Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since the 1970s, when spinal cord stimulation (SCS) first came into widespread clinical use, its most common application has been management of persistent pain following low back surgery, commonly known as the failed back surgery syndrome (FBSS). It was asserted at that time ( ), and has been accepted previously, that covering the topography of pain with stimulation paresthesia, at subjectively comfortable or tolerable stimulation amplitudes, is a necessary condition for achieving pain relief. Covering the low back with stimulation paresthesia has proven to be more difficult than covering the lower extremities in the average patient, and for many years patients with a chief complaint of radiating lower extremity pain, as opposed to axial low back pain (LBP), have been considered to be more amenable to treatment with SCS ( ; ).
In previous studies, the only two randomized controlled trials (RCTs) of SCS for FBSS reporting long-term clinical outcomes included subjects with radiating leg pain, exceeding or, at a minimum, equaling LBP ( ). These studies showed that the results of SCS were superior to repeated low back surgery and to conservative medical management. These studies could not be generalized, however, to patients with a chief complaint of LBP, to which this chapter will give particular attention.
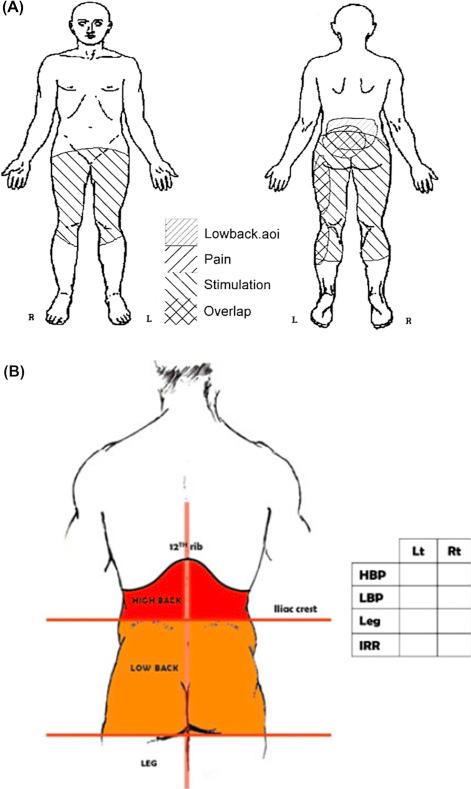
The words “low back pain” are often used as though their meaning is unambiguous, but when definitions have been published, they vary significantly. As shown in Fig. 50.1A and B , for example, published pain drawings show that the “low back,” on one side of the Atlantic, might include part of the “high back” (above the iliac crests) and, on the other side, the low back extends down to the gluteal folds ( ). Most often the phrase is simply undefined. Comparisons among studies should be made with this in mind.
Notwithstanding the relative difficulty reported by many authors, some have reported that with careful attention to SCS electrode placement on the physiologic midline and adjustment of stimulation parameters, low back coverage can be achieved in most patients ( ). Law introduced the concept of “range of stimulation” to describe the clinically useful amplitudes, beginning at perceptual threshold and extending up to discomfort (or motor) threshold, as shown in Fig. 50.2 ( ).
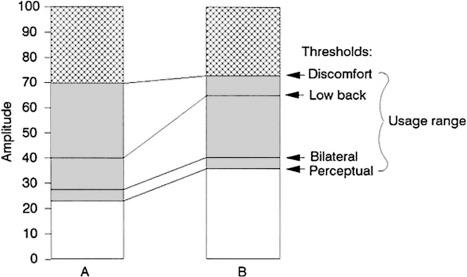
Quantitative comparisons of performance may be made between different configurations (e.g., different contact positions, different pulse widths), with respect to such measures as coverage of an area of pain, e.g., the low back. To achieve coverage in the midline, Law went on to introduce the concept of placing two percutaneous multicontact electrodes in parallel, one on either side of the midline, and then making adjustments after implantation to achieve symmetry ( ) This can be less demanding and time-consuming, and more forgiving of electrode migration or malposition, than placing one electrode precisely in the midline.
The routine practice of temporary percutaneous electrode placement for an SCS trial, which if successful is followed by permanent electrode implantation, has made it possible to do controlled trials comparing different electrode designs, in which each patient serves as his or her own control and the temporary and permanent electrodes are implanted in exactly the same location. We compared two 4-contact columns with one column in this fashion in FBSS patients with a chief complaint of LBP, and we found that two columns were in fact inferior to one: scaled to the range from first perception to discomfort (see Fig. 50.2 ), the amplitude required to achieve low back coverage was higher (i.e., closer to discomfort threshold and therefore technically inferior) for the two-column configuration ( ).
Technical results aside, the clinical outcomes for the two-column system, in patients with chiefly LBP compared favorably with SCS results in general, and in FBSS in particular, as reported previously in patients with primarily leg pain: the rate of successful trials was 91%, and at 2.3-year follow-up the long-term rate of success (at least 50% pain relief plus patient satisfaction with outcome) was 53%.
In another study comparing electrode designs, this time an RCT, we showed advantages for an insulated paddle electrode implanted via laminectomy over a percutaneous electrode, implanted in exactly the same location in the same FBSS patients. All patients underwent percutaneous trial electrode placement and mapping to determine the optimal level for a midline 4-contact electrode array, and those with successful trials were randomized to receive a permanent electrode, which was either the same percutaneous design or an insulated paddle. The insulated paddle electrode showed significant technical advantages over the percutaneous electrode, notably (for purposes of the present discussion) in terms of the scaled amplitude necessary to cover the low back ( ). Clinical follow-up showed significantly better outcomes for the insulated paddle electrode at 2 years; however, this result was not maintained at 3 years, due in part to small sample size (24 at study inception) ( ). The patients in this study had leg pain equaling or exceeding LBP.
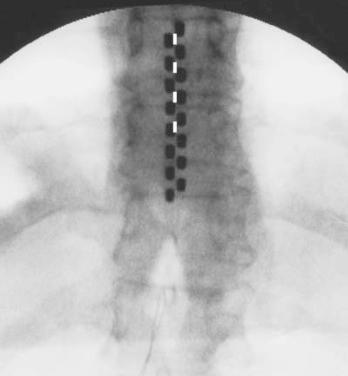
In a subsequent nonrandomized study in patients with a chief complaint of LBP (exceeding leg pain), we compared a single 4-contact percutaneous temporary electrode with a two-column 16-contact insulated paddle ( ). Fig. 50.3 shows the two configurations superimposed on a study subject’s anteroposterior thoracic spine X-ray. The percutaneous 4-contact afforded low back coverage in 23 of 25 patients screened (92%) and led to satisfactory relief in 64%. In the 10 patients for whom we collected comparative data for the temporary and the permanent electrode, there were no major technical advantages for either design in the acute comparison, indicating that the benefits of the insulated paddle were offset by the disadvantages of the two-column design shown in our prior studies. In the multicenter clinical trial of which this study was a part, 69% of patients reported fair to excellent relief of LBP at 1-year follow-up ( ).
These findings were consistent with finite element computer models of SCS, which had been developed to predict recruitment patterns—specifically, that an insulated paddle and a midline column of contacts (by comparison with two columns, one on either side of the midline) would minimize recruitment of lateral structures, in particular dorsal roots, and thus the segmental side effects that limit the useful range of stimulation amplitudes ( ; ).
It follows that a paddle electrode with a midline column—the optimal configuration among those studied earlier in this chapter—might offer even better performance if additional lateral columns were added to provide redundancy to compensate for migration or malposition. Going beyond this, computer models predicted that contacts in the lateral columns used as anodes would (1) shield lateral structures from recruitment and (2) allow “steering” from right to left if anodal current could be divided variably between the lateral contacts ( ).
Indeed, Holsheimer’s “transverse tripole” was shown to allow left-right steering in acute studies; however, in a series of 10 patients, “significant” LBP was “not particularly responsive” ( ). The paddle electrode available at the time had a single row of lateral contacts available for transverse stimulation, and neither implantation nor programming used the methodology described earlier to optimize its longitudinal placement or its performance. The same electrode was used in a subsequent multicenter trial, performed with more rigor using pain drawing templates (but not systematic, computerized adjustment), and paresthesia steering was demonstrated. Targeting the low back was not specifically undertaken at most study centers (although most patients had FBSS), and no particular advantages in this regard were observed ( ).
Continuing evolution of SCS systems has made more and more contacts (if not independent channels) available for use, and this has allowed not only more columns but also more rows of contacts. As shown in Fig. 50.4 , paddle electrodes with as many as 32 contacts are now available; thus, arrays may be created with 3, 4, 5, or more columns or centerlines as well as multiple rows ( ). Each row may allow lateral anodes, and this overcomes the limitation of the original transverse tripole, which was limited to a single row, the spinal level of which was fixed at the time of implantation. Each row allows noninvasive, postoperative programming to identify the midline, and as the number of columns or centerlines grows, the result approaches that of precise intraoperative placement using fewer columns. Not only paddles with three or more columns, but also percutaneous multicolumn arrays (in particular so-called “percutaneous tripoles,” first introduced by Law in , before implanted generators had enough contacts to support them fully), have been developed since the turn of the century ( ).

Programming a multicontact array to optimize its performance is a complex task: if all functional combinations of all contacts are to be tested, an array with 4 contacts requires 50 tests, which is beyond the capability of manual methods and requires computerized methods ( ). An 8-contact array has 6050 combinations; testing these exhaustively is beyond the capability of even a patient interactive system, requiring an algorithm to define a manageable subset for testing ( ). Such algorithms are under development, with growing reported success in achieving paresthesia coverage of the low back, using arrays with as many as 32 contacts, as shown in Fig. 50.4 ( ; ).
The importance of paresthesia coverage has come into question with the introduction of waveforms that do not produce paresthesia at amplitudes used therapeutically (to be distinguished from amplitudes used during electrode placement, so as to define position physiologically). Whereas “conventional” or “traditional” SCS uses pulse repetition rates (a.k.a. frequencies) at up to 1.5 kHz, adjusted to amplitudes that produce a vibratory or buzzing sensation, SCS at 10 kHz elicits no sensation until the amplitude is well above that used clinically. Thus, on the amplitude scale from perception to discomfort defined by and for conventional stimulation, 10 kHz is used at levels below perception.
It was reported first in a case series that pain relief, superior to that afforded by “conventional” SCS, could be achieved with 10 kHz SCS ( ). In 2015, an RCT demonstrated superiority in patients with a chief complaint of LBP ( ). A subset of the patients in this study, the great majority of whom had FBSS, had never undergone surgery. Relief of axial LBP by 10 kHz SCS has been reported in a case series of patients with no history of prior surgery ( ).
Paresthesia-free stimulation can be achieved with other waveforms: whereas conventional stimulation uses a monotonic waveform with invariant interpulse intervals, “burst” stimulation consists of short pulse trains at a high rate, repeated at a lower rate (emulating activity of single neurons). When 5 pulses at 500 Hz are repeated 40 times per second and delivered as SCS, pain relief is often achieved at amplitudes below the perceptual threshold ( ). In a small randomized, placebo-controlled trial comparing burst with conventional tonic and placebo SCS for limb and back pain, primarily in FBSS patients, many with a chief complaint of LBP, De Ridder reported significantly better results for burst, in particular for the LBP component ( ). A larger RCT comparing burst with conventional SCS in a mixed population, mostly FBSS, but without specific emphasis on predominance of LBP, has shown superiority of burst SCS ( ).
Paresthesia-free stimulation may be delivered with otherwise conventional SCS by simply adjusting amplitudes deliberately below perceptual threshold, at relatively high pulse widths and frequencies in the kilohertz range (“high density”). This stimulation strategy has been reported to afford superior results in some patients ( ). This case series evidence in patients failing conventional SCS has included patients with FBSS but has not specifically addressed those with a chief complaint of LBP.
It has been noted that high-frequency, burst, and high-density stimulation deliver higher power (energy per unit time) to the spinal cord than does conventional SCS, and improved results might represent a dose-response relationship ( ). Comparative efficacy studies have pitted one SCS waveform against another, as if they are mutually exclusive, when in fact they are complementary (assuming they can be delivered by the same device). One burst study, described earlier, for example, was done using a device which delivers both conventional and burst SCS, and crossover data were collected, showing that notwithstanding the superiority of burst stimulation, a substantial number of patients preferred conventional SCS ( ). A dual-purpose device makes both waveforms available with no more than a programming change. We might expect that devices capable of delivering multiple waveforms will offer significant advantages, but this remains to be established by further study.
The paresthesia generated by conventional SCS was used to guide electrode implantation in the burst studies, as well as in the high-density studies, before therapy (which was often paresthesia-free) began. Although the same might have been done in the 10 kHz studies, those studies relied upon radiographic guidance alone, using real time fluoroscopy to locate the midline, with a longitudinal target consistent with historical data from paresthesia mapping dating back to Law ( ), showing T9-10 as the optimal level for treatment of LBP. The potential role of real-time paresthesia mapping before 10 kHz stimulation remains to be determined—although this role is obvious if the same device will also deliver paresthesia-based therapy.
As shown in Fig. 50.5 , the electrode configuration reported for 10 kHz stimulation for LBP uses midline contacts placed percutaneously, so as to span approximately 2 vertebral levels above and below the T9-10 disc space. Placement is guided by fluoroscopy, but not by intraoperative test stimulation, as has been done traditionally for paresthesia-based stimulation. Following implantation, mapping in the ambulatory patient to select the best contact position(s) proceeds on the basis of reported pain relief. This can require many hours, even days, to assess each new contact position, whereas paresthesia mapping (whether by verbal or pain-drawing techniques) can take only seconds ( ). It remains to be seen whether the optimal contact position is in fact the same for both waveforms; for now, the recommended placement for 10 kHz stimulation for LBP is the same as that defined by paresthesia-based stimulation and reported during decades of experience.

The response to a trial using conventional stimulation determined whether a permanent implant would be done in the burst studies, as well as in the high-density studies. Had other waveforms been used as well during the trial, this might have improved the trial-to-implant yield, but this remains to be studied. The 10 kHz studies used 10 kHz stimulation for trials, and this might have led to higher implant rates than controls with conventional stimulation; but the implant rate might have been higher still had patients failing the trial had other waveforms available. This too remains to be studied.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here