress ( Fig. 90.4 ). Inversion stress is best applied with the ankle plantarflexed. Tilting of the talus 15 degrees may indicate rupture of the anterior talofibular ligament alone, tilting 15 to 30 degrees indicates rupture of the anterior talofibular and calcaneofibular ligaments, and tilting more than 30 degrees may indicate that all three of the lateral ligaments (anterior and posterior talofibular as well as calcaneofibular ligaments) were ruptured. However, there is no absolute endpoint to distinguish a positive talar tilt from a negative one. At our institution, we stress both ankles and believe that more than 10 degrees of talar tilt over that of the normal side indicates a significant lateral ligamentous injury. Stress radiographs do not need to be obtained routinely because most unstable ligamentous injuries are treated functionally with good results. “Functional” treatment usually refers to the use of RICE ( r est, i ce, c ompression, e levation) and a short semirigid brace. This is followed by early range-of-motion exercises and early weight bearing with an emphasis on neuromuscular training.
An os subfibulare (an ossicle adjacent to the fibula inferiorly) may represent an avulsion fracture instead of a normal variant and may or may not be associated with laxity of the anterior talofibular ligament. Recurrent inversion sprains of the ankle and continuous discomfort are indications for stress films to determine any tibiotalar joint laxity and any movement of the os subfibulare.
The anterior drawer sign ( Fig. 90.5 ) indicates a tear of the anterior talofibular ligament. Clinically, it is helpful to place the tip of the thumb on the tip of the lateral malleolus while palpating the lateral talar process with the base of the thumb. The ankle is held in neutral or slight plantarflexion and is allowed to internally rotate. With gentle stress, one can assess the degree of anterior displacement of the talus relative to the tibia ( Fig. 90.5C ). A sulcus sign may be present with disruption of the anterior talofibular ligament ( Fig. 90.5D ). A relatively low-magnitude load is all that is required when evaluating the integrity of the anterior talofibular ligament in an acute ligamentous ankle injury. More important than the number of millimeters of displacement is the clinical impression that the talus is subluxating out of the mortise.

Recently, subtalar sprains have garnered more attention. Although it is difficult to differentiate between a subtalar and ankle sprain, negative stress films in the presence of a clinically serious ankle injury or patient-reported chronic functional instability should arouse suspicion of an underlying subtalar sprain. Most subtalar ligamentous injuries occur in combination with injuries of the lateral ligament of the ankle. Sectioning of the interosseous talocalcaneal ligament along with the anterior talofibular ligament produces a significant change in subtalar motion compared with injury to the anterior talofibular ligament alone. To determine the appropriate treatment in a symptomatic patient, subtalar stress radiographs (inversion stress Broden view) in addition to routine talar stress radiographs to quantify the relative contributions of each of these joints to inversion laxity may be useful. Several authors, however, have questioned the validity of these tests to diagnose subtalar instability.
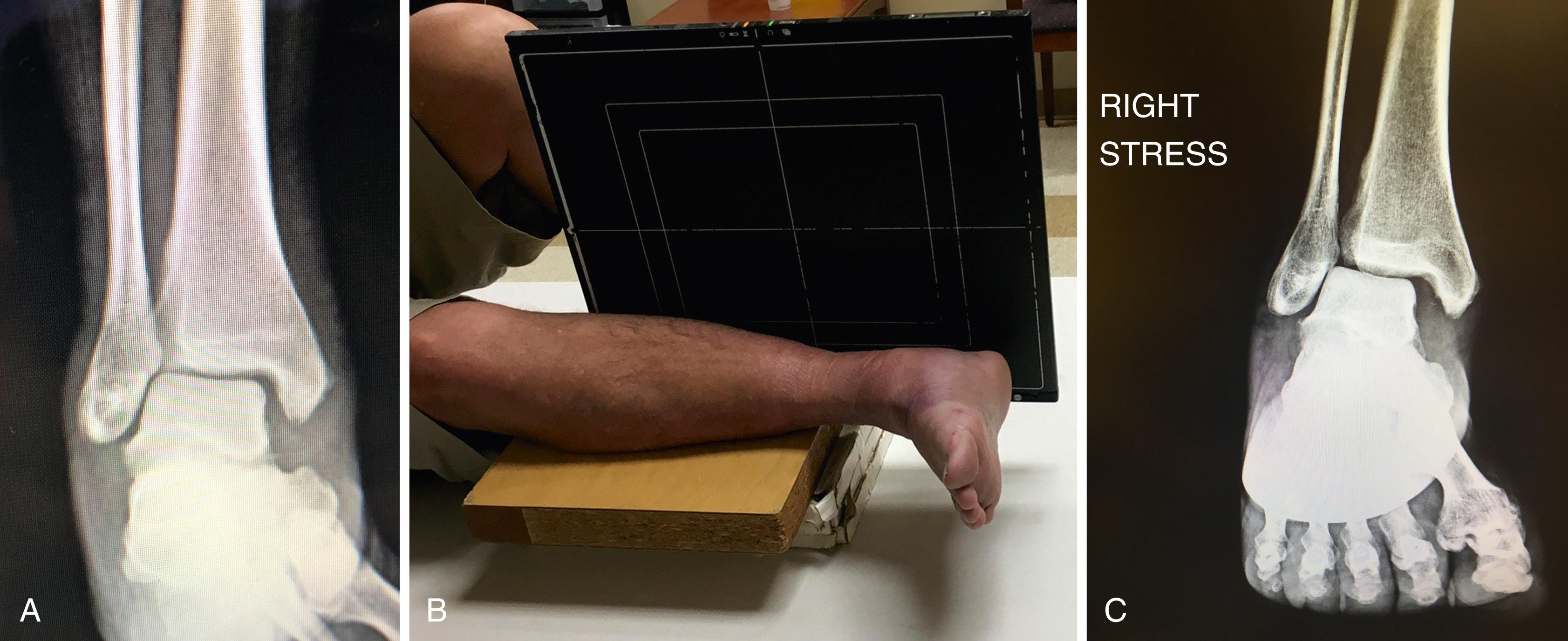
If not pronounced a stress view of the mortise may help in diagnosing syndesmotic injuries ( Fig. 90.6A ). Gravity and manual external rotation stress views are both effective, although radiographic measurements are influenced by position. We usually opt for the gravity stress view because this causes less discomfort to the patient. To perform the gravity stress view, the patient is placed in a semilateral position with the affected side down. The injured limb is placed over a bolster, with the distal third of the leg “floating” off the table and the cassette positioned for a cross table lateral image ( Fig. 90.6B ). This allows for external rotation stress of the mortise and diagnosis of the instability ( Fig. 90.6C ).
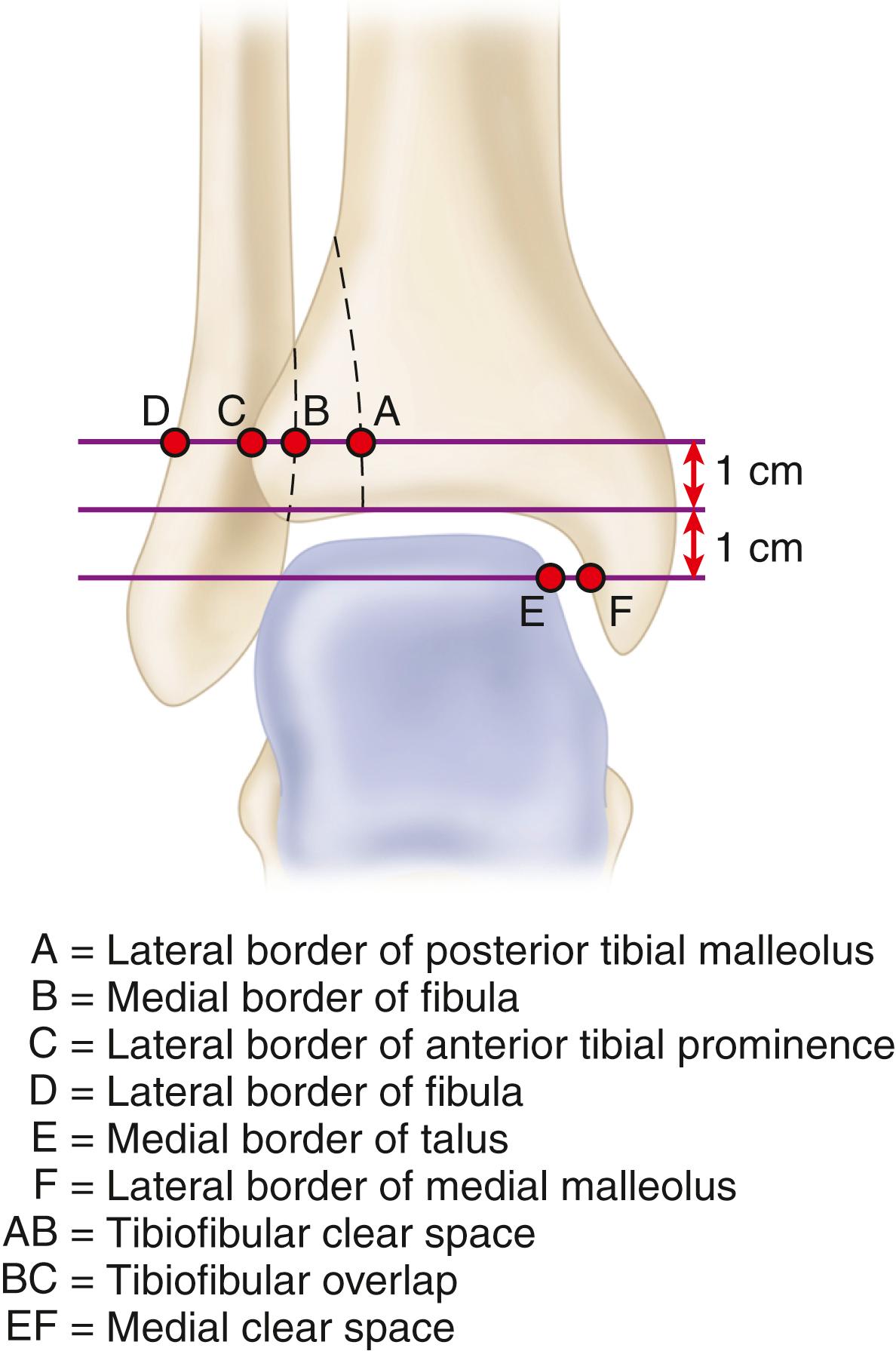
More powerful and three-dimensional MRI studies have allowed for greater accuracy in the diagnosis of ankle and hindfoot injuries. Axial MRI with a local gradient provides optimal views of the anterior and posterior talofibular ligaments and the deep layers and tibionavicular component of the deltoid ligament, whereas MRI coronal imaging allows a complete view of the calcaneofibular, posterior talofibular, tibiocalcaneal, and posterior tibiotalar ligaments. In both imaging planes, differentiation of the deep and superficial layers of the medial collateral ligament, as well as between the syndesmotic complex and the lateral collateral ligaments, was possible. Nielson et al. found no correlation between tibiofibular clear space and overlap measurements in patients with syndesmotic injuries seen on MRI ( Fig. 90.7 ). A medial clear space measurement of more than 4 mm correlated with disruption of the deltoid and tibiofibular ligaments ( Fig. 90.8 ).
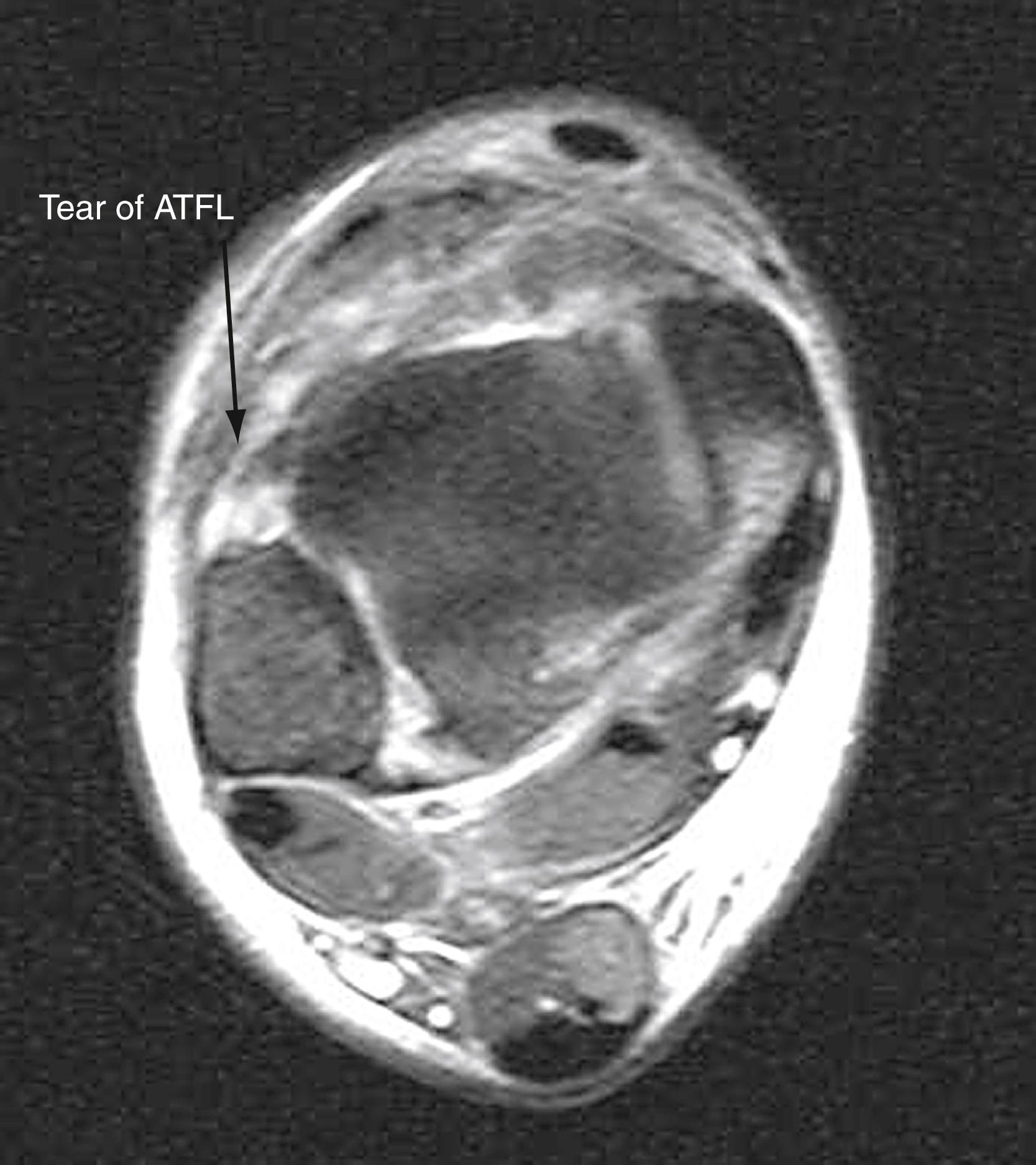
MRI has been shown to be more specific than sensitive, especially as it relates to the calcaneofibular ligament. Note that bone bruises occur in a significant number of ankle sprains and that multiple bone bruises occur more frequently in patients with multiple ligaments injured. Although bone bruise–like lesions may be seen at an average of 8.4 weeks, they often are present more than 1 year after injury. MRI has been shown to be effective by several authors in identifying and differentiating lateral ankle ligament injuries; however, many believe that the costs outweigh the benefits. If a peroneal pathologic process is suspected, MRI may be beneficial, but it is not routinely necessary to diagnose lateral ligament injury.
Most type I and type II sprains or ligamentous injuries can be treated by functional bracing and early rehabilitation. This treatment allows stretched and attenuated ligaments to be in reasonable anatomic alignment and length during the healing process. Although immobilization quickly relieves pain and may be beneficial in reducing the swelling, early mobilization for these injuries produces results that are superior to immobilization. Proprioceptive training after usual care appears beneficial as well. Regardless, most sprains do not need surgical repair. Even patients with complete grade III tears may obtain good results with functional treatment consisting of a short period of protection with taping or bracing that allows early weight bearing, followed by functional range-of-motion exercises and neuromuscular training of the ankle . High-demand patients will benefit from a sport-specific rehabilitation program developed with the collaboration of the physician, trainer, therapist, and coaches. Advantages of this method include quick recovery of functional range of motion and early return to work and physical activity. However, acute surgical intervention may improve long-term results if instability is present clinically and radiographically. Secondary operative reconstruction or delayed repair of the ruptured ligaments can be done years after the injury if necessary, and the results may be comparable with primary repair. Competitive athletes can be treated functionally, although 10% to 20% require later secondary repair. Although functional treatment avoids the additional trauma to the tissues and complications inherent in surgical treatment, in high-demand patients with clinical and radiographic instability, acute surgical intervention is a reasonable approach. Indications for surgical treatment are large bony avulsions, unstable osteochondral injuries, severe ligamentous incompetence on the medial or lateral sides of the ankle, and recurrent ankle injuries.
The goal of treatment is to prevent chronic instability of the ankle. A 1-mm lateral shift of the talus in the mortise has been shown to produce a 42% reduction in the area of contact between the tibia and the talus. Because stress per unit area increases as the total contact area decreases, displacement may contribute to a poor result and give support to the contention that joint instability leads to traumatic arthritis. Ankle instability may result from fracture or ligamentous injury or a combination of both, and what may appear at the ankle to be a pure ligamentous injury with talar shift may include a fracture of the proximal fibula (e.g., Maisonneuve fracture).
In active patients, acute ruptures of the deltoid ligament, shown by abnormal tilt or shift of the talus in the ankle mortise and a palpable defect in the ligament, usually should be repaired. Often, the lateral malleolus is fractured or the distal tibiofibular joint is disrupted ( Fig. 90.9 ). Crim et al., in a review of patients with chronic lateral ankle instability, found that 72% had an injury of the deltoid ligament as seen on MRI; 43% of all patients had injuries to both the deep and superficial components. Isolated partial ruptures of the deltoid ligament have been reported, but isolated complete ruptures are rare. Varus and valgus stress testing may show some widening of the clear space of the medial malleolus and some tilting of the talus in deltoid ligament rupture without fracture, and comparison MRI can determine the extent and location of the deltoid tear. For isolated complete disruption, immobilization in a below-knee, non–weight bearing plaster cast for 4 to 6 weeks, followed by use of a molded shoe orthosis for 4 to 6 months, has been recommended. Surgical exploration for patients with evidence of significant displacement at the time of injury is often warranted. This condition should not be confused with isolated rupture of the posterior tibial tendon, which also causes medial ankle pain in pronation.
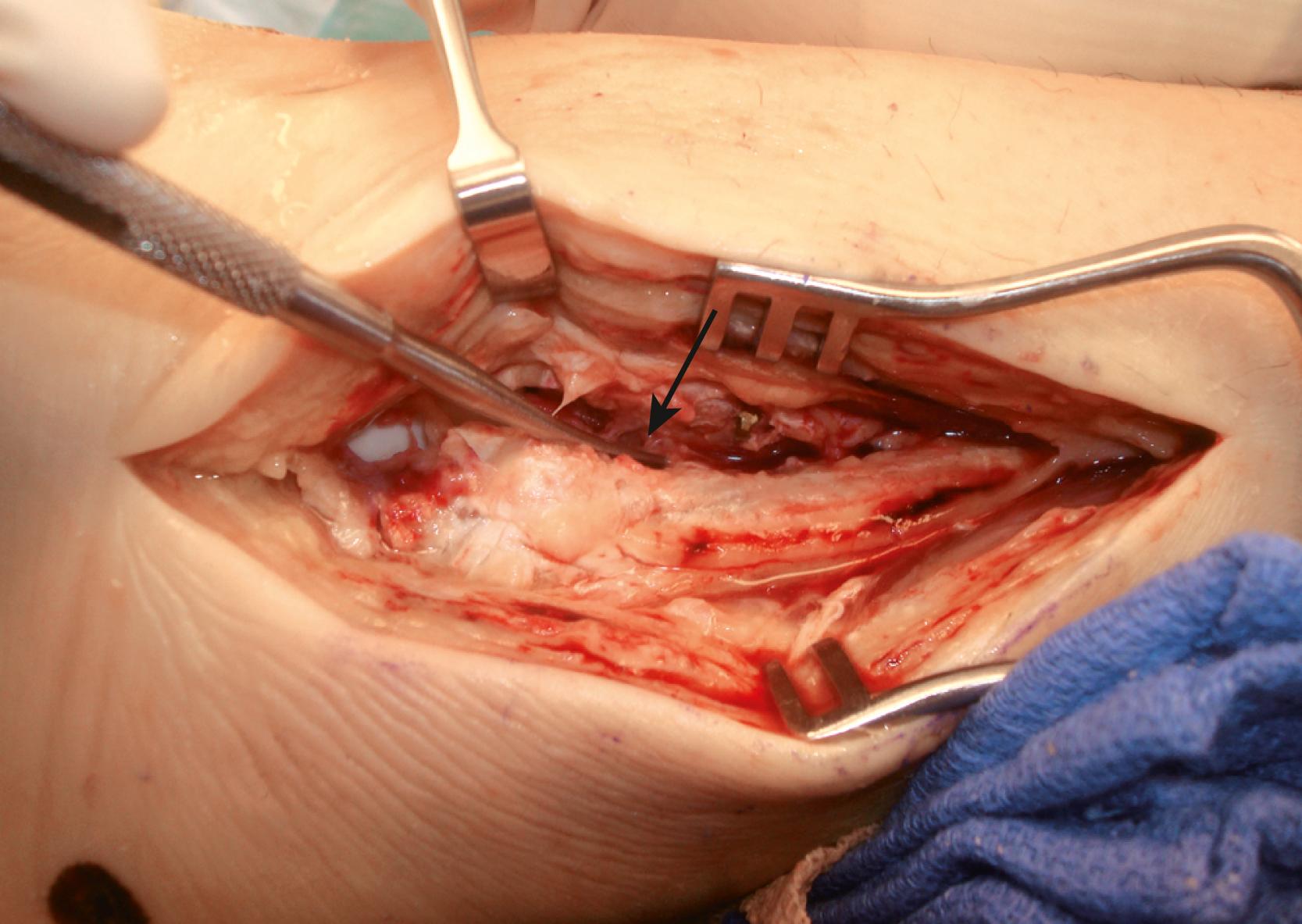
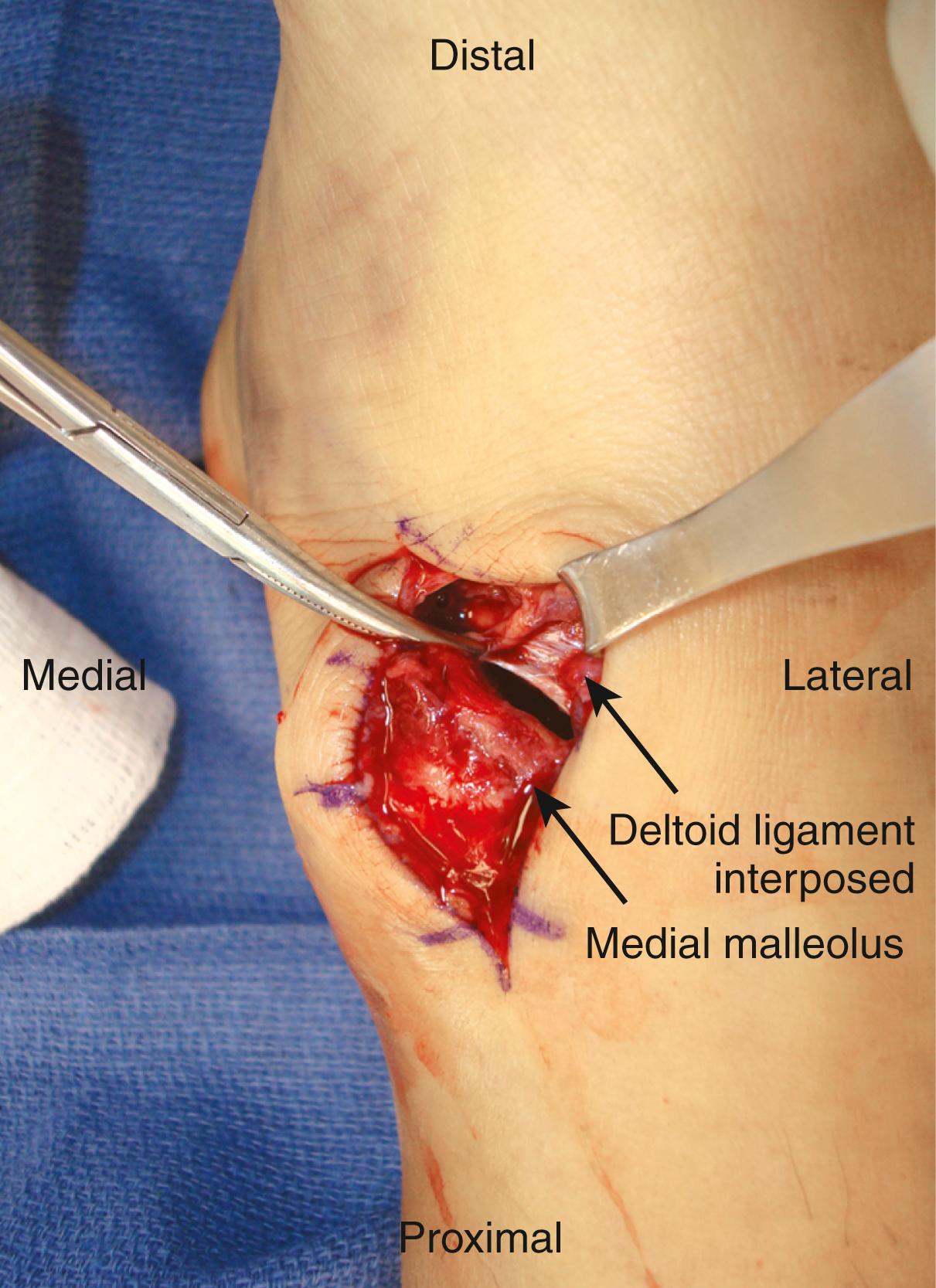
Satisfactory functional results have been reported after surgical treatment in patients with complete disruption or incompetency of the deltoid ligament, without deltoid repair as part of the initial operation as long as surgical reduction of the medial joint space and lateral malleolus was accurate and maintained until bone repair was complete. Hsu et al. reviewed 14 cases of direct repair of the deltoid ligament in professional American football athletes after ankle fracture fixation. Each patient underwent a dynamic arthroscopic examination with removal of loose bodies and debridement of osteochondral lesions as indicated followed by fixation of the lateral malleolar fracture. The deltoid ligament was then repaired directly by approximating the tibionavicular and tibial calcaneal portion of the deltoid to its native attachment on the medial malleolus. Each patient followed a standard postoperative rehabilitation protocol. Good results were noted in these high-performance athletes after this treatment regimen. Note that the posterior tibial tendon or the proximal end of the avulsed deltoid ligament may be caught between the medial malleolus and the talus with attempted reduction of the laterally displaced talus (see Fig. 90.9 ). The technique of repair of acute rupture of the deltoid ligament is described in Chapter 54 .
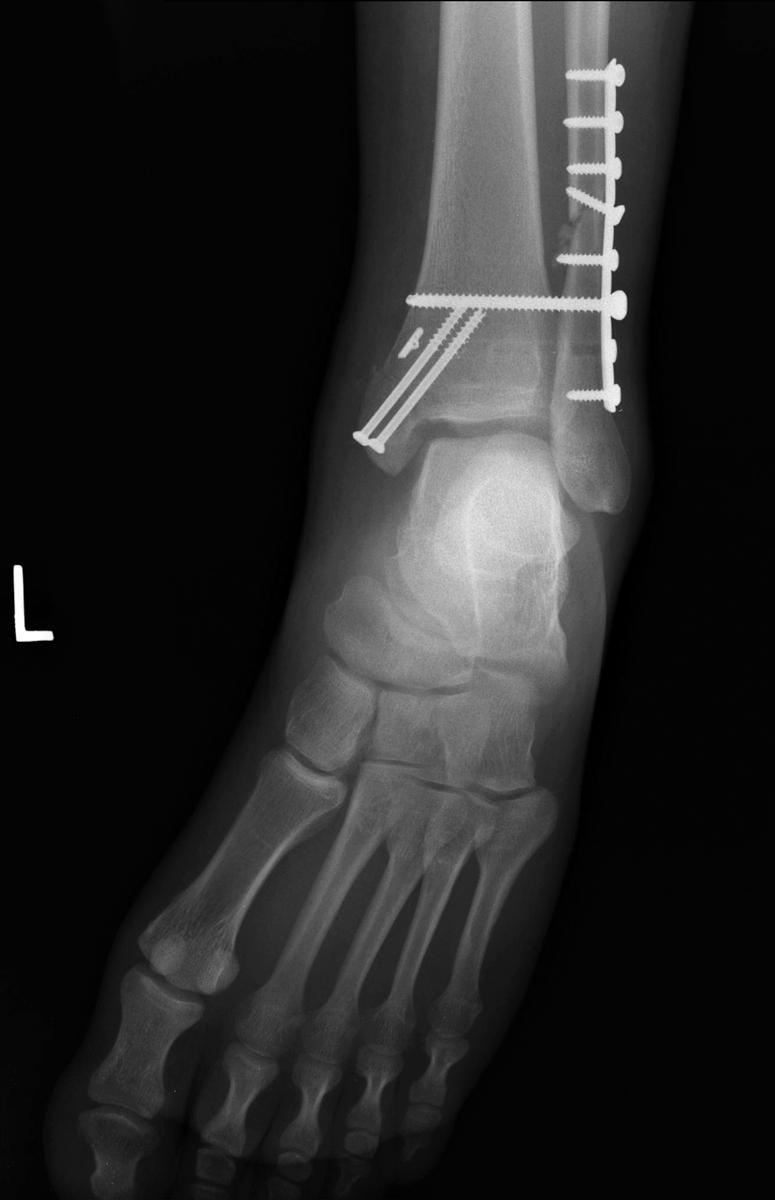
When the ligaments binding the distal tibia to the fibula are ruptured, the medial malleolus usually is fractured or the fibula is fractured proximal to the lateral malleolus or both injuries may occur. Occasionally, however, the associated injury is rupture of the deltoid ligament. Syndesmotic sprains reportedly account for approximately 1% of all ankle injuries and 18% of all ankle sprains; however, because diastasis is rare in isolated injuries, this may be underreported. Male sex and higher level of competition are risks factors for syndesmotic ankle sprain during athletics. Diastasis after an isolated syndesmotic injury is rare, and rupture of the ligaments of the distal tibiofibular joint usually can be treated by closed methods. However, if widening of the ankle mortise remains after manipulation, surgery is necessary ( Fig. 90.10 ). In surgically treated syndesmosis injuries, malreduction results in poor functional outcomes. Open reduction of the syndesmosis results in a significantly lower incidence of malreduction compared with closed reduction with percutaneous fixation ( Fig. 90.11 ). In patients treated operatively and with acceptable risks for a larger incision, we advocate open treatment of the syndesmosis. Direct visualization or palpation of the syndesmosis has been shown to be equally effective in achieving syndesmotic reduction, but neither method is perfect. If the ankle mortise was dislocated or significantly subluxed, we recommend routinely opening it medially with sweeping of the medial clear space and repair of the deltoid ligament as necessary.
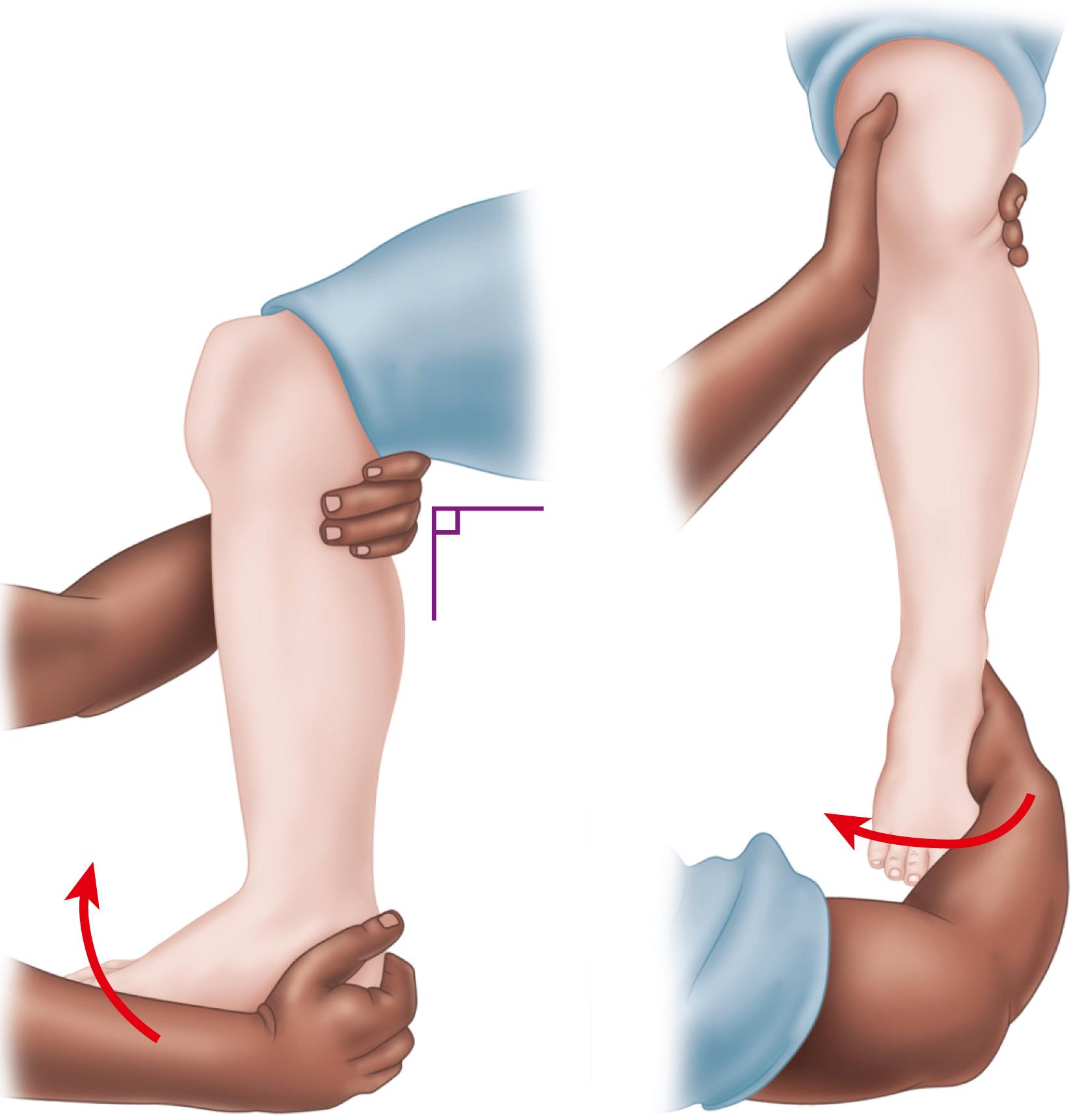
Several authors have described the sequelae of syndesmosis ankle sprains in military cadets and professional and college football players. They concluded that this is a more serious injury with a longer recovery time than a third-degree lateral ankle sprain. Accurate diagnosis of a syndesmosis sprain can be made by a positive squeeze test ( Fig. 90.12 ), but this should be done only after other injuries to the leg are ruled out by examination and radiographs. According to the study by Teitz and Harrington, compression (squeezing) of the calf caused separation of the distal fibula and tibia. External rotation stress testing ( Fig. 90.13 ) also is helpful in making the diagnosis. At follow-up, many patients in these series had developed ossification of the syndesmosis ( Fig. 90.14 ); however, in the absence of frank synostosis, functional ankle results were excellent or good. Chronic ankle instability did not seem to result from the syndesmosis sprains, but recurrent sprains were common if heterotopic ossification occurred. In some patients, syndesmosis ossification may be symptomatic, thus requiring surgical excision. Yasui et al. reported good results with anatomic reconstruction of the anteroinferior tibiofibular ligament using an autologous gracilis tendon in six patients with chronic disruption of the syndesmosis after a pronation and external rotation type IV injury. Surgical fusion of the syndesmosis may be required in patients with chronic instability.


Most authors have advocated the use of metal screws or suture buttons for the stabilization of syndesmotic injuries with persistent diastasis. The outcomes with titanium or stainless steel screws, as well as with tricortical or quadricortical fixation, have not been shown to be significantly different. Although 4.5-mm screws have not demonstrated improved biomechanical properties when placed in a tricortical fashion, they have demonstrated improved resistance to shear stress on the distal tibiofibular joint when placed across four cortices. More recent literature indicates that suture button fixation of the syndesmosis may result in improved American Orthopaedic Foot and Ankle Society (AOFAS) scores, lower postoperative complications, and earlier time to full weight bearing. Ideal placement of the fixation device has not been established. We advocate placement of the screw or suture button 3 cm proximal and parallel to the distal tibial articular surface (just proximal to the incisura), angled 20 to 30 degrees anteromedially and starting on the posterolateral aspect of the fibula. In theory suture button fixation ( Fig. 90.15 ) provides secure, but not rigid, fixation of the syndesmosis, allowing for spontaneous reduction of the syndesmosis even if there is mild initial malreduction .

Hardware removal is common for both screw and suture button techniques. A review found that approximately 50% of screws and 10% of suture buttons require removal. When screw removal is planned, it most often is done before full weight bearing, 3 to 4 months after the initial procedure. Screw breakage, button subsidence, and early or late loss of reduction have been reported as some of the most common complications after surgical repair of the syndesmosis. Our institution favors suture button fixation in active individuals, allowing for earlier weight bearing and obviating the need for routine implant removal. Alternatively, the syndesmosis can be directly repaired through fixation of bony avulsion injuries or suture anchor repair. We do not recommend suture button fixation when the fibular fracture is not rigidly fixed (e.g., Maisonneuve fractures). Suture fixation allows for a small amount of motion and may result in the fibula healing slightly shortened.
Position the patient supine with a bump under the ipsilateral hip. A more lateral decubitus position with a beanbag may be necessary to visualize the posteroinferior tibiofibular ligament, if desired. External rotation of the hip allows access to the medial structures as needed.
Place a bolster under the ankle while allowing the heel to “float” off the operating table. This will prevent anterior subluxation of the talus on the tibial plafond.
Make an incision 5 cm long parallel to the anterior border of the distal fibula, and expose the distal tibiofibular joint.
Press the fibula into the groove in the tibia (incisura fibularis) to shift the fibula and the talus medially into normal position. With this technique, suturing or reattaching the ligaments is unnecessary.
Once reduced, maintain the syndesmosis in position with a large clamp under gentle compression (if the mortise is anatomically reduced, a clamp may be unnecessary) and ensure that the fibula does not sublux or rotate. Use intraoperative fluoroscopy to further assess fibular position and reduction of the syndesmosis and ankle mortise.
Under fluoroscopic visualization, drill an appropriate-sized tunnel for placement of either a screw or a suture button. This can be placed through a fibular plate or directly against the fibula. A plate may decrease the risk of a stress injury or implant subsidence but may increase lateral irritation. Direct the drill in a 25% anteromedial direction beginning on the posterior aspect of the fibula. Drill 3 cm proximal and parallel to the tibial plafond. Combined use of a metal screw and a suture button provides rigid fixation for 10 to 12 weeks and protects against late loss of reduction.
If the screw is to be removed, placement across four cortices may facilitate retrieval should the screw break ( Fig. 90.16 ).
Check the position of the implant and the reduction of the talus by radiographs in the operating room to ensure that the talus has been replaced precisely against the medial malleolus; if not, it is likely that some soft structure, such as a tendon or the deltoid ligament, is obstructing reduction ( Fig. 90.17 ) (see discussion of irreducible fracture or fracture-dislocation of the ankle in Chapter 89 ).
For an associated proximal fibular fracture, apply a small, lightweight, semitubular plate to fix the fracture. One of the screws for the plate on a more distal fracture can be used to transfix the distal tibiofibular joint. This AO technique is described in Chapter 53 .
Position the patient as described previously.
Repair lateral malleolar injury as needed.
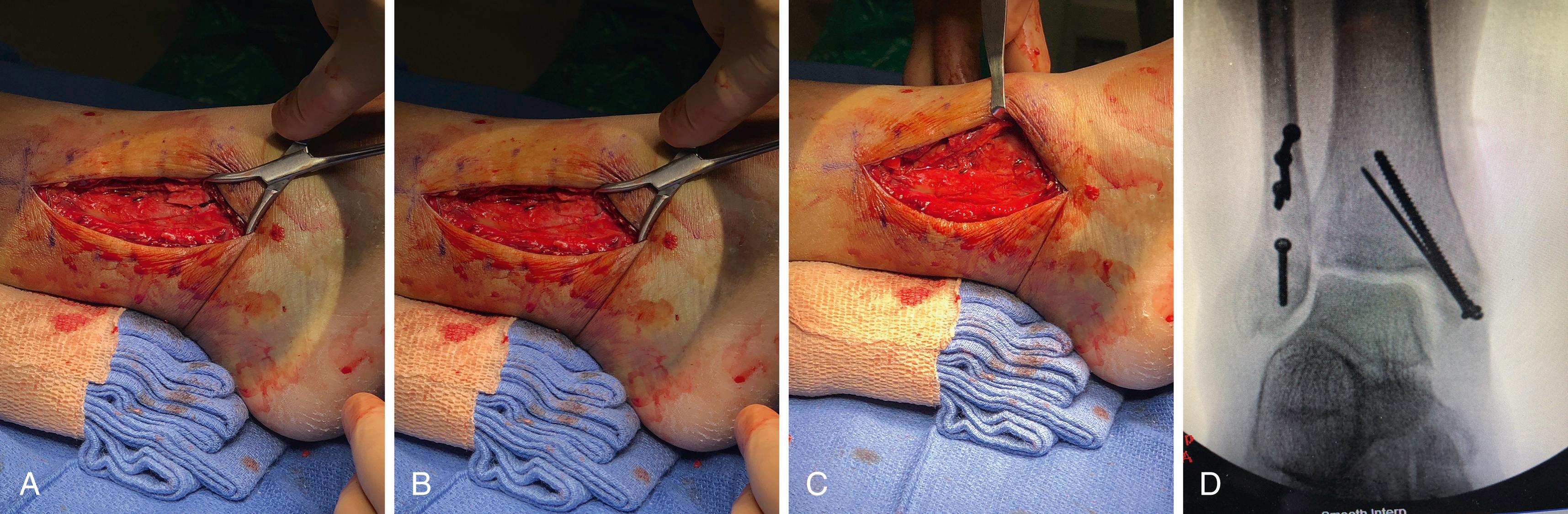
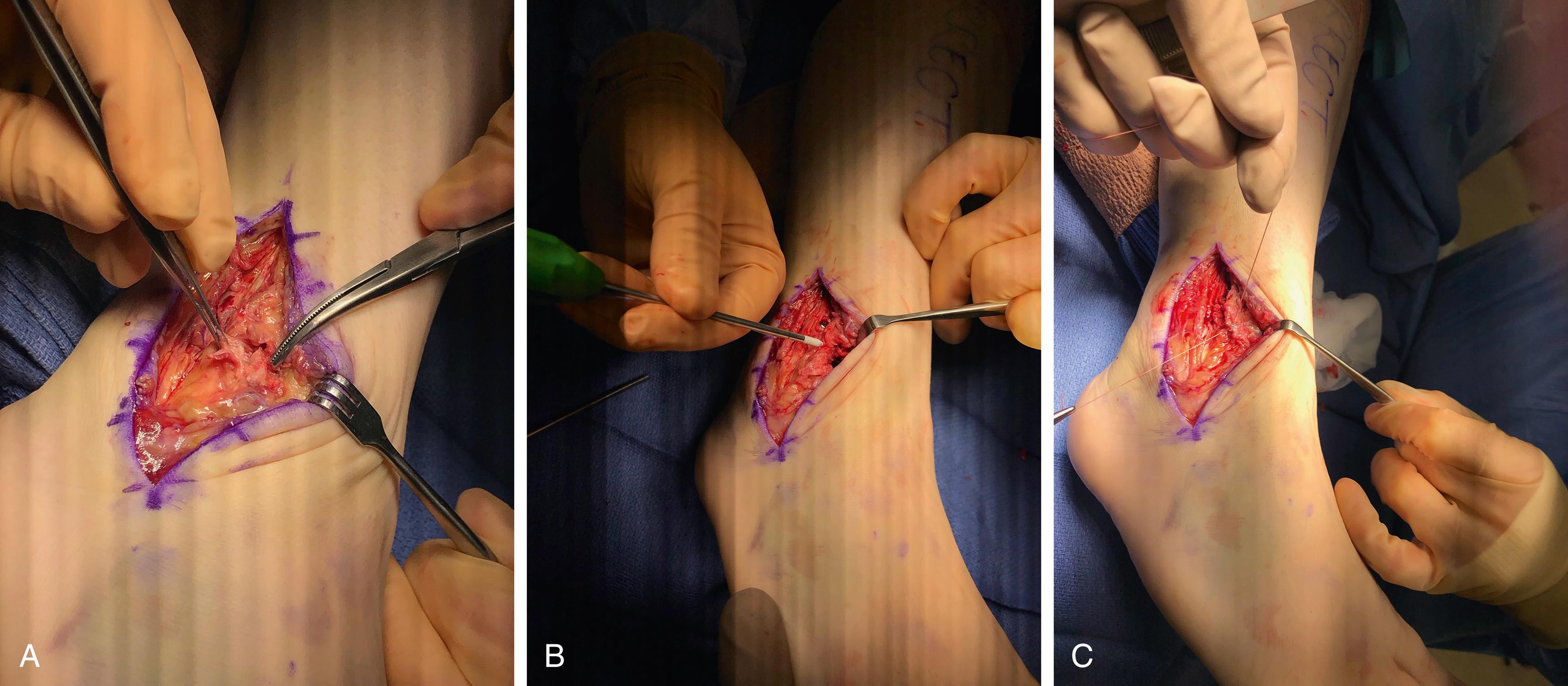
If syndesmotic instability is associated with a bony avulsion, attempt bony fixation because this will provide a stronger repair ( Fig. 90.18A-D ). If the fragment is too small to allow for bony fixation, excise it and place a suture anchor at the fibular or tibial footprint of the anteroinferior tibiofibular ligament or posteroinferior tibiofibular ligament, as indicated ( Fig. 90.19A-C ).
A splint is applied from the base of the toes to the tibial tuberosity. At 2 weeks, the splint is removed, and a cast is applied and worn for an additional 3 weeks. At 5 weeks, a walking boot is placed and the patient is instructed on active, touch-down–weight-bearing range-of-motion exercises. Weight bearing in the boot is begun at 8 to 10 weeks. The boot is worn until the screw (if used) is removed at 14 weeks postoperatively. Weight bearing should be limited until/if hardware is removed because it may become loose or break within the tibiofibular joint.
The anterior talofibular ligament is the most important stabilizing ligament of the ankle; however, isolated rupture of the anterior talofibular ligament can be treated by immobilization. Although 10% to 20% of athletes may have chronic symptoms related to an ankle sprain, the cause of functional instability of the ankle after injury of the ligaments is unknown. After healing of a ruptured anterior talofibular ligament, some patients still have lateral pain and swelling even though they can return to full activity. It has been postulated that the presence of a localized synovitis, painful scar in the ligament, weakness of the peroneal musculature, or even a proprioceptive deficit involving the nerves of the ankle joint may be the cause of residual symptoms. Articular cartilage lesions also may cause pain after healing or stabilization of the joint. Intraarticular chondral lesions larger than one half the thickness of the articular cartilage and more than 5 mm in diameter are associated with postoperative pain, indicating that ligament reconstruction alone may not relieve pain if large intraarticular lesions are present and that the two problems (ligamentous insufficiency and intraarticular lesion) must be evaluated and treated separately.
When at least two of the lateral ligaments, the anterior talofibular and the calcaneofibular, are torn, support exists for surgical repair. Disruption of the calcaneofibular ligament results in de facto alterations to subtalar joint kinematics, although the literature suggests repair is not always required. Several authors have reported better results with acute surgical repair of ruptured lateral ligaments, especially in young athletic patients. One study of 388 patients randomized to functional treatment (taping or elastic bandaging, followed by functional rehabilitation) or operative treatment found that the risk of giving way, recurrent sprains, and residual pain was reduced in the surgically treated group. There was no difference in swelling, subjective outcome, or return to sports. Despite the better results, the authors did not recommend routine primary repair of the lateral ankle ligaments, partly because of the higher costs involved and the risk of complications associated with surgery. In other series of patients, not necessarily athletes, operative repair resulted in a higher incidence of early complications that slightly delayed the patients’ return to work, and there was no evidence that operative repair offered improved symptomatic or functional benefit. A comprehensive literature evaluation and meta-analysis concluded that conservative treatment of acute lateral ligament tears results in outcomes similar to those with surgical treatment. The excellent results found after delayed repairs or reconstruction of the lateral ligaments perhaps allow for a more conservative approach to acute injuries. Conservative treatment should consist of functional therapy. Rest, ice, compression, and elevation (RICE) should begin immediately after injury. In most instances, a functional brace should be placed and physical rehabilitation begun as soon as weight bearing is tolerated. Athletes with a significant ligament injury should consider the indefinite use of a functional brace because they are at increased risk of recurrent sprains.
Several authors have reported good results with the Gould modification of the Broström procedure. This modification includes mobilization and reattachment of the lateral portion of the extensor retinaculum to the tip of the fibula after direct capsular reefing or repair of the anterior talofibular and calcaneofibular ligaments as originally described by Broström.
If the lateral ligaments are significantly disrupted, of the patient demonstrates hyperlaxity or weighs more than 240 lb, we often add suture tape augmentation over the primary repair.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here