Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Curth’s postulates provide a group of criteria that are helpful to determine whether a skin condition is likely to be related to an internal malignancy.
Individual paraneoplastic skin conditions tend to be associated more frequently with certain types of cancer (e.g., Bazex syndrome and upper aerodigestive cancer).
The pathogenesis of many paraneoplastic skin conditions remains unclear. Tumor-secreting hormones, paracrine factors, and the immune response may contribute to variable cutaneous findings.
Cancer-related genodermatoses, such as hereditary leiomyomatosis and its association with renal cell cancer, may present with skin findings before the internal malignancy. Therefore, early diagnosis can prompt screening to detect occult malignancy.
A family history of cancer and a personal or family history of cancer of the same type, particularly of earlier onset of malignancy than expected, should prompt consideration of an inherited cancer syndrome.
The skin often reflects internal processes, and patients’ awareness of this leads them to consider malignancy as a potential cause for many cutaneous abnormalities. Indeed, there are many skin conditions that have been linked to internal malignancy in a specific and/or nonspecific manner. This chapter considers those cutaneous disorders that have been linked to internal malignancy, the precise manner in which the cutaneous disease and the neoplasm are related, and the evaluation necessary for the patient with a cutaneous sign of internal malignancy.
Curth previously suggested criteria by which to gauge the potential relationship of two disorders, in this case a cutaneous finding and neoplasia ( Table 17-1 ). The disorders may occur concurrently or follow a parallel course; there may be a specific tumor site or cell type associated with the cutaneous disease; there may be a statistical association between the two processes; or there may be a genetic association between the two disorders. In this chapter, we examine these factors to determine whether a “true” association exists for three categories of skin disease: (1) proliferative and inflammatory dermatoses; (2) hormone-secreting tumors; and (3) inherited syndromes.
| Concurrent onset |
| Parallel course |
| Uniform neoplasm (site or cell type) |
| Statistical association |
| Genetic association |
The characteristic clinical feature of acanthosis nigricans (AN) is hyperpigmented, velvety thickening of the skin on intertriginous surfaces. The eruption usually affects the axillary vault ( Fig. 17-1 ), neck, inguinal crease, nipples, and umbilicus, but may also involve areas of trauma, such as the elbows, knees, and knuckles. Frequently, the oral mucosa has a papillomatous thickening. In rare instances, the eruption can become generalized ( Fig. 17-2 ). Verrucous or papillary lesions may accompany the typical lesions of AN. Patients may develop multiple seborrheic keratoses simultaneously.

AN can occur in many clinical scenarios, including obesity and insulin resistance, and as a manifestation of a number of heritable diseases (e.g., Crouzon syndrome, congenital lipodystrophy). Once other associations have been excluded, the possibility of an underlying neoplasm must be considered, particularly with widespread AN skin involvement. In general, patients with “malignant AN” are older adults with a history of associated weight loss.
AN most often occurs simultaneously with the underlying malignancy; however, it may precede or follow a malignancy diagnosis. Approximately 90% of the tumors associated with AN arise within the abdominal cavity, particularly the gastrointestinal and genitourinary tracts. Gastric adenocarcinoma is the most commonly described cancer associated with malignant AN. However, malignancies outside the abdomen and nonadenocarcinomas have been reported. The course of malignant AN parallels the course of the tumor, which tends to be aggressive in nature. Malignant AN is a prototypic dermatological condition associated with malignancy, fulfilling all of Curth’s “postulates” except for having a genetic association.
Acrokeratosis paraneoplastica, or Bazex syndrome, is by definition always associated with an underlying malignancy. Acrokeratosis paraneoplastica develops progressively through three stages. The initial cutaneous signs consist of erythematous to violaceous, poorly defined macules with a fine adherent scale that occur over the acral areas of the body, including the fingers, toes, ears, and nose. A paronychial reaction is also common. In the second stage, skin lesions begin to generalize and keratoderma develops. In the third stage, the eruption generalizes but still maintains its violaceous nature and predilection for acral involvement ( Fig. 17-3 ). The three stages of the cutaneous disease parallel the growth and spread of the underlying tumor. Bazex syndrome is more common in men, and the underlying tumors are most often squamous cell carcinomas of the upper aerodigestive tract; however, a variety of other solid malignancies and lymphomas have also been associated. Therefore, a comprehensive head, neck, and pelvic examination with laboratory, radiographic, and endoscopic evaluation is needed. As with acanthosis nigricans, the course of cutaneous involvement in Bazex syndrome typically parallels the course of the tumor, thereby fulfilling the criteria to consider it a marker of internal malignancy.

Several bullous dermatoses have been reported to be associated with malignancy. Although the association between bullous pemphigoid and cancer may be related primarily to the increased incidence of both conditions in elderly patients, certain other autoimmune bullous dermatoses with dermal epidermal junction pathology appear to be associated with an increased risk of malignancy, in particular those with negative immunofluorescence results, those with prominent mucosal lesions, and those with linear IgA disease. Egan and colleagues reported solid organ malignancies in 10 of 35 patients with antiepiligrin cicatricial pemphigoid (AECP). In eight cases the cancer was discovered within 14 months of the diagnosis of AECP. AECP is an uncommon, severe, and often scarring mucosal variant of pemphigoid associated with an IgG antibody directed against laminin 5. In contrast, two reviews of mucous membrane pemphigoid associated with antibodies to the β4α6 integrin subunits did not identify an increased risk of cancer. Furthermore, although a wide variety of neoplasms have been associated with bullous pemphigoid, there does not appear to be a specific course relating the pemphigoid to the malignancy. Thus, at present the data do not support a relationship between bullous pemphigoid and malignancy, with the possible exception of certain pemphigoid subsets, particularly AECP.
Epidermolysis bullosa acquisita (EBA) has very rarely been associated with malignancy, most commonly of hematologic origin. However, several such reports describe patients with features of both EBA and cicatricial pemphigoid.
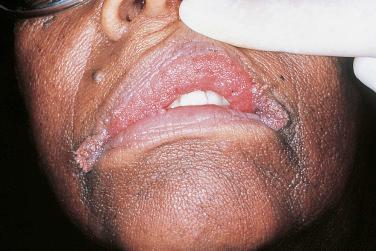
The pemphigus group of disorders is most commonly associated with thymoma and lymphoproliferative malignancies. Patients with thymomas also often develop myasthenia gravis. The pemphigus course does not coincide with that of the neoplasm. However, careful review of chest X-ray findings may be prudent to ensure a possible thymoma is not missed. In the early 1990s, Anhalt and coworkers reported an entity that they termed “paraneoplastic pemphigus” (PNP). Patients with PNP develop severe mucosal erosions and ulcerations, polymorphic cutaneous lesions that may resemble erythema multiforme, and antibodies targeting a number of proteins, particularly desmoplakin, envoplakin, and periplakin ( Fig. 17-4 ). However, several cases of lichenoid paraneoplastic pemphigus in patients treated with rituximab have been reported in which autoantibody detection was delayed or antibodies were not identified. The term paraneoplastic autoimmune multiorgan syndrome (PAMS) has been proposed in order to reflect the multiorgan system involvement now appreciated with PNP. Patients often also develop disease involving their bronchi and may die of respiratory failure (see Chapter 16 for further discussion of PNP/PAMS). The prognosis is poor, with very few survivors.

Dermatitis herpetiformis (DH) is associated with a risk of non-Hodgkin’s lymphoma (NHL), particularly enteropathy-associated T-cell lymphoma and B-cell NHL. In a recent meta-analysis, one in 2000 persons with gluten-sensitive enteropathy develops NHL each year. In DH patients who develop intestinal lymphoma, the removal of the tumor does not appear to affect the course of the cutaneous disease.
Porphyria cutanea tarda (PCT) has been associated with hepatic tumors, in particular with primary hepatoma. This association is most likely a coincidental phenomenon, as hepatitis C virus infection is a risk factor for both PCT and hepatic carcinoma. The exact frequency of hepatic tumors in patients with PCT is not known; however, there are reports of concurrent onset and a parallel disease course. Careful evaluation of the liver, including hepatitis C antibody testing, is advised in all patients with PCT.
As discussed in Chapter 2 , dermatomyositis (DM) is clearly associated with malignancy, which affects approximately one-quarter of patients with adult-onset DM; however, only rarely do patients with DM have a concurrent onset and a parallel course of their tumors. The malignancy work-up of an adult with a new diagnosis of DM is reviewed in detail in Chapter 2 , but goes beyond traditional age-appropriate evaluation. Women should be carefully evaluated for malignancy of the breast and gynecologic system. Ethnicity should also be considered: nasopharyngeal carcinoma was the most common malignancy in a study of DM in Taiwan. All patients should have a chest X-ray and probably a CT scan of the chest, abdomen, and pelvis, as well as a stool hematest. Malignancy risk appears to decrease with time from DM diagnosis, but repeat examinations should be performed annually for at least the first 3 years of the disease course, as malignancies such as ovarian cancer may not be easily detected by physical examination and imaging. At all times, unexplained symptoms or signs should be thoroughly evaluated.
Malignancies appear to be a coincidental occurrence in patients with lupus erythematosus. Several reports of lymphoreticular malignancies in patients with systemic lupus erythematosus likely reflect a complication of immunosuppressive therapy. Myeloma and paraproteinemias have been reported in patients with chronic cutaneous lupus erythematosus, but the frequency and significance of these findings are not clear.
An increased risk of malignancy in patients with scleroderma has been confirmed in two recent meta-analyses. Increased risk of lung cancer, NHL, and other hematopoietic cancers was found. One study suggested that men are at higher risk of developing cancer than women, possibly due to the greater number of men who use tobacco. Although breast cancer is frequently reported in women with scleroderma, the risk of breast cancer in scleroderma was found to be equivalent to that of the general population.
The coexistence of cutaneous small-vessel vasculitis and malignant neoplasms has been noted and reported as paraneoplastic vasculitis. Cutaneous small-vessel vasculitis is a common finding, as are cutaneous and systemic polyarteritis nodosa. Most of the tumors reported with vasculitis are of the lymphoreticular system (particularly hairy cell leukemia), but sporadic cases associated with solid tumors have also been described. Occasionally, the cutaneous disease is the initial finding in these patients, and a parallel course may also occur. A patient presenting with cutaneous vasculitis probably does not require a specific evaluation for malignancy.
Reports linking the sudden appearance of angiomas or telangiectases with internal malignancies have been published in the dermatological literature. Angiomatous lesions are common in the adult population and are seen as small, cherry-colored papules. It is not clear whether a rapid onset of lesions should prompt a malignancy evaluation. The situation in regard to telangiectases is similarly unclear.
The sudden appearance or growth of multiple seborrheic keratoses is known as the sign of Leser–Trélat (see Fig. 17-1 ). Numerous reports have linked this condition to various malignancies. Many patients also have AN, and the sign of Leser–Trélat is similarly associated with intra-abdominal adenocarcinoma, albeit to a lesser extent than with malignant AN. Population studies have not demonstrated a link between multiple seborrheic keratoses and internal malignancy. However, a patient has been described who had demonstrable epidermal growth factor receptors on the seborrheic keratosis, with evidence that a melanoma produced this factor. In this patient, when the melanoma was excised, the keratoses regressed. Although all the criteria for an association with malignancy are not fulfilled, it seems reasonable to carefully evaluate patients with a sudden onset or growth of multiple seborrheic keratoses, including evaluation for other epidermal features associated with internal malignancy, such as AN and tripe palms. The work-up should include a history and physical examination, and imaging studies of the gastrointestinal and genitourinary systems.
Erythroderma (exfoliative dermatitis) is a cutaneous reaction characterized by general erythema, edema, and scaling (see Chapter 14 ). The reaction may be accompanied by fever, lymphadenopathy, organomegaly, and/or leukocytosis. Malignancy may be present in approximately 10% to 15% of patients. In most instances, the malignancy is in the lymphoreticular system, but several reports of solid tumors have also been published. The course of the cutaneous disease often follows that of the tumor, and the discovery of the malignant process has often been linked to the diagnosis of the cutaneous disorder. Therefore, the possibility of an underlying neoplasm must be considered in all patients with erythroderma of unknown etiology.
There are multiple figurate erythemas, but the only one that appears to be truly related to malignancy is erythema gyratum repens. In this eruption, erythematous lesions form gyrate or serpiginous bands that rapidly spread across the cutaneous surface ( Fig. 17-5 ), producing a “wood-grain” appearance. Nearly all patients with erythema gyratum repens have an associated malignancy, which is often discovered concurrently. The course also frequently parallels that of the neoplasm. Although any malignancy may be associated, lung cancer is the most common, followed by breast, genitourinary (GU), and gastrointestinal (GI) tumors. The presence of erythema gyratum repens mandates an extensive internal evaluation for malignancy.

Hypertrichosis is the excessive growth of hair without signs of virilization ( Fig. 17-6 ). The sudden development of fine downy hair has been linked to the presence of an underlying neoplasm in all patients thus far reported. The malignancies are of varied sites and cell types, and are often discovered at the time of the diagnosis of hypertrichosis lanuginosa. Glossitis has also accompanied the malignancy-associated down, but it is believed to be a manifestation of vitamin deficiency rather than a related finding. Patients with this type of hair growth who do not have another clear explanation for their condition, such as a medication (e.g., cyclosporine, minoxidil), porphyria cutanea tarda, or endocrinopathy, should be evaluated for the possibility of an internal malignancy.

Acquired ichthyosis resembles ichthyosis vulgaris, and is characterized by rhomboidal scales with margins that are lifted off the surface of the skin. Acquired ichthyosis is most frequently associated with lymphoreticular disorders, particularly Hodgkin’s lymphoma. It is also associated with other paraneoplastic conditions, such as AN and the sign of Leser–Trélat. However, several other nonmalignant conditions have been associated with acquired ichthyosis, including hypothyroidism and sarcoidosis. When acquired ichthyosis is related to a malignancy, the cancer diagnosis precedes the diagnosis of acquired ichthyosis in most cases.
Keratoacanthoma is a rapidly growing epidermal neoplasm that may be locally invasive but otherwise exhibits a benign course. In association with sebaceous neoplasms, keratoacanthomas are one of the cardinal features of Muir–Torre syndrome, a variant of hereditary nonpolyposis colorectal cancer (HNPCC) Lynch syndrome II. Additional sporadic cases describing an association between multiple keratoacanthomas and internal malignancy have been described. However, because patients with keratoacanthoma tend to be elderly, this association may be an age-related phenomenon.
Although superficial thrombophlebitis is a relatively common medical condition, migratory thrombophlebitis (Trousseau’s syndrome) is associated with a risk of an underlying occult malignancy, most frequently of the pancreas, stomach, or lung. The veins of the chest, abdomen, and lower extremities are involved either sequentially or simultaneously. The hypercoagulable state associated with cancer is probably multifactorial in origin, and may be induced by inflammatory cytokines, acute-phase reactants, circulating tissue factor, and cancer microparticles. Patients with migratory thrombophlebitis without a known underlying cause should have a thorough evaluation, including a CT scan of the chest and abdomen.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here