Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Most causes of sore throat are nonbacterial and neither require nor are alleviated by antibacterial therapy ( Tables 2.1, 2.2, and 2.3 ). Accurate diagnosis is essential. Acute streptococcal pharyngitis warrants proper diagnosis and prompt therapy to prevent serious suppurative and nonsuppurative sequelae. Life-threatening complications of oropharyngeal infections, whether caused by streptococci or other pathogens, may manifest initially with poorly differentiated symptoms of mouth pain and pharyngitis and then extend into the parapharyngeal space, cause jugular venous thrombophlebitis, or result in critical airway obstruction ( Tables 2.4 and 2.5 ). Noninfectious causes of sore throat, such as solid tumors, hematologic malignancy, or Kawasaki disease, if not appropriately diagnosed, may similarly carry a high risk of morbidity and even mortality. In most cases, history and physical examination identify the etiology of a sore throat or sufficiently narrow the differential diagnosis so as to direct an evaluation strategy or empiric treatment. It is important to note that in many of these diseases sore throat is not the defining symptom but part of a systemic illness (e.g., measles, COVID-19, Kawasaki disease).
| Infection |
|
| Irritation |
|
| Other |
|
| Definite Causes |
|
| Probable or Occasional Causes |
|
| Bacteria |
|
| Virus |
|
| Fungus |
|
| Peritonsillar Abscess | Retropharyngeal Abscess (Cellulitis) | Submandibular Space (Ludwig Angina) ∗ | Lateral Pharyngeal Space | Masticator Space ∗ | Epiglottitis | Laryngotracheobronchitis (Croup) | Bacterial Tracheitis | Postanginal Sepsis (Lemierre Syndrome) | |
|---|---|---|---|---|---|---|---|---|---|
| Etiology | Group A streptococci, oral anaerobes † | Staphylococcus aureus, oral anaerobes, † group A streptococci, “suppurative adenitis” | Oral anaerobes † | Oral anaerobes † | Oral anaerobes † | Haemophilus influenzae type b (rarely), group A streptococci, Streptococcus pneumoniae , Staphylococcus aureus , and non–type b H. influenzae | Parainfluenza virus; influenza, adenovirus, and respiratory syncytial virus less common | Moraxella catarrhalis, S. aureus, H. influenzae type b or nontypeable | Fusobacterium necrophorum |
| Age | Teens | Infancy, preteens, occasionally teens | Teens | Teens | Teens | 2–5 yr | 3 mo–3 yr | 3–10 yr | Teens |
| Manifestations | Initial episode of pharyngitis, followed by sudden worsening of unilateral odynophagia, trismus, hot potato (muffled) voice, drooling, displacement of uvula | Fever, dyspnea, stridor, dysphagia, drooling, stiff neck, pain, cervical adenopathy, swelling of posterior pharyngeal space Descending mediastinitis (rare) Lateral neck radiograph reveals swollen retropharyngeal prevertebral space: infants, >1× width of adjacent vertebral body (>2–7 mm); teens, >1/3× width of vertebral body (>1–7 mm) CT distinguishes cellulitis from abscess |
Fever, dysphagia, odynophagia, stiff neck, dyspnea; airway obstruction, swollen tongue and floor of mouth (tender) Muffled voice |
Severe pain, fever, trismus, dysphagia, edematous appearing, painful lateral facial (jaw) or neck swelling (induration) May lead to Lemierre syndrome |
Pain, prominent trismus, fever Swelling not always evident |
Sudden-onset high fever, “toxic” appearance; muffled voice; anxiety; pain, retractions; dysphagia; drooling; stridor; sitting-up, leaning-forward tripod position; cherry-red swollen epiglottis Usually not hoarse or coughing Lateral neck radiograph shows “thumb sign” of swollen epiglottis |
Low-grade fever, barking cough, hoarseness, aphonia, stridor; mild retractions; radiograph shows “steeple sign” of subglottic narrowing on anteroposterior neck view | Prior history of croup with sudden onset of respiratory distress, high fever, “toxic” appearance, hoarseness, stridor, barking cough, tripod sitting position; radiograph as per croup plus ragged tracheal air column | Prior pharyngitis with sudden-onset fever, chills, odynophagia, neck pain, septic thrombophlebitis of internal jugular vein with septic emboli (e.g., lungs, joints), bacteremia |
∗ Often odontogenic; check for tooth abscess, caries, tender teeth.
|
Most episodes of pharyngitis are caused by viruses (see Tables 2.2 and 2.3 ). It is difficult to precisely distinguish between viral and bacterial pharyngitis on clinical grounds, though certain clues may help. Accompanying findings of rhinitis, conjunctivitis, cough, croup, laryngitis, or discrete oropharyngeal ulcerations are common with viral infection but are rare in bacterial pharyngitis ( Table 2.6 ).
| Suggestive of Group A Streptococcus |
|
| Suggestive of Viral Etiology |
|
Many viruses can produce pharyngitis (see Tables 2.2 and 2.3 ). Some cause distinct clinical syndromes that are readily diagnosed without laboratory testing ( Table 2.7 ; see also Tables 2.1 and 2.4 ). In pharyngitis caused by parainfluenza viruses, influenza viruses, rhinoviruses, coronaviruses, and respiratory syncytial viruses, symptoms of coryza and cough often overshadow sore throat, which is generally mild. Parainfluenza viruses are associated with croup and bronchiolitis; minor sore throat and signs of pharyngitis are common at the outset but rapidly resolve. Influenza infection is often associated with high fever, cough, headache, malaise, myalgia, and cervical adenopathy in addition to pharyngitis. In young children, croup or bronchiolitis may develop. When influenza is suspected on clinical and epidemiologic grounds or confirmed by testing (polymerase chain reaction [PCR] is most accurate), specific antiviral therapy is available for treatment of patients and prophylaxis of family members and other close contacts. In young children, respiratory syncytial virus (RSV) infection is associated with bronchiolitis and, to a lesser degree, pneumonia and croup. In older children, RSV infection is usually indistinguishable from a simple upper respiratory tract infection. Pharyngitis is not a prominent finding of RSV infection in any age group. Infections caused by parainfluenza, influenza, and RSV are often seen in seasonal (winter) epidemics. Many viral pathogens can be identified using multiplex or targeted PCR testing, but there is rarely reason to test patients in the outpatient setting and infrequent benefit to testing in the inpatient setting, except to confirm and treat influenza.
| Gingivostomatitis | Herpangina | Hand-Foot-Mouth Disease | Chickenpox | Systemic Lupus Erythematosus (SLE) | Inflammatory Bowel Disease (IBD) | Aphthous Stomatitis | Behçet Disease | Vincent Stomatitis | Recurrent Scarifying Ulcerative Stomatitis (Sutton Disease) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Etiology | Herpes simplex virus (HSV I) | Coxsackievirus A, B; echovirus or HSV (rarely) | Coxsackievirus A, coxsackievirus B (rarely) | Varicella-zoster virus | Autoimmune | Autoimmune | Unknown | Unknown; vasculitis | Unknown; or anaerobic bacteria | Unknown |
| Location | Ulcerative vesicles of pharynx, tongue, and palate plus lesions of mucocutaneous (perioral) margin | Anterior fauces (tonsils), soft palate (uvula), less often pharynx | Tongue, buccal mucosa, palate, palms, soles, anterior oral cavity | Tongue, gingiva, buccal mucosa, marked cutaneous lesions; trunk > face | Oral, nasal mucosa; palate, pharynx, buccal mucosa | Lips, tongue, buccal mucosa, oropharynx | As in IBD | Oral (similar to IBD); genital ulcers | Gingiva; ulceration at base of teeth | Tongue; buccal mucosa |
| Age | <5 yr | 3–10 yr | 1 yr–teens | Any age | Any age | Any age | Teens and adulthood | Teens, adulthood, occasionally <10 yr | Teens; if younger, consider immunodeficiency and blood dyscrasia | Teens |
| Manifestations | Fever, mouth pain, toxic, fetid breath, drooling, anorexia, cervical lymphadenopathy; cracked, swollen hemorrhagic gums; secondary inoculation possible (fingers, eye, skin); reactivation with long latency (any age) | Fever, sore throat, odynophagia; summer outbreaks; 6–12 lesions (2–4 mm papule) → vesicle → ulceration; headache, myalgia | Painful bilateral vesicles, fever | Fever, pruritic cutaneous vesicles, painful oral lesions | Renal, central nervous system, arthritis, cutaneous, hematologic, other organ involvement; ulcers minimally to moderately painful; may be painless | Multiple recurrences; painful ulcerations 1–2 mm, but may be 5–15 mm; abdominal pain, diarrhea, hematochezia, weight loss | Similar to IBD | Painful ulcerations (heal without scarring); uveitis, arthralgia, arthritis, lower gastrointestinal ulceration (similar to IBD); recurrences; spontaneous remissions | Fever, bleeding gums; gray membrane | Deep, large, painful ulcerations; relapsing; scarring with distortion of mucosa |
Adenoviruses can cause upper and lower respiratory tract disease, ranging from ordinary colds to severe pneumonia and multisystem disease, including hepatitis, myocarditis, and myositis. The incubation period of adenovirus infection is 2–4 days. Upper respiratory tract infection typically produces fever, erythema of the pharynx, and follicular hyperplasia of the tonsils, together with exudate. Enlargement of the cervical lymph nodes occurs frequently. When conjunctivitis occurs in association with adenoviral pharyngitis, the resulting syndrome is called pharyngoconjunctival fever . Pharyngitis may last as long as 7 days and does not respond to antibacterials. There are many adenovirus serotypes; adenovirus infections may therefore develop in children more than once. Outbreaks have been associated with swimming pools and contamination in health care workers. If obtained, laboratory studies may reveal a leukocytosis and an elevated ESR.
The enteroviruses can cause sore throat. High fever is common, and the throat is mildly erythematous; tonsillar exudate and cervical adenopathy are unusual. Symptoms usually resolve within a few days. Enteroviruses historically were classified as nonpolio enteroviruses, coxsackie A viruses, coxsackie B viruses, and echoviruses, though with increasing recognition of the multitude of enterovirus serotypes they are now numbered consecutively as novel serotypes are identified. Enteroviruses can also cause meningitis, acute flaccid myelitis, myocarditis, rash, and two specific syndromes that involve the oropharynx: herpangina and hand-foot-mouth disease. Herpangina is characterized by distinctive discrete, painful, gray-white papulovesicular lesions distributed over the posterior oropharynx (see Table 2.7 ). The vesicles are 1–2 mm in diameter and are initially surrounded by a halo of erythema before they ulcerate ( Fig. 2.1 ). Fevers are typically present at illness onset, last several days before abating, and may reach 39.5°C or higher. The illness is typically caused by coxsackie A viruses and generally lasts <7 days, but severe pain may impair fluid intake and occasionally necessitates medical support. Hand-foot-mouth disease is also caused by enteroviruses, most commonly coxsackievirus A16. Painful vesicles that ulcerate can occur throughout the oropharynx, as opposed to the lesions of herpangina, which tend to be restricted to the posterior oropharynx. Vesicles also develop on the palms and soles and, less often, on the trunk, extremities, or diaper region ( Fig. 2.2 ). Fever is present in most cases, but many children do not appear seriously ill. Illness typically lasts <7 days.

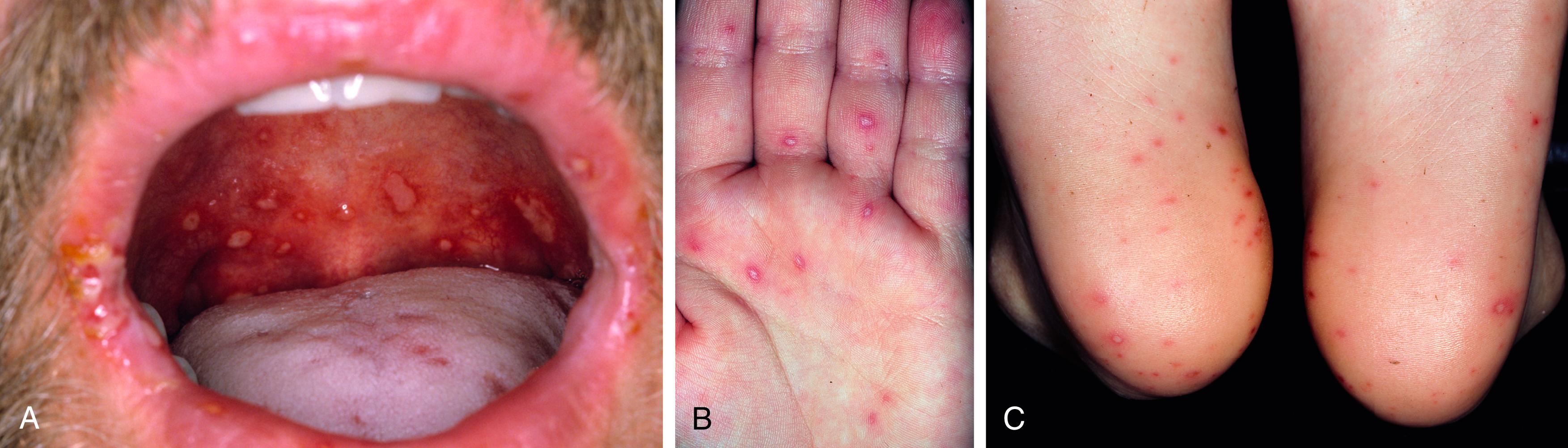
Primary infection caused by herpes simplex virus (HSV) ( Fig. 2.3 ) usually produces high fever with acute gingivostomatitis, involving vesicles throughout the anterior portion of the mouth, including the lips; vesicles eventually ulcerate. There is sparing of the posterior pharynx in herpes gingivostomatitis; the infection usually occurs in young children. High fever is common, pain is intense, and intake of oral fluids is often impaired, which may lead to dehydration and need for medical support. In adolescents, HSV may manifest as poorly differentiated pharyngitis. Approximately 35% of new-onset HSV-positive adolescent patients have herpetic lesions; most teenage patients with HSV pharyngitis cannot be distinguished from patients with other causes of pharyngitis. The classic syndrome of herpetic gingivostomatitis in infants and toddlers lasts up to 2 weeks; data on the course of more benign HSV pharyngitis infections in older children and adolescents are lacking. The differential diagnosis of vesicular-ulcerating oral lesions is noted in Tables 2.7 and 2.8 .

| Condition | Comment |
|---|---|
| Common | |
| Aphthous ulcers (canker sores) | Painful circumscribed lesions; recurrences |
| Traumatic ulcers | Accidents, chronic cheek biter, after dental local anesthesia |
| Hand-foot-mouth disease | Painful; lesions on tongue, anterior oral cavity, hands, and feet |
| Herpangina | Painful; lesions confined to soft palate and oropharynx |
| Herpetic gingivostomatitis | Vesicles on mucocutaneous borders; painful, febrile |
| Recurrent herpes labialis | Vesicles on lips; painful |
| Other viruses | HIV, varicella, EBV |
| Chemical burns | Alkali, acid, aspirin; painful |
| Heat burns | Hot food, electrical |
| Drugs | NSAIDs, chemotherapy, sulfa drugs, phenytoin, ACE inhibitors, others |
| Uncommon | |
| Neutrophil defects | Agranulocytosis, leukemia, cyclic neutropenia; painful |
| Systemic lupus erythematosus | Recurrent; may be painless or bullous |
| Behçet syndrome | Resembles aphthous lesions; associated with genital ulcers, uveitis |
| Necrotizing ulcerative gingivostomatitis | Vincent stomatitis; painful |
| Syphilis | Chancre or gumma; painless |
| Oral Crohn disease | Aphthous-like; painful |
| Histoplasmosis | Lingual |
| Pneumococcal sepsis or pneumonia | Gingival cystic ulcerations |
| Pemphigus | May be isolated to the oral cavity |
| Stevens-Johnson syndrome | May be isolated to or appear initially in the oral cavity |
| Mycoplasma (MIRM) | Rash may be absent |
| RIME | Non-mycoplasma infections; lesions similar to MIRM; may be reactive |
| PFAPA | Unknown etiology recurrent autoinflammatory fever syndrome |
| Celiac disease | Primary or nutritional deficiencies |
| Nutritional deficiencies | Vitamin B 12 , iron, folate |
Infants and toddlers with measles often have prominent oral findings early in the course of the disease. In addition to high fever, cough, coryza, and conjunctivitis, the pharynx may be intensely and diffusely erythematous, without tonsillar enlargement or exudate. Koplik spots , the pathognomonic white or blue-white enanthem of measles, appear on the buccal mucosa near the mandibular molars, generally before the typical measles rash develops. Complications of measles include ear infections, pneumonia, and encephalitis. In the United States, widespread measles vaccination virtually eliminated transmission of natural measles infection except among unvaccinated subpopulations (e.g., children younger than 12 months old, families who have refused immunization). Most recent cases are related to unimmunized visitors from countries with endemic measles, although there has been a rise in cases within the United States due to increasing rates of unvaccinated children.
The lesions of herpangina, hand-foot-mouth disease, herpes gingivostomatitis, and measles should be distinguished from noninfectious aphthous ulcers, colloquially referred to as canker sores. Aphthous ulcers are typically discrete, 3–5 mm in diameter, round or ovoid, with a peripheral erythematous halo and a white to yellow-white covering exudate. Lesions tend to be painful, though some may be noted only incidentally. An isolated episode of individual or clustered lesions may be related to physical or chemical irritation, a reaction to an allergic or infectious exposure, nutritional deficiency, or immune-mediated inflammation. Individuals with recurrent aphthous stomatitis may lack associated features during or between episodes and experience one to several outbreaks per year, a condition known as simple aphthosis. The outbreaks of simple aphthosis tend to start in late childhood or adolescence, last up to 2 weeks, and abate by adulthood. Patients with complex aphthosis tend to have more frequent outbreaks, have more numerous and painful lesions, and occasionally have lesions on the genital mucosa as well. In such circumstances, complex aphthosis must be distinguished from Behçet disease , the latter of which is a systemic inflammatory disorder that may include arthritis, neurologic manifestations, and cutaneous lesions, in addition to orogenital mucosal aphthae (see Table 2.6 ).
An autoinflammatory periodic fever syndrome known as PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis) occurs predictably every 2–8 weeks. The onset of PFAPA is usually before the age of 5 years. In addition to aphthous stomatitis and pharyngitis, PFAPA is characterized by high fever lasting 4–6 days. The diagnosis is clinical and is typically made in patients with a phenotype consistent with PFAPA after excluding cyclic neutropenia, other periodic fever syndromes, infections, malignancy, and the persistence of elevated acute-phase reactants between episodes. Individual episodes resolve spontaneously but may respond to oral prednisone. Cimetidine in PFAPA syndrome is ineffective. As corticosteroids do not prevent future fever cycles, long-term intervention may also include tonsillectomy with or without adenoidectomy, although risks of surgical intervention such as anesthetic and postoperative complications must be considered. In most patients PFAPA completely resolves without sequelae before puberty; a few persist into adulthood. Some patients initially diagnosed as having PFAPA actually had a monogenetic recurrent fever syndrome (see Chapter 54 ).
Acute exudative pharyngitis commonly occurs with infectious mononucleosis caused by primary infection with the Epstein-Barr virus (EBV). Mononucleosis is a febrile, systemic, self-limited lymphoproliferative disorder that is usually associated with hepatosplenomegaly and generalized lymphadenopathy. Acute pharyngitis may be mild or severe, with erythema, impressive tonsillar exudates, and significant tonsillar hypertrophy that can result in airway obstruction. Regional lymph nodes may be particularly enlarged and slightly tender. Infectious mononucleosis usually occurs in adolescents and young adults; EBV infection is generally milder or subclinical in preadolescent children. In U.S. high school and college students, attack rates are 200–800 per 100,000 per year. EBV is transmitted primarily by saliva.
After a 2–4-week incubation period, patients with infectious mononucleosis usually experience an abrupt onset of malaise, fatigue, fever, and headache, followed closely by pharyngitis. The tonsils are enlarged with exudates and cervical (often posterior) adenopathy. More generalized adenopathy with hepatosplenomegaly often follows. Fever and pharyngitis typically last 1–3 weeks, and lymphadenopathy and hepatosplenomegaly resolve over 3–6 weeks. Malaise and lethargy can persist for several months and can affect school or work performance.
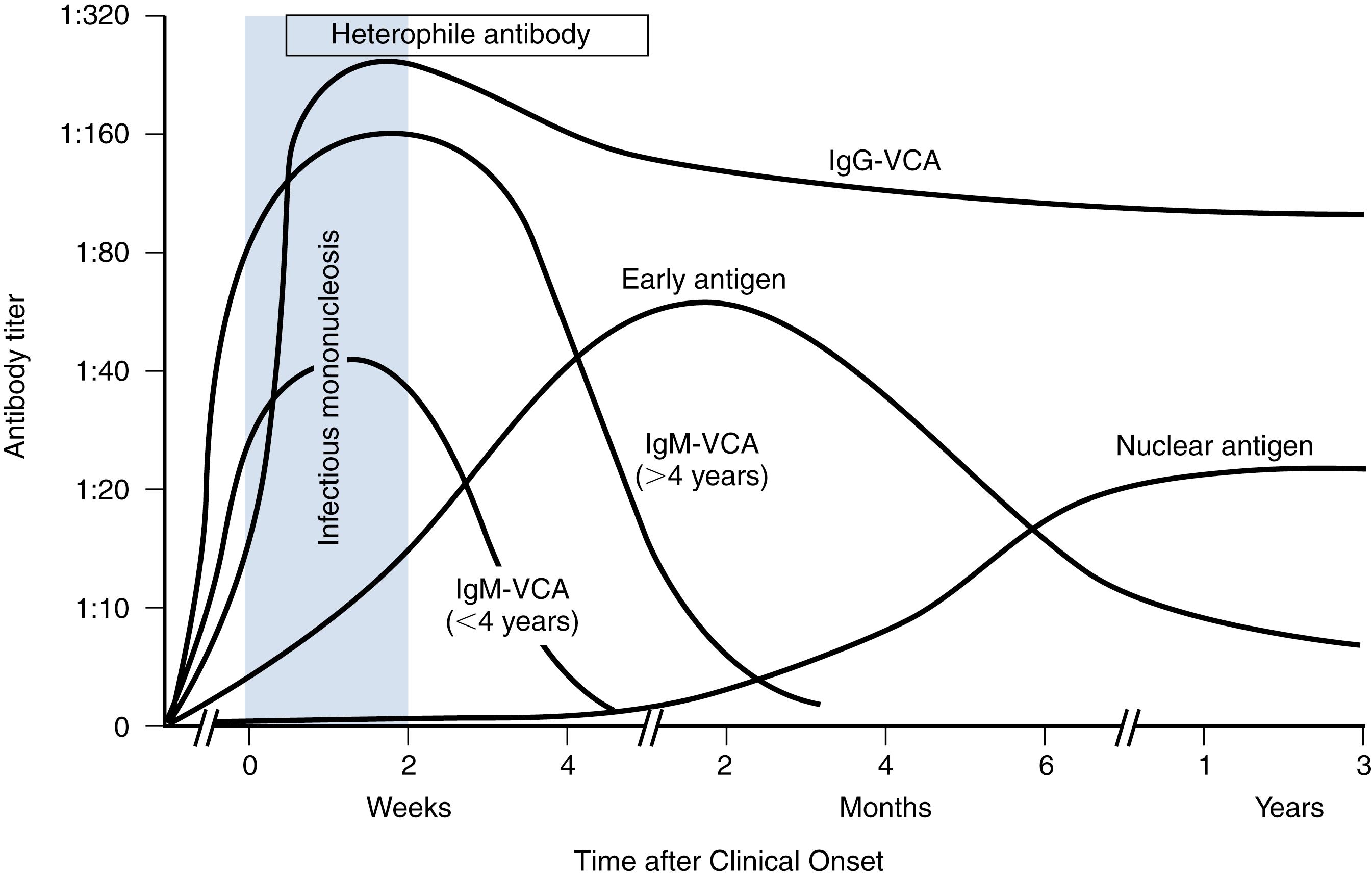
The findings of acute exudative pharyngitis together with hepatomegaly, splenomegaly, and generalized lymphadenopathy suggest infectious mononucleosis. Early in the disease and in cases without liver or spleen enlargement, differentiation from other causes of pharyngitis, including streptococcal pharyngitis, is difficult. Indeed, a small number of patients with infectious mononucleosis have a throat culture positive for group A streptococci, though these patients are likely streptococcal carriers. Patients with infectious mononucleosis treated for presumed streptococcal pharyngitis with antibacterials, particularly with ampicillin or amoxicillin, frequently develop a diffuse, erythematous, papular exanthem during the course of therapy that retrospectively suggests infectious mononucleosis due to EBV. An indistinguishable mononucleosis syndrome can occur with cytomegalovirus, but differentiation is rarely of clinical importance. Acute toxoplasmosis may also present similarly. Serologic evidence of mononucleosis should be sought when splenomegaly or other features are present or if symptoms persist longer than expected. Laboratory studies of diagnostic value include atypical lymphocytosis; these lymphocytes are primarily EBV-specific, cytotoxic T lymphocytes that represent a reactive response to EBV-infected B lymphocytes. A modest elevation of serum aminotransferase levels, reflecting EBV hepatitis, is common. Tests useful for diagnosis include detection of heterophile antibodies that react with bovine erythrocytes (most often detected by the monospot test) and a specific antibody against EBV viral capsid antigen (VCA), early antigen (EA), and nuclear antigen (EBNA). Acute infectious mononucleosis is usually associated with a positive heterophile antibody test result and the presence of antibodies to VCA and EA in a specific pattern; subacute and remote infections produce distinct antibody profiles ( Fig. 2.4 ). In young children, the monospot may be negative.
Primary infection with HIV may produce a mononucleosis-like illness with sore throat, fever, lymphadenopathy, rash, myalgia, and hepatosplenomegaly. Early infection may be detected by viral RNA or DNA load because immunoglobulin M (IgM) or immunoglobulin G (IgG) titers may have not yet developed.
In evaluating a patient with sore throat, the primary concern is usually accurate diagnosis and treatment of pharyngitis caused by group A streptococci (GAS), also known as Streptococcus pyogenes , which accounts for up to 30% of all episodes of pharyngitis in children in the United States. The sequelae of GAS pharyngitis, especially acute rheumatic fever (ARF) and poststreptococcal glomerulonephritis (PSGN), at one time resulted in considerable morbidity and mortality in the United States and continue to do so in other parts of the world. Prevention of ARF in particular depends on timely diagnosis of streptococcal pharyngitis and prompt antibacterial treatment. Group A streptococci are characterized by the presence of group A carbohydrate in the cell wall, and they are further distinguished by several cell wall protein antigens (M, R, T). These protein antigens, especially the M protein, a virulence factor, are useful for studies of epidemiology and pathogenesis but are not used in clinical care.
Group A streptococcal pharyngitis is endemic in the United States; epidemics occur sporadically. Episodes peak in the late winter and early spring. Rates of GAS pharyngitis are highest among children aged 5–11 years old. Spread of GAS in classrooms and among family members is common, especially in the presence of crowded living conditions. Transmission occurs primarily by the inhalation of organisms in large droplets or by direct contact with respiratory secretions. Pets do not appear to be a frequent reservoir. Untreated streptococcal pharyngitis is particularly contagious early in the acute illness and for the first 2 weeks after the organism has been acquired. Antibacterial therapy effectively prevents disease transmission: Within 24 hours of institution of therapy with penicillin, it is difficult to isolate GAS from patients with acute streptococcal pharyngitis, and infected children can return to school.
Molecular epidemiology studies of streptococcal pharyngitis have shown that the prevalent M protein types vary among communities and over time. Numerous distinct strains of GAS can circulate simultaneously in a community during the peak season. Molecular genetic studies can establish the specific M protein gene (i.e., emm gene); M protein identification is not available or useful for clinical care. Children with streptococcal pharyngitis can serve as a local reservoir for strains that cause invasive disease (e.g., sepsis, streptococcal toxic shock syndrome, cellulitis, necrotizing fasciitis) in the same geographic area and season.
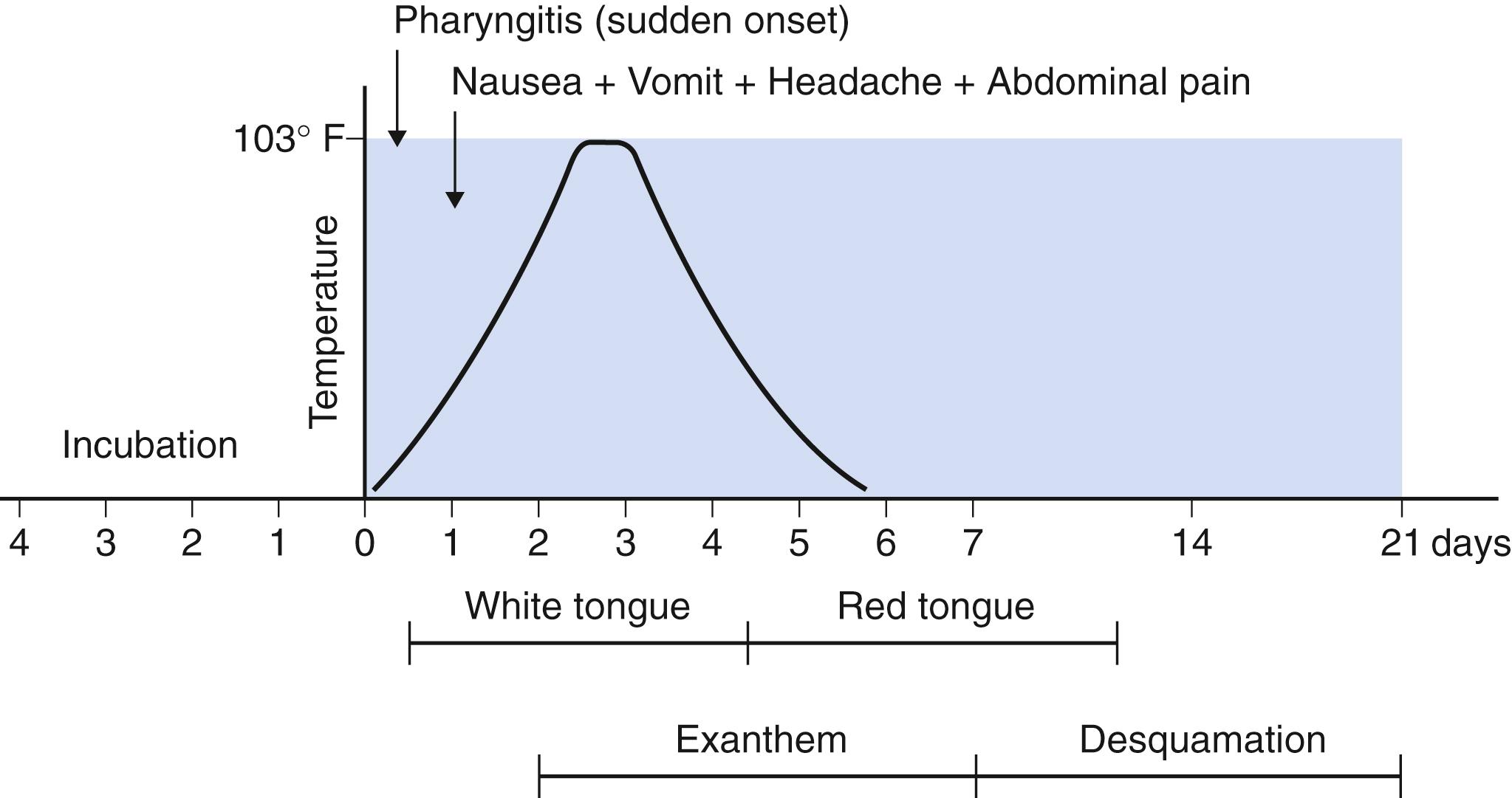
Acute streptococcal pharyngitis classically presents with the sudden onset of fever and sore throat (see Table 2.6 ). Headache, malaise, abdominal pain, nausea, and vomiting occur frequently. Cough, rhinorrhea, conjunctivitis, stridor, diarrhea, discrete ulcerated lesions, and hoarseness are distinctly unusual and suggest a viral etiology (see Table 2.6 ).
Physical examination reveals marked pharyngeal erythema. Petechiae may be noted on the palate but can also occur in viral pharyngitis, especially mononucleosis. Tonsils are enlarged, symmetric, and bright red, with patchy exudates on their surfaces. Anterior cervical lymph nodes are often tender and enlarged.
Combinations of these signs can be used to assist in diagnosis; in particular, tonsillar exudates in association with fever, palatal petechiae, and tender anterior cervical lymphadenopathy strongly suggest infection with GAS. However, other diseases can produce this constellation of findings, including infectious mononucleosis. Some or all of these classic characteristics may be absent in patients with streptococcal pharyngitis. Symptoms usually resolve within 5 days even in the absence of antibacterial therapy. Younger children can have a syndrome called streptococcosis —coryza with crusting below the nares, more generalized adenopathy, and a more chronic course. When rash accompanies the illness, accurate clinical diagnosis is easier. Scarlet fever , so-called because of the characteristic fine, diffuse red rash, is essentially pathognomonic for infection with group A streptococci. Scarlet fever is rarely seen in children younger than 3 years old or in adults.
The rash of scarlet fever is caused by infection with a strain of GAS that contains a bacteriophage encoding for production of an erythrogenic (redness-producing) toxin, usually erythrogenic (also called pyrogenic) exotoxin A (designated SPE A). Scarlet fever is simply GAS pharyngitis with a rash and should be explained as such to patients and their families. Although patients with streptococcal toxic shock syndrome are also infected with GAS that produces SPE A, most GAS pharyngeal infections are not associated with development of severe invasive or systemic disease.
The rash of scarlet fever has a texture like sandpaper and blanches with pressure ( Figs. 2.5 and 2.6 ). It usually begins on the face, but after 24 hours, it becomes generalized. The face is red, especially over the cheeks, and the area around the mouth often appears pale in comparison, giving the appearance of circumoral pallor. Accentuation of erythema occurs in flexor skin creases, especially in the antecubital fossae, a finding termed Pastia lines. The papillae of the tongue may be red and swollen, hence the designation “strawberry tongue.” The erythema begins to fade within a few days. Desquamation begins within a week of onset on the face and progresses downward, often resembling that seen after mild sunburn. On occasion, sheetlike desquamation occurs around the free margins of the fingernails; this is usually coarser than the desquamation seen with Kawasaki disease. The differential diagnosis of scarlet fever includes Kawasaki disease, measles, and staphylococcal toxic shock syndrome ( Table 2.9 ).

| Scarlet Fever | Kawasaki Disease | Measles | Staphylococcal Toxic Shock Syndrome | Staphylococcal Scalded Skin Syndrome | |
|---|---|---|---|---|---|
| Agent | Group A streptococci | Unknown | Measles virus | Staphylococcus aureus | S. aureus |
| Age range | All (peak, 5–15 yr) | Usually <5 yr | <2 yr, 10–20 yr | All (especially >10 yr) | Usually <5 yr |
| Prodrome | No | No | Fever, coryza, cough, conjunctivitis | Usually no | No |
| Enanthem | No | Occasionally | Koplik spots | No | Limited |
| Mouth | Strawberry tongue, exudative pharyngitis, palatal petechiae | Erythema; red, cracked lips; strawberry tongue | Diffusely red, no cracked lips | Usually normal | Erythema |
| Rash | Fine, red, “sandpaper,” membranous desquamation, circumoral pallor, Pastia lines | Variable polymorphic; erythematous face, trunk, and diaper area; tips of fingers and toes desquamate 10–28 days after onset |
Maculopapular; progressing from forehead to feet; may desquamate | Diffuse erythroderma; desquamates | Erythema, painful bullous lesions; positive Nikolsky sign; desquamates |
| Other | Cervical adenitis, gallbladder hydrops, fever | Coronary artery disease; fever >5 days; conjunctival (nonpurulent) injection; tender, swollen hands and feet; cervical adenopathy (size >1.5 cm); thrombocytosis;pyuria (sterile); gallbladder hydrops | “Toxic” appearance; dehydration; encephalitis, pneumonia; | Shock (hypotension, including orthostatic); encephalopathy; diarrhea; headache | Fever, cracked lips; conjunctivitis |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here