Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
© 2018 Elsevier Inc. All rights reserved. Please note that the copyright for the original figures submitted by the contributors is owned by Contributors.
Control of local disease is the critical determinant of the ultimate treatment outcome in most cases of chordomas and chondrosarcomas. Surgical resection, with the aim of complete tumor removal, is considered the mainstay treatment modality. Surgery can provide definitive pathologic diagnosis, alleviate mass effect, preserve or restore neurologic function by decompressing critical neurovascular structures, and optimize tumor geometry and spatial relationships with the surrounding structures for the postoperative radiation therapy that is commonly recommended. Nonetheless, the successful management of skull base chordomas and chondrosarcomas is challenging. The vast majority of these neoplasms originate from the clivus or the spheno-petro-occipital synchondrosis. Consequently, by virtue of their deep, central location and inherent anatomical relations with multiple cranial nerves and the internal carotid artery (ICA), complete tumor removal is often precluded.
This chapter will review important considerations in the management of patients harboring skull base chordomas and chondrosarcomas with an emphasis on surgical treatment. The general principles of skull base surgery and the concepts, foundations, and anatomic bases of modern multicorridor, 360-degree access to the skull base will be presented. The 360-degree access to the skull base involves multidisciplinary cooperation in surgical strategies designed to decrease operative morbidity by minimizing manipulation of neurovascular tissue. A comprehensive description of both open transcranial and endoscopic endonasal approaches (EEAs) to the skull base will be presented as an introduction to the following chapters of this book; these should assist the reader in selecting the most appropriate surgical approach and treatment strategy for individual patients.
Treatment options for skull base chordomas and chondrosarcomas include surgical resection and radiation therapy. Clinical and radiographic observation may be appropriate only for asymptomatic, highly reliable patients with a small and well-circumscribed lesion in the petrous apex whose radiological findings suggest a low-grade chondrosarcoma (see Chapter 7 ) given the indolent nature of this tumor and the likelihood of detecting significant growth on surveillance scans [magnetic resonance (MR) images].
The vast majority of chordomas and chondrosarcomas, however, will be symptomatic at the time of diagnosis, and treatment is indicated. A multidisciplinary team of neurosurgeons, otolaryngologists, head and neck surgeons, and radiation oncologists must develop a comprehensive plan to maximize tumor control and patient survival and limit the risk of treatment-related complications. Treatment strategies include biopsy followed by observation, biopsy followed by radiation therapy, surgical resection followed by observation, and surgical resection followed by radiation therapy. The choice of the strategy should be based on many factors including the patient’s overall condition and neurological status, the tumor’s size, location, extension and relationship with critical neurovascular structures, the goals of surgery, prior treatment (i.e., surgery and radiation therapy), the presence of metastases, and the experience of the surgical team with open transcranial approach and EEAs to the skull base.
As discussed in Chapter 2 , chordomas and chondrosarcomas are distinct pathological entities with different natural histories. Maximum tumor resection, with preservation of neurological function, followed by adjuvant radiotherapy, is the gold standard treatment for chordomas. The Chordoma Global Consensus Group recommends, whenever possible, an en bloc resection with negative microscopic margins of 1 mm or greater to minimize the risk of tumor seeding and recurrence along the surgical pathway. However, this goal is rarely achieved for clival chordoma because of the involvement of neurovascular structures, especially the abducens nerve and the ICA. In these situations, a more reasonable option is aggressive piecemeal gross total resection. Inseparable tumor attachment to the cranial nerves or critical arteries necessitates incomplete resection (leaving tumor-positive margins along involved nerve roots and/or arteries) to preserve neurological function. Postoperative radiation therapy is then indicated.
In contrast, treatment of skull base chondrosarcomas is more controversial because their natural history is less well understood. On the one hand, there is little evidence that greater extent of resection correlates with improved survival when postoperative radiation is given. On the other hand, experienced surgeons have reported favorable patient outcomes and high rates of recurrence-free survival (above 70%) for totally resected tumors. Given the controversy, the potential benefits of each treatment modality must be balanced against the associated morbidity.
Unless surgical resection is planned regardless of the pathology, given the vast number of neoplastic and nonneoplastic lesions that can mimic chordoma and chondrosarcoma (see Chapter 6 ), osteolytic skull base tumors arising from or involving the clivus and the spheno-petro-occipital synchondrosis should be biopsied prior to definitive treatment. In planning a biopsy, the risk of seeding along the biopsy track and the possibility of resecting the track during subsequent tumor removal must be considered. Moreover, a biopsy may be contraindicated by a high risk of neurovascular complications.
As discussed in Chapter 5 , preoperative biopsy of skull base tumors is most commonly performed through the nose, mouth, and mastoid. Chordomas are more prone to extend extracranially and are more likely to be biopsied than chondrosarcomas. Chordomas extending from the clivus into the soft tissue of the nasal and oral pharynx may form a submucosal mass apparent during physical examination and, therefore, easily biopsied using a transnasal/transoral endoscope. It is also important to be aware of extensive skull base erosion and intradural extension that increase the risks of inadvertent injury to the intracranial neurovascular structures and cerebrospinal fluid (CSF) leakage. In performing a biopsy of a tumor extending into the oropharynx and parapharyngeal space, the surgeon must be aware of the position of the parapharyngeal segment of the ICA, which may have a tortuous trajectory, especially in elderly patients, and thus be vulnerable to injury risking catastrophic vascular complications. Chondrosarcomas, unless quite large, are more difficult to biopsy because they less commonly extend extracranially. Occasionally, these tumors may erode into the mastoid process, where a biopsy can be performed easily. A transnasal biopsy may be performed in tumors extending medially, ventrally, and superiorly from the petrooccipital synchondrosis into the lateral recess of the sphenoid sinus.
Once the diagnosis of chordoma or chondrosarcoma is established, surgical resection is usually indicated, although asymptomatic patients with small low-grade chondrosarcomas may be closely observed. Surgically accessible tumors, especially those whose radiation to curative dose is precluded by the proximity to the brainstem or optic pathways, are targeted for removal, whereas relatively inaccessible tumors, such as those investing the cavernous sinuses, are left for postoperative radiation therapy. A comprehensive bimodality plan may be prospectively designed for large tumors spanning multiple skull base compartments.
Experience with radiation, be it fractionated photons, fractionated protons, stereotactic radiosurgery and, most recently, heavy ion particles, as the sole treatment of skull base chordomas and chondrosarcomas is limited (see Chapter 30, Chapter 32, Chapter 33, Chapter 35, Chapter 35 ). The excellent results with adjuvant radiation therapy for low-grade chondrosarcomas suggest that it may be sufficient for some small, asymptomatic, low-grade tumors. Preliminary results of stereotactic radiosurgery of such lesions are also impressive. Almost all higher grade chondrosarcomas and chordomas warrant surgery whenever extensive resection is feasible. For these pathologies, radiation alone is reasonable only for surgically inaccessible tumors or in patients having contraindications, by virtue of age or medical condition, to the extensive surgery often required for radical removal.
The fundamental principle of skull base surgery is to achieve adequate exposure for maximal tumor resection while reducing the risks of complications, such as neurological loss and infection, minimizing brain retraction, preserving uninvolved anatomic structures, and properly reconstructing the skull base defect created during the approach and tumor resection. However, achieving these goals is often challenging. For decades, the skull base, especially the clival region, was labeled as “no-man’s-land” due to its deep location, complex anatomy, and intricate relationship with facial and neck structures such as the upper aerodigestive tract, the basal surface of the brain, multiple cranial nerves, and vessels that form the polygon of Willis.
From a historical perspective, larger craniotomies and extensive craniofacial disassembly were initially favored because they provide wide access for the visualization of tumor margins and maneuvering of instruments required safe tumor dissection, while obviating brain retraction. The introduction of the operating microscope, which significantly improved intraoperative illumination and visualization, and microsurgical instrumentation, better understanding of the complex skull base microsurgical anatomy, and increased collaboration among neurosurgeons, otolaryngologists, head and neck surgeons, and those from other disciplines, made safe and effective tumor resection through smaller exposures feasible.
Over the past 20 years, the development of the “keyhole” and “surgical corridor” concepts, the use of the surgical endoscope, popularization of EEAs to the skull base, and other technological advancements (e.g., surgical navigation, intraoperative monitoring, highly crafted and powered instruments) have allowed less invasive approaches and safer, more extensive tumor resections.
Tumor exposure and resection must be followed by proper skull base reconstruction that restores isolation of the sterile intracranial space from contaminated extracranial spaces. This begins with watertight dural closure and/or reconstruction to prevent postoperative CSF leakage and infection. Often opened dura cannot be primarily resewn. Vascularized tissue, such as regional nasal mucosal flaps rotated on a vascular pedicle or free tissue flaps reanastamosed to local blood supply are needed, especially when postoperative radiation therapy is planned. Dissecting along natural tissue planes to minimize disruption of normal tissue and closing the wound in anatomic layers reduce postoperative discomfort and improve functional and cosmetic results.
Preoperative assessment should always include general medical, neurologic, otolaryngological, and radiographic evaluation. Endocrinological evaluation may be necessary in selected cases. Even though aggressive gross total resection of skull base chordomas and chondrosarcomas is oncologically desirable, the decision to operate must be undertaken only after careful consideration of the surgical goals in the context of the risks of perioperative complications and the complementary benefits of the adjuvant radiation therapy that is commonly recommended.
General medical evaluation:
A patient’s mental and physical vigor as well as overall medical condition, including comorbidities, must be evaluated to determine fitness for substantial and aggressive surgery and possibly lengthy recovery.
Neurological evaluation:
Evidence of cranial neuropathies and brainstem compression must be sought. A complete neuro-ophthalmologic evaluation is recommended for patients with visual symptoms and tumors encroaching on the visual pathways and the cavernous sinuses.
Otolaryngological evaluation:
Hearing deficits mandate formal audiological evaluation. Tumors compromising the lower cranial nerves along the posterior cranial fossa or extending anteriorly may compromise, respectively, swallowing and speech and respiration and must undergo formal laryngological evaluation to estimate the need for postoperative tracheostomy and gastrostomy.
Endocrinological evaluation:
Lesions involving the pituitary region warrant studies to exclude pituitary hypersecretion or insufficiency. Postoperative endocrinologic follow-up is also warranted in these cases, especially after adjuvant radiation therapy that exposes the pituitary gland or hypothalamus.
Radiographic evaluation:
High-quality neurodiagnostic imaging is essential for effective preoperative assessment and planning (see Chapter 7 ). The tumor size, location, pattern of extension, and relationship to critical neurovascular structures, revealed by multiplanar computed tomography (CT) and MR imaging, will determine the potential for complete surgical resection. Furthermore, appropriate design of complementary surgical approaches (i.e., combined or staged approaches) and radiation fields necessitates clear delineation of the tumor extent and normal structures. CT imaging, windowed for bone detail, best depicts the pattern of tumor calcification and extent of bone destruction. Skull base erosion around the orbit, paranasal sinuses, cavernous sinuses, carotid canal, and occipital condyle are important preoperative considerations as it may increase the risks of intraorbital complications, occult CSF leakage, inadvertent cranial nerve or ICA injury, and craniovertebral junction instability.
MR imaging helps characterize the soft tissue component of the tumor and involvement of adjacent structures. The tumor’s intracranial and extracranial extension may be delineated and differentiated from the surrounding bone marrow and soft tissue by of fat-suppressed T2-weighted and contrast-enhanced T1-weighted imaging techniques, respectively. Clival erosion may be also assessed by unenhanced T1 images. Displacement or encasement of the neurovascular structures in the subarachnoid space, best seen in steady-state acquisition sequences (i.e., FIESTA or CISS), may affect the choice of surgical approach.
Formal vascular assessment with MR angiography and, even less commonly, formal cerebral angiography, is seldom required. However, given the higher risk of inadvertent vascular injury, a temporary balloon test occlusion (BTO) combined with perfusion scanning may be indicated in cases with tumor encasement of the ICA. This test estimates the risk of permanent neurological deficits following permanent occlusion of the ICA. Choices for patients who fail BTO include a more conservative resection and high-flow bypass cerebral revascularization permitting ICA sacrifice and more aggressive tumor resection (see Chapter 22 ). Another option to minimize the risk of vascular injury is preoperative stenting to strengthen the wall of an artery involved by tumor. In these cases, surgery is postponed for 3 months to allow new intimal growth to line the stent.
CT angiography with a bone window setting is routinely used especially in recurrent tumors, for surgical strategy planning and intraoperative navigation. For instance, this reveals the direction of chondrosarcoma displacement of the ICA and guides the choice of approach: lateral displacement favors an anterior approach and medial displacement favors a lateral approach.
The choice of surgical approach to chordomas and chondrosarcomas requires a thorough understanding of the anatomy of the central skull base from which they most commonly arise (see Chapter 9 ). The central skull base encompasses the frontal air sinuses anteriorly, the nasion, the sinonasal cavities between the orbits, the foramen cecum, crista galli, cribriform plates, planum sphenoidale, tuberculum sellae, sella, and the clivus from posterior clinoid processes down through the foramen magnum. The roof of the ethmoid sinus begins in the midline just behind the foramen cecum. It contains the crista galli in the midline and cribriform plates bilaterally. The anterior and posterior ethmoidal arteries and olfactory nerves pass through foramina in the cribriform plates. The roof of the sphenoid sinus, the planum sphenoidale, begins just behind the cribriform plate and extends to the tuberculum sellae. Lateral to the cribriform plate and planum sphenoidale, the orbital processes of the frontal bone, the plana orbitale, form the orbital roofs. These converge posteromedially to the optic canals and the anterior clinoid processes. The anterior clinoid processes, extending laterally as the superior aspect of the lesser wing of the sphenoid bone, define the posterior margin of the anterior cranial fossa. The greater wing of the sphenoid bone forms part of the posterolateral wall of the orbit and contains the foramen rotundum and foramen ovale. Extending inferiorly from the greater sphenoid wing between the foramen rotundum and the foramen ovale are the pterygoid plates.
Chordomas have a strong predilection for the clival midline. The clivus is the defining osseous component of the central cranial base. It extends from dorsum sellae to the foramen magnum (see Chapter 2 ). It can be divided into three parts:
The superior third , from the dorsum sellae and posterior clinoid processes to the petrous apices, is sphenoidal in origin: anteriorly lie the sella and sphenoid sinus; laterally, the intracavernous ICA, cavernous sinus, tentorial notch, and temporal lobe; and posteriorly, the bifurcation of the basilar artery, its branches, and the midbrain.
The middle third , between the petrous apex at Dorello canal and the pars nervosa of the jugular foramen, is the superior extension of the basi occiput; anteriorly lie the nasopharynx and retropharyngeal tissue; laterally, the inferior petrosal sinus, the anterior petrous face, and cranial nerves VII and VIII; and posteriorly, the trunk of the basilar artery and its branches, the vertebrobasilar junction, and the pons.
The lower third , between the pars nervosa of the jugular foramen (JF) to the foramen magnum, includes the occipital condyles and hypoglossal canal of the basi occiput; anteriorly lie the nasopharynx and retropharyngeal tissues; laterally, the sigmoid sinus, jugular tubercle and bulb, and hypoglossal nerve; and posteriorly, the vertebral artery, pontomedullary junction, medulla, and cervicomedullary junction.
Conversely, chondrosarcomas typically originate from the paramedian central skull base along the spheno-petro-occipital synchondrosis and tend to extend medially into the clivus and laterally into the adjacent petrous bone early in their growth. These tumors may also extend from there in multiple directions: superomedially toward the cavernous sinus and sellar–suprasellar region and further medially, to the sphenoid sinus; laterally toward the Meckel cave and middle cranial fossa (MCF); inferolaterally toward the jugular foramen; posteriorly toward the cerebellopontine angle and cerebellomedullary cisterns in addition to the brainstem; and anteriorly, displacing or encasing the petrous, lacerum, and paraclival segments of the ICA. The petrous temporal bone is the defining osseous component of the lateral cranial base. It has an apex, a base, and three surfaces. Its apex reaches the posterior margin of the greater wing of the sphenoid bone at the junction of the upper and middle thirds of the clivus. Its base ends in the mastoid portion of the temporal bone. The petrous apex forms the posterior wall of the foramen lacerum and is bordered laterally by the distal carotid canal. Its superomedial margin is lined by the tentorial attachment and grooved by the superior petrosal sinus, and its inferior margin is grooved by the inferior petrosal sinus along the lateral aspect of the middle third of the clivus.
The anterosuperior surface of the petrous bone forms the posterior third of the floor of the MCF. The medial portion of this surface contains the trigeminal impression anteriorly, the roof of the internal auditory meatus and cochlea centrally, and the arcuate eminence covering the superior semicircular canal posteriorly. The lateral portion of this surface along the junction with the squamosal temporal bone forms the roofs of the petrous portion of the ICA anteriorly and the vestibule and proximal facial canal posteriorly. The central portion of the anterosuperior face of the petrous bone is formed by the tegmen tympani above the tympanic cavity, mastoid antrum, and tensor tympani muscle. Impressions for the greater and lesser superficial petrosal nerves lie along its anterolateral aspect.
The posteromedial surface of the petrous temporal bone forms the lateral wall of the posterior fossa. Its anterior portion extends from the apex to the internal auditory meatus above and the anterosuperior corner of the JF below. Its posterior portion begins at the posterior wall of the internal auditory meatus, contains the vestibular aqueduct, forms the medial portion of the base at the sigmoid sinus, and abuts the mastoid part of the temporal bone.
The inferior surface of the petrous bone is bordered by the foramen lacerum anteromedially and the foramen ovale and foramen spinosum anterolaterally. Its central portion contains attachments for the eustachian tube medially and is pierced by the proximal carotid canal laterally. Posteriorly this surface contains the jugular fossa medially and is attached to the tympanic portion of the temporal bone medially. The tympanic part of the temporal bone lies at the junction of squamous, petrous, and mastoid parts of the temporal bone. The mandibular fossa lies anteriorly, the squamosal temporal bone and external canal lies superiorly, and the jugular fossa lies medially. Its posterior portion gives rise to the styloid process separated from the mastoid process by the stylomastoid foramen that transmits the facial nerve.
The goal of an operation within the overall treatment plan, whether it is en bloc excision with margins devoid of microscopic tumor, gross total resection of the imaging abnormality, or radical subtotal removal to improve the geometry for postoperative radiation therapy, should be foremost in the surgeon’s mind at all times. Within the context of the goal chosen, a “skull base team” of neurosurgeons, otolaryngologists, and head and neck surgeons with skills and expertise in open and endoscopic procedures and oncologic and vascular surgery should coordinate the surgical strategy.
The most direct and least destructive surgical route that will allow the most complete resection with fewest complications is the preferred one. Overall, the site of origin or attachment of the tumor in the skull base and its direction of expansion will dictate the displacement of the surrounding cranial nerves and blood vessels and determine the most appropriate surgical approach. However, in selecting the optimal route of exposure, it is important to consider the effects of surgery on the normal tissues that will require surgical manipulation. Any operative displacement of tissue has the potential to permanently alter the anatomy and physiology of the affected structures. Moreover, a combination of different approaches should be considered for larger tumors with no specific predilection for the direction of growth to achieve these goals (see Chapter 21 ).
Sound knowledge of the three-dimensional skull base anatomy is essential for the thoughtful design and meticulous implementation of this surgical strategy seeking to balance the extent of tumor resection and the risk of postoperative morbidity.
The skull base has two surfaces: (1) the endocranial surface, which faces the brain, contains many anatomic landmarks to guide open transcranial approaches, such as the subfrontal and extended MCF approaches and (2) the exocranial surface, which faces the sinonasal cavities, orbits, pharynx and parapharyngeal spaces, pterygopalatine and infratemporal fossae, and infrapetrosal spaces, has numerous anatomic landmarks to guide the transfacial approach and EEAs. These include canals, foramina, and fissures, which connect both surfaces and give passage to neural and vascular structures.
From a geometric perspective, the epicenter of the skull base may be represented as a region of confluence of critical neurovascular structures (i.e., cranial nerves, the ICA, and the polygon of Willis) surrounded by the central skull base foramina. As the cranial nerves travel outward toward the foramina, their pathways diverge radially such that they create potential surgical corridors to anatomically distinct modules of the skull base separated by key neurovascular anatomical planes. These corridors are arrayed circumferentially for 360 degrees around the skull base and should be developed in both open transcranial approaches and EEAs used either independently or in combination. This concept of surgical corridors to anatomically distinct modules of the skull base emphasizes the simplicity of approach and respect for the integrity of premorbid anatomy as facilitators of tumor exposure and resection with minimal brain retraction, limited manipulation of neural tissue, and control of vascular structures.
The most important consideration in selecting a specific corridor for approaching a skull base tumor is avoidance of crossing the axial plane of a cranial nerve. These nerves are exquisitely sensitive to manipulation and are best kept to the perimeter of a route of tumor access and resection where they are less likely to be disturbed.
Nerves within a corridor that must be moved back and forth during tumor removal are highly vulnerable to iatrogenic injuries, especially when the tumor is firm or tightly attached to the surrounding structures. Direct dissection along nerves and vessels should be avoided if their plane with tumor is indistinct given the risk of direct trauma or ischemic injury to the nerves and of bleeding or stroke from vessel disruption. For larger tumors involving multiple anatomic modules and necessitating use of multiple surgical corridors, a staged, rather than a more extensive single operation, may be considered (see Chapter 21 ).
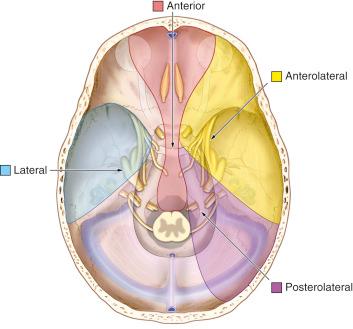
Surgical approaches to chordomas and chondrosarcomas of the central skull base can be grouped in this anatomically modular multicorridor scheme with regard to the primary angle of approach: anterior midline, anterolateral, lateral, and posterolateral surgical modules. Given that the skull base falls off from superior to inferior as one moves from the foramen cecum to the foramen magnum, the area of skull base exposed by these various approaches also moves from anterosuperior to posteroinferior. Thus the two most posteriorly situated corridors, the lateral and posterolateral modules, may be further divided into lateral–inferior and inferior–posterolateral approaches, respectively. The anatomical limits of each of these corridors are described as follows:
Anterior midline corridor
The anterior midline corridor is bordered laterally by the optic nerves, cranial nerves III, IV, V1 and VI, and the cavernous segment of the ICA in its superior aspect; by cranial nerve VI and the paraclival segment of the ICA in its middle aspect; and by cranial nerve XII posterolaterally and vertebral arteries in its inferior aspect.
Anterolateral corridor
The anterolateral corridor is bordered anteromedially by the lateral limits of the superior aspect of the anterior midline corridor and the supraclinoidal segment of the ICA and posterolaterally by the cochlea, semicircular canals, and VII–VIII cranial nerve complex. An inferior extension of this corridor toward the posterior cranial fossa is limited posteromedially by the bifurcation of the basilar artery, the posterior communicating artery, and cranial nerve III.
Lateral and lateral–inferior corridors
The lateral corridor is bordered anteriorly, similarly to the anterolateral corridor, by the lateral limits of the superior aspect of the anterior midline corridor and the petrous segment of the ICA rather than its supraclinoidal segment. The posterior limit is defined by the position of the cochlea, semicircular canals, and VII–VIII cranial nerve complex. Compared with the anterolateral corridor, the lateral corridor has a more lateral to medial trajectory. An inferior extension toward the posterior cranial fossa may be achieved by drilling the anterior portion of the petrous bone (i.e., anterior petrosectomy). The lateral–inferior corridor corresponds to a subtemporal–infratemporal approach and provides a shallow exposure of the MCF and midclivus through a zygomatic osteotomy and resection or displacement of the mandibular condyle.
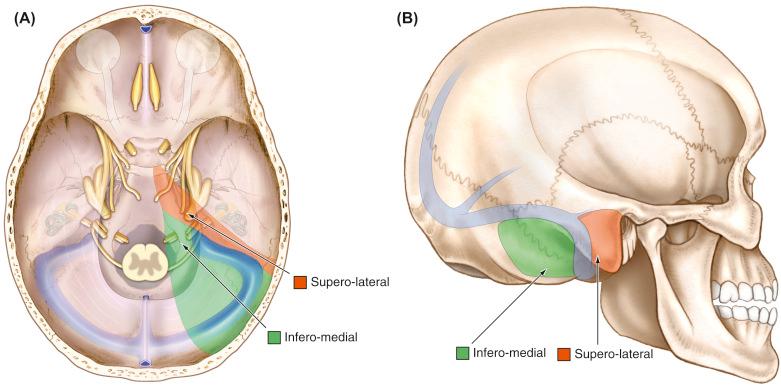
Posterolateral and inferior–posterolateral corridor
The posterolateral corridor is limited anterolaterally by the posterior limits of the lateral corridor and posteromedially by the lateral limits of the inferior aspect of the anterior corridor (i.e., cranial nerve XII and vertebral artery). This corridor is further divided into superolateral (i.e., posterior transpetrosal) and inferomedial (i.e., extreme lateral approaches) components by the sigmoid sinus, jugular bulb, and lower cranial nerves (IX–XI).
Each direction of approach, the bones traversed, and the limiting structures encountered are listed in Table 10.1 . Figs. 10.1 and 10.2 illustrate the 360-degree surgical corridors to the central skull base. An extensive discussion of the indications, advantages, limitations, preoperative planning, surgical technique, complication avoidance, and postoperative care relevant to each anatomic module and surgical corridor, from anterior midline to posterolateral, is presented in the Surgery of Skull Base Tumors section of this book.
| Approach | Clivus Targeted | Bones Traversed | Limiting Structures |
|---|---|---|---|
| Anterior Midline | |||
| Subfrontal | All | Frontal, nasal, ethmoid, sphenoid, occipital | Orbits, optic nerves, cranial nerves III–VI, cavernous/paraclival/petrous ICA, cranial nerve XII, vertebral arteries |
| Transfacial | All | Nasal, maxillary, ethmoid, sphenoid, occipital | Orbits, optic nerves, cranial nerves III–VI, cavernous/paraclival/petrous ICA, cranial nerve XII, vertebral arteries |
| Endoscopic endonasal | All | Sphenoid, ethmoid, occipital, petrous | Optic nerves, cranial nerves III–VI, cavernous/paraclival/petrous ICA, cranial nerve XII, vertebral arteries |
| Anterolateral | |||
| Pterional | Superior one-third (lateral) | Frontal, squamous, sphenoid (LW, GW) | Cavernous/supraclinoidal ICA, cranial nerves III–VI, SOF, BA, PCA, PComA |
| Lateral | |||
| Extended middle cranial fossa | Superior half (lateral) | Sphenoid (LW, GW, squamous, anterior petrous | Cavernous/petrous ICA, cranial nerves III–VI, SOF, cochlea, SCC, cranial nerves VII–VIII |
| ST-IT | Middle one-third (lateral) | Zygoma, mandible, squamous, anterior petrous | Petrous ICA, V3, cochlea, SCC, cranial nerves VII–VIII |
| Posterolateral | |||
| Posterior transpetrosal | Middle half (lateral) | Petrous, occipital, squamous | Cochlea, SCC, VII–VIII, sigmoid sinus, jugular bulb, IX–XI |
| Extreme lateral | Inferior one-third (lateral) | Occipital, C1-C2 | Vertebral artery, cranial nerves VI–XII, sigmoid sinus, jugular bulb, cranial nerves IX–XI |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here