Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Neuromodulation involves the use of both implantable and nonimplantable medical device technologies for treatment of disease through enhancement or suppression of the activity of the nervous system using electrical, pharmacologic, or other agents. Neuromodulation therapies may target the brain, spinal cord, peripheral nerves, and autonomic nervous system. Examples of neuromodulation therapies include spinal cord stimulation, deep brain stimulation, peripheral nerve stimulation, and surgically implanted drug delivery systems.
Use of electrical impulses for treatment of pain dates back to antiquity when use of torpedo fish to produce numbness was first described. The modern era involving use of electrical impulses for neuromodulation began with deep brain stimulation in the 1960s and was soon followed by application of spinal cord stimulation to the treatment of intractable pain. More recently, electrical stimulation of the central or peripheral nervous system has been applied to the treatment of patients with spinal cord injuries in an attempt to restore various types of functions.
Modern spinal cord stimulators (SCSs) are neuromodulatory devices that utilize epidural electrodes placed percutaneously, or through a limited open exposure, to deliver electrical impulses to the spinal cord. The epidural electrodes are connected by lead wires to an implanted, programmable pulse generator that can have an internal or external power source. Classically, this stimulation has been used to reduce neuropathic pain, or pain resulting from damage or abnormal activity within the nervous system. By acting on white-matter pathways in the dorsal column of the spinal cord, most modern SCS systems exchange debilitating neuropathic pain with paresthesias, which are considered more tolerable. SCS does not reliably relieve nociceptive pain, or pain from surgery or tissue damage. The location of the stimulation within the vertical axis of the spinal cord targets different areas of the body. Interestingly, SCS have been shown to have angiogenic effects, and have been used to treat diseases such as peripheral artery disease or angina pectoris. Spinal cord stimulation has been further studied for treatment of pain and paralysis resulting from spinal cord injury (SCI).
In the context of treatment of chronic pain, the mechanism of spinal cord stimulation is conceptualized based on the gate control theory of pain. This theory states that peripheral nerve fibers carrying pain to the spinal cord may have their input modified at the spinal cord level prior to transmission to the brain. The synapses in the dorsal horns act as gates that can either close to keep impulses from reaching the brain or open to allow impulses to pass. Small-diameter nerve fibers (C-fibers and lightly myelinated A-delta fibers) transmit pain impulses. Excess small fiber activity at the dorsal horn of the spinal cord opens the gate and permits impulse transmission, leading to pain perception. Large nerve fibers (A-beta fibers) carry nonpainful impulses, such as touch and vibratory sensation, and have the capacity to close the gate and inhibit pain transmission. Spinal cord stimulation is thought to preferentially stimulate large nerve fibers because these fibers are myelinated and have a lower depolarization threshold than small-diameter nerve fibers.
Experimental evidence suggests a mechanism of action for spinal cord stimulation by increasing levels of gamma aminobutyric acid (GABA) within the dorsal horn of the spinal cord. GABA is an inhibitor of neural transmission in the spinal cord and suppresses hyperexcitability of wide-dynamic range interneurons in the dorsal horn. Spinal cord stimulation may also exert a direct effect on brain activity, but this mechanism is not well understood.
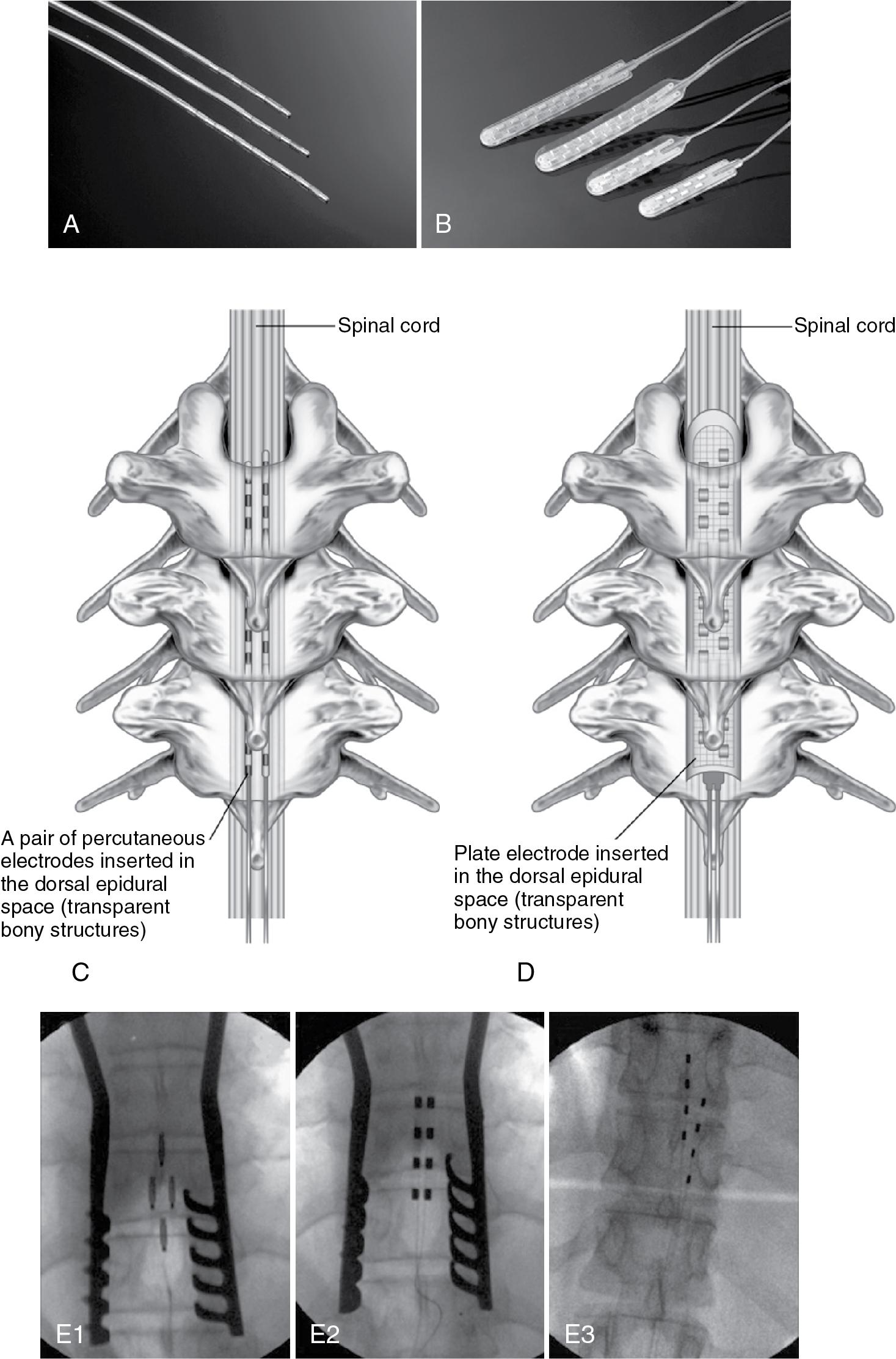
The two main types of electrodes are catheter-type electrodes and plate-type electrodes.
Catheter-type electrodes (also known as percutaneous electrodes) are placed via a percutaneous needle approach under fluoroscopic guidance and are ideal for use in trial stimulation to determine whether permanent implantation is appropriate.
Plate-type electrodes (also known as laminotomy, paddle, or surgical electrodes) require a surgical laminotomy for placement. Advantages of plate-type electrodes include lower risk of migration in the epidural space and increased electrical efficiency. Lead systems have evolved from quadripolar (four electrodes) or octapolar leads (eight electrodes) to current multilead systems ( Fig. 34.1 ).
General guidelines regarding initial lead placement are:
Pain involving the posterior occipital region : place leads near C2
Upper extremity pain not involving the hand : place leads between C2 and C5
Upper extremity pain involving the hand : place leads at C5 or C6
Chest wall pain and angina : place leads between T1 and T4
Pain involving the thigh and knee : place leads between T9 and T10
Pain involving the lower leg and ankle : place leads between T10 and T12
Pain involving the foot : place leads between T11 and L1
Successful coverage of the soles of the feet is challenging and may require stimulation of the L5 or S1 nerve roots. For axial back pain, one lead is placed at midline and another lead is placed on either side of midline. Final lead position is determined based on patient feedback and lead adjustment following initial lead placement.
The two main types of pulse generator systems are totally implantable pulse generators and radiofrequency-driven pulse generators.
Totally implantable pulse generators utilize an internal power source (lithium battery). Following activation, these pulse generators are controlled by transcutaneous telemetry and can be switched on-off with a magnet. The battery requires replacement in 2–5 years, while a rechargeable power source may last 10–25 years, or longer. At the end of this life span, the battery must be surgically changed. For this reason, studies have indicated that rechargeable battery systems may offer significant financial savings over long-term use.
Radiofrequency-driven pulse generators consist of a receiver implanted subcutaneously and a transmitter that is worn outside the body and utilizes an external power source. An antenna is applied to the skin and transmits the stimulation signals to the receiver. The radiofrequency-driven pulse generators have the ability to deliver more power than the totally implantable pulse generators and are appropriate for patients who have greater power requirements.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here