Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Spondylolisthesis refers to ventral displacement of the proximal spinal column in relation to the distal spinal column. The degree of slip is determined by measuring the amount of anterior translation of the displaced vertebra relative to the superior aspect of the inferior vertebra and is expressed as a percentage. The Meyerding Classification grades translational displacement as:
Grade 1: 1%–25%
Grade 2: 26%–50%
Grade 3: 51%–75%
Grade 4: 76%–100%
Grade 5: slippage of the L5 vertebra anterior and distal to the superior S1 endplate (spondyloptosis)
Slippages <50% are referred to as low-grade spondylolisthesis, while slippages >50% are referred to as high-grade spondylolisthesis.
The Wiltse Classification identifies type of spondylolisthesis based on a combination of etiologic and anatomic features:
Type 1: Dysplastic . Associated with a congenital deficiency of the L5–S1 articulation
Type 2: Isthmic . Associated with a lesion in the pars interarticularis (type 2A: stress fracture; type 2B: elongated but intact pars interarticularis; type 2C: acute pars fracture)
Type 3: Degenerative . Disc degeneration and facet arthrosis lead to spondylolisthesis and associated spinal stenosis in adults
Type 4: Traumatic . An acute fracture in a region of the posterior elements other than the pars interarticularis (e.g., facets, pedicle, lamina)
Type 5: Pathologic . Generalized bone disease (e.g., metabolic, neoplastic) results in attenuation of the pars and/or pedicle region leading to spondylolisthesis
Type 6: Postsurgical . Spondylolisthesis that develops following lumbar laminotomy or laminectomy
The Marchetti and Bartolozzi Classification identifies two major types of spondylolisthesis: developmental and acquired. Developmental spondylolisthesis is associated with dysplasia at the level of the spondylolisthesis and is subdivided into high- and low-dysplastic types. Acquired types of spondylolisthesis include traumatic, degenerative, pathologic, and postsurgical etiologies.
The Spinal Deformity Study Group Classification of Spondylolisthesis was developed to incorporate the current understanding of sacropelvic and global spinopelvic balance as a guide to treatment decision making. Classification of L5–S1 spondylolisthesis is based on three factors:
Degree of slip (low grade or high grade),
Sacropelvic alignment and balance, and,
Global spinopelvic balance.
Low-grade spondylolisthesis is stratified into three types based on pelvic incidence (PI):
Type 1 (low PI, <45°),
Type 2 (normal PI, 45°–60°) and
Type 3 (high PI, >60°).
Type 1 patients have low PI, which results in low shear stress across the lumbosacral junction and low risk of slip progression. In contrast, type 3 patients have high PI, which increases shear stress across the lumbosacral junction and increases the risk of spondylolisthesis progression.
High-grade spondylolisthesis is subdivided into three types:
Type 4 (balanced pelvis)
Type 5 (retroverted pelvis with a balanced spine)
Type 6 (retroverted pelvis with an unbalanced spine)
In a balanced pelvis, sacral slope (SS) exceeds pelvic tilt (PT) (i.e., high SS/low PT). In contrast, in an unbalanced pelvis, there is a low sacral slope and a high pelvic tilt (i.e., low SS/high PT) and the pelvis becomes retroverted and the sacrum becomes vertically oriented. Global spinopelvic balance is assessed by the position of the C7 plumb line. The spine is considered balanced when the C7 plumb line is located through or behind the femoral heads and unbalanced when the C7 plumb line is located anterior to the femoral heads. Surgery to restore sagittal alignment through reduction and realignment procedures is recommended for type 5 and type 6 deformities ( Table 53-1 ; Fig. 42.6 ).
| SLIP GRADE | SACROPELVIC ALIGNMENT/BALANCE | SPINOPELVIC BALANCE | SPONDYLOLISTHESIS TYPE |
|---|---|---|---|
| Low grade | Low pelvic incidence (<45°) | - | Type 1 |
| Normal pelvic incidence (45°-60°) | - | Type 2 | |
| High pelvic incidence (>60°) | - | Type 3 | |
| High grade | Balanced sacropelvis | - | Type 4 |
| Unbalanced (retroverted) sacropelvis | Balanced | Type 5 | |
| Unbalanced (retroverted) sacropelvis | Unbalanced | Type 6 |
Ninety percent of cases of isthmic spondylolisthesis occur at the L5–S1 level. The next most commonly affected level is L4–L5.
The clinical presentation of adults with isthmic spondylolisthesis is quite variable. Adult isthmic spondylolisthesis occurs more commonly in males than females. The prevalence of isthmic spondylolisthesis in adults with and without low back pain has been reported as 10.8% and 7.3%, respectively. Symptomatic adult patients with isthmic spondylolisthesis most commonly present with low back pain and over half of patients present with lower extremity radicular pain. Symptomatic adults present most commonly with low-grade slips. Patients with high-grade slips are more commonly encountered during adolescence, but occasionally present in adulthood due to new-onset or worsening symptoms or for evaluation following prior surgical treatment. Spondylolysis and low-grade isthmic spondylolisthesis that have been asymptomatic since childhood may become symptomatic in later life in the absence of precipitating trauma. As the ability of the intervertebral disc to resist shear forces at the level of the pars defect is compromised, spondylolisthesis progression may occur as degenerative disc changes develop, most often during the fourth and fifth decades of life.
It is critical to precisely localize the pain generator in adult patients with spondylolisthesis because pain may not be related to the level of the spondylolisthesis, but rather due to degenerative spinal pathology at adjacent spinal levels, or extraspinal causes such as hip or knee arthritis.
A standing lateral spinal radiograph is the initial imaging study required for diagnosis of spondylolisthesis in adult patients. Magnetic resonance imaging (MRI) is used to evaluate neural compression and assess the status of the lumbar discs. Computed tomography (CT) is the method of choice for assessing osseous anatomy. Patients who are surgical candidates require a standing lateral full-length spinal radiograph to assess sagittal alignment and global balance.
Nonsurgical treatment options include active physical therapy, education, and instruction in a home exercise program, nonsteroidal antiinflammatory medication, and bracing. Epidural injections are a treatment option for patients with isthmic spondylolisthesis and clinically significant lower extremity radicular symptoms.
Surgery is infrequently required for adult patients with spondylolysis or isthmic spondylolisthesis. General indications to consider surgical intervention include:
Failure of nonsurgical treatment for disabling back and/or leg pain
Patients with symptomatic and radiographically unstable isthmic spondylolisthesis
Documented slip progression (> grade 2 slip)
Symptomatic grade 3 or 4 spondylolisthesis or spondyloptosis
Associated symptomatic spinal stenosis or progressive neurologic deficit
Cauda equina syndrome related to spondylolisthesis
L5 nerve root compression (exiting nerve root of the L5–S1 motion segment) is the type of neural compression most commonly associated with L5–S1 isthmic spondylolisthesis. L5 nerve root compression may occur secondary to:
Hypertrophy of fibrocartilage at the site of the pars defect
Compression in the foraminal zone as the L5 nerve root is compressed between a disc protrusion or osteophyte and the inferior aspect of the L5 pedicle
Compression between the inferior aspect of the L5 transverse process and the superior aspect of the sacral ala
Increased tension within the L5 nerve root may occcur due to forward displacement of the L5 vertebra when the L5 nerve root is tethered by a hook-like projection from the lamina at the inlet to the intervertebral foramen.
The sacral nerve roots can become involved in high-grade isthmic spondylolisthesis as these nerves become stretched over the L5–S1 disc and posterior aspect of the sacrum.
No. Adult patients with symptomatic spondylolysis have poorer healing potential compared with pediatric patients, and additional pain generators within the spinal motion segment other than the pars interarticularis are often responsible for back and/or leg pain symptoms. Spinal fusion is recommended for treatment of symptomatic spondylolysis that does not respond to nonoperative treatment.
Potential surgical treatment options for low-grade isthmic spondylolisthesis include:
L5–S1 decompression
Decompression and in situ posterolateral fusion with or without posterior pedicle fixation
Decompression, posterolateral fusion, and posterior pedicle fixation combined with interbody fusion
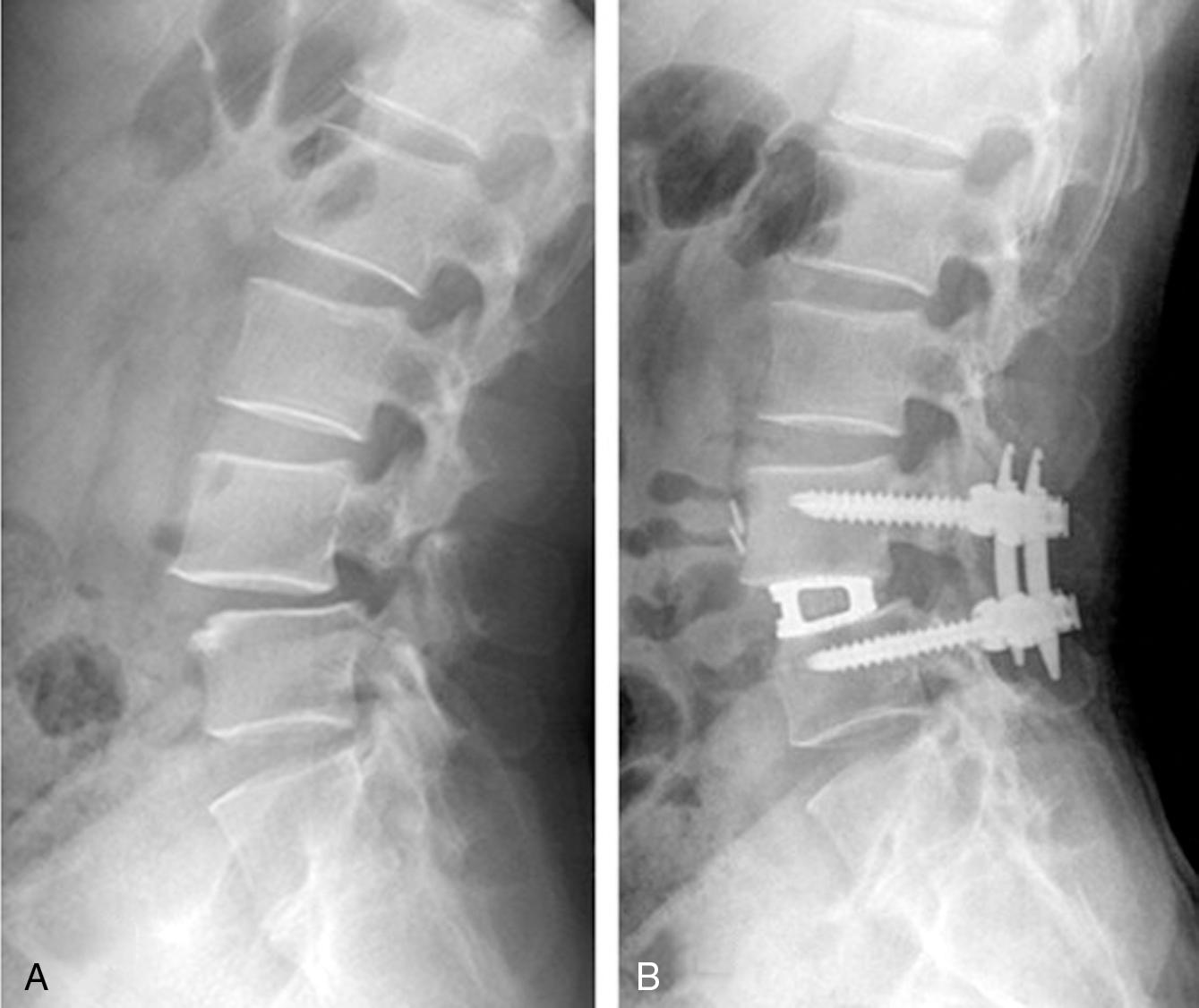
Lack of consensus exists regarding the optimal procedure for treatment of low-grade L5–S1 isthmic spondylolisthesis. Posterior decompression without fusion is rarely performed due to the high risk of postoperative slip progression. Adult patients are frequently treated with posterior spinal fusion in combination with pedicle fixation and direct neural decompression. The rationale for use of posterior spinal instrumentation is to decrease the risk of postoperative slip progression and increase fusion rates. Some surgeons prefer to perform posterior fusion without direct neural decompression in the absence of severe neurologic deficits to preserve greater osseous surface area for posterior fusion. Other surgeons advocate posterior fusion without use of instrumentation for low-grade slips. The addition of an L5–S1 interbody fusion is advocated by many surgeons and may be performed through a variety of approaches including transforaminal lumbar interbody fusion (TLIF), posterior lumbar interbody fusion (PLIF), and anterior lumbar interbody fusion (ALIF). Rationale for use of interbody fusion includes increased fusion surface area, which is expected to increase fusion rates; restoration of disc space height, which increases neuroforaminal height and provides indirect neural decompression; and increased segmental stability provided by anterior column support, which reduces stress on posterior spinal implants and promotes early patient mobilization ( Fig. 53.1 ). Use of stand-alone anterior lumbar interbody fusion and supplemental anterior fixation is reported for treatment of adult low grade isthmic spondylolisthesis. However, notable complications have been described with this strategy including pseudarthrosis, instrumentation failure and sacral fracture due to the coexistence of high anterior column shear forces in the presence of a posterior tension band defect.
Surgical treatment options for high-grade isthmic spondylolisthesis include:
In situ posterolateral L4–S1 spinal fusion in combination with posterior spinal instrumentation and spinal decompression.
Circumferential fusion consisting of posterolateral L4–S1 fusion and posterior spinal instrumentation, spinal decompression, L5–S1 interbody fusion, and partial or complete reduction of spondylolisthesis.
Circumferential fusion consisting of posterolateral L4–S1 spinal fusion and instrumentation, spinal decompression and transsacral interbody fusion and fixation ± partial reduction of spondylolisthesis.
L5 vertebrectomy (Gaines procedure) for spondyloptosis
Surgery that restores sagittal alignment through reduction and realignment procedures is recommended for type 5 and type 6 deformities based on the Spinal Deformity Study Group Classification of Spondylolisthesis. Interbody fusion through either an anterior or posterior approach and use of distal fixation consisting of either S2 alar-iliac screw fixation or iliac screw fixation are integral to the success of reduction procedures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here