Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
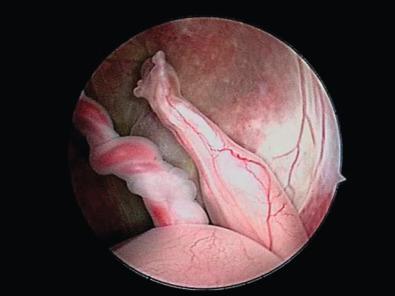
Sirenomelia is a rare congenital disorder that was previously considered a severe form of caudal regression, although it is currently considered a completely different entity. Also known as the mermaid syndrome , it is characterized by a variable degree of atrophy of the lower limbs, with the resultant appearance of a mermaid tail or fin ( Fig. 144.1 ). Because of the associated anomalies (particularly bilateral renal agenesis), the syndrome is typically considered lethal; however, several case reports now exist of survival to several years of life.
Sirenomelia is characterized by three common findings: a single lower limb, bilateral renal agenesis, and a single umbilical artery contiguous with the aorta. Multiple other severe anomalies may present. Reported associated findings include ambiguous or absent external genitalia, absent internal genitalia, absent bladder, absence of the anus and rectum, and sacral agenesis.
Two methods of classifying sirenomelia have been proposed. The first categorizes cases into three groups based on the number of feet present: symelia apus, symelia unipus, and symelia dipus. Symelia apus is the most common and is characterized by a single lower extremity and absent or rudimentary feet. Symelia unipus shows a single foot with two femurs, tibiae, and fibulae. With symelia dipus both feet are present but are malrotated, thus resembling fins.
The second classification system is based on the presence or absence of bones in the lower limb. Type I sirenomelia has all the bones of the limb present (two femurs, two tibiae, two fibulae). Type II has two femurs and two tibiae but fused fibulae, and in type III the fibulae are completely absent. Types IV and V are both characterized by partially fused femurs and are distinguished by the presence of fused fibulae in type IV and absent fibulae in type V. In type VI, a fused femur and fused tibia are present, and type VII has a fused femur and no tibia.
A key feature to distinguish sirenomelia from caudal regression syndrome is the anatomy of the umbilical artery. In sirenomelia, a large artery arises from the aorta and functions as a single umbilical artery ( Fig. 144.2 ). This artery is likely a remnant of the vitelline artery complex and is almost always associated with sirenomelia. In contrast, cases of caudal regression may be distinguished by the presence of two umbilical arteries, nonlethal renal anomalies, and two hypoplastic lower limbs.

Sirenomelia is a rare disorder, occurring in 1.5 : 100,000–4.2 : 100,000 births. It is 100–150 times more common in monozygotic twins than singletons. The sirenomelia spectrum of defects includes external and internal genital defects. Because of the absence of external genital and infrequent information on gonadal or chromosomal sex, data on sex distribution are very scarce; however, the limited information that is available indicates male sex preference or does not indicate any substantial sex preference.
Sirenomelia is also strongly associated with maternal pregestational diabetes; 2% of reported cases are in diabetic mothers. A recent epidemiologic study by Orioli et al. observed a higher prevalence (2.36 : 100,000) of sirenomelia in the Mexican registry (one of 19 birth defect surveillance systems analyzed worldwide) with an increased prevalence with maternal age less than 20 years. Considering twinning and maternal diabetes are both associated with sirenomelia, and both conditions are more common in older gravidae, the higher prevalence of sirenomelia found in younger mothers in this study was unexpected.
Although this has been described as “fused lower limbs,” it more likely represents failure of blastogenesis of the lower limb buds. Two theories exist as to the etiology. The first is the vascular steal theory developed by Stevenson et al. This theory posits that blood flow is diverted from the embryo, caudal to the origin of the aberrant vitelline remnant. As a result, tissues distal to this site are either malformed or not formed because of lack of oxygen and nutrients. As the vitelline remnant normally arises superior to the inferior mesenteric and renal arteries, the affected tissues typically include the kidneys, lower intestine, sacrum, and lower extremities. For this theory to be accurate, the vascular steal must occur before day 23 of development, which is before the cleavage of the lower limb bud.
More attention is now being focused on an alternative theory; the concept of primary development field defects. During blastogenesis, the caudal eminence gives rise to the lower limb buds as well as the perineum, somites, and vertebrae. An insult at the caudal neuropore could give rise to the spectrum of anomalies seen in sirenomelia.
Mutations in the superfamily of CYP genes have been noted in animal models (mice) with sirenomelia. Specifically, CYP26A1 is the receptor of retinoic acid, and lower vertebral column malformations have been reported in pregnancies after exposure to high doses of retinoic acid at different gestational ages, linking sirenomelia and retinoic acid intoxication. Another observation is the link between bone morphogenic protein 7 (BMP7) and twisted gastrulation (Tsg); loss of BMP7 combined with a complete loss or half-dose of Tsg in mice models is associated with sirenomelia. These studies have not been replicated in humans.
Sirenomelia is considered to be a sporadic event. Affected fetuses typically have a normal karyotype, and the recurrence risk is not thought to be greater than that of the general population. No instances of familial recurrence of sirenomelia have been reported; however, under the pathogenetic concept of sirenomelia as part of caudal regression syndrome, familial cases are known. Teratogenic exposures may play a role. Animal models demonstrate associations between sirenomelia and exposure to retinoic acid, cadmium, lithium, diethylpropion, lead, hyperthermia, and radiation. In addition, there are case reports of sirenomelia after cocaine use.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here