Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Age-specific rates of many sexually transmitted infections ( STIs ) are highest among sexually experienced adolescents and young adults, after controlling for sexual activity. Although some STI pathogens present as STI syndromes with a specific constellation of symptoms, most are asymptomatic and only detected by a laboratory test. The approach to prevention and control of these infections lies in education, screening, and early diagnosis and treatment.
Any adolescent who has had oral, vaginal, or anal sexual intercourse is at risk for acquiring an STI. Not all adolescents are at equal risk; physical, behavioral, and social factors contribute to the adolescent's higher risk ( Table 146.1 ). Adolescents who initiate sex at a younger age, youth residing in detention facilities, youth attending sexually transmitted disease (STD) clinics, young men having sex with men, and youth who are injection drug users are at higher risk for STIs. Risky behaviors, such as sex with multiple concurrent partners or multiple sequential partners of limited duration, failure to use barrier protection consistently and correctly, and increased biologic susceptibility to infection, also contribute to risk. Although all 50 states and the District of Columbia explicitly allow minors to consent for their own sexual health services, many adolescents encounter multiple obstacles to accessing this care. Adolescents who are victims of sexual assault may not consider themselves “sexually active,” given the context of the encounter, and need reassurance, protection, and appropriate intervention when these circumstances are uncovered (see Chapter 145 ).
Younger age at puberty
Cervical ectopy
Smaller introitus leading to traumatic sex
Asymptomatic nature of sexually transmitted infection
Uncircumcised penis
Early adolescence: have not developed ability to think abstractly
Middle adolescence: develop belief of uniqueness and invulnerability
Poverty
Limited access to “adolescent-friendly” healthcare services
Adolescent health-seeking behaviors (forgoing care because of confidentiality concerns or denial of health problem)
Sexual abuse, trafficking, and violence
Homelessness
Drug use
Young adolescent females with older male partners
Young men having sex with men
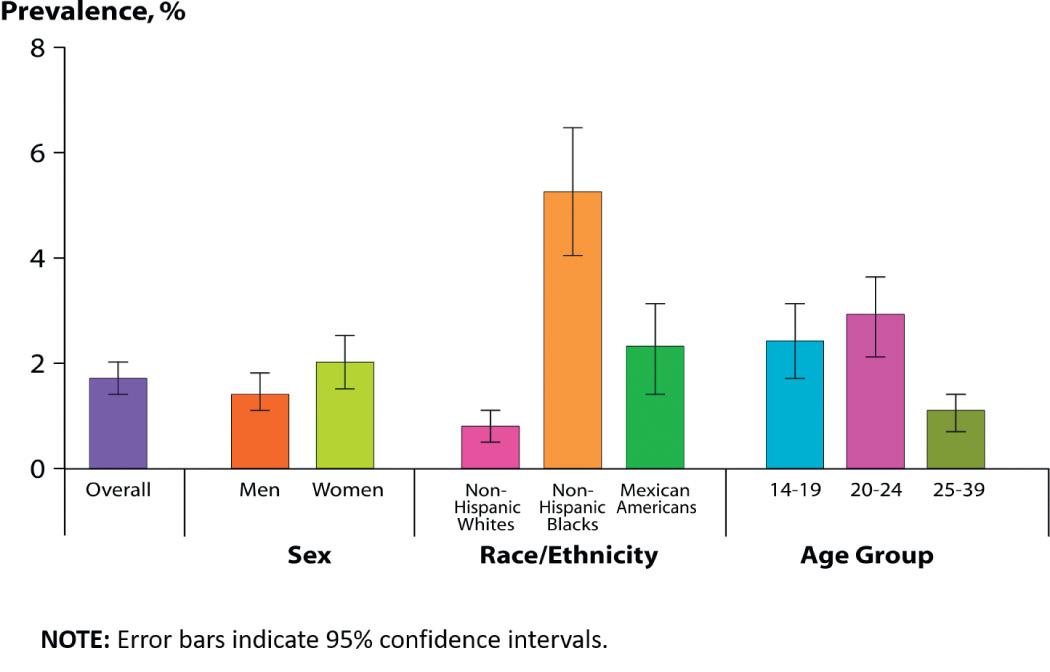
STI prevalence varies by age, gender, and race/ethnicity. In the United States, although adolescents and young adults ages 15-24 yr represent 25% of the sexually experienced population, this age-group accounts for almost 50% of all incident STIs each year. Adolescents and young adults <25 yr of age have the highest reported prevalence of gonorrhea (see Chapter 219 ) and chlamydia (see Chapter 253 ); among females and males, rates are highest in the 15-24 yr old age-groups ( Fig. 146.1 ). In 2015, females age 20-24 yr had the highest reported chlamydia rate (3,730 per 100,000 population), followed by females 15-19 yr of age (2,994/100,000). The reported 2015 chlamydia rate for 15-19 yr old females was almost 4 times higher than for 15-19 yr old males. Chlamydia is common among all races and ethnic groups; Blacks, Native American/Alaska Native, and Hispanic females are disproportionately affected. In 2015, non-Hispanic black females 20-24 yr of age had the highest chlamydia rate of any group (6,783), followed by black females 15-19 yr of age (6,340). Data from the 2007–2012 National Health and Nutrition Examination Survey (NHANES) estimated the prevalence of chlamydia among the U.S. population was highest among African Americans ( Fig. 146.2 ).
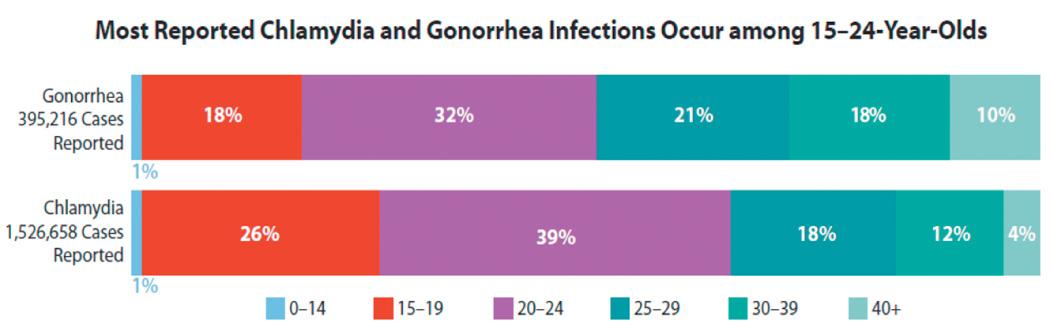
Reported rates of other bacterial STIs are also high among adolescents and young adults. In 2015, 20-24 yr old females had the highest (547/100,000) and 20-24 yr old males had the second highest gonorrhea rates (539/100,000) compared to any other age/sex group (see Chapter 219 ). Gonorrhea rates among 15-24 yr old males and females increased between 2014 and 2015. Syphilis rates are increasing at an alarming rate, especially among males, accounting for >90% of all primary and secondary syphilis cases. Of those male cases, men who have sex with men (MSM) account for 82% of male cases when the gender of the sex partner is known. Males age 20-24 yr have the 2nd highest rate of primary and secondary syphilis among males of any age-group (36/100,000); whereas rates among males 15-19 yr old (8/100,000) are much lower. Female primary and secondary syphilis rates are much lower than male rates (5/100,000 among 20-24 yr olds; 3/100,000 among 15-19 yr olds) (see Chapter 245 ). Pelvic inflammatory disease (PID) rates are highest among females age 15-24 compared with older women.
Adolescents also carry a large burden of viral STIs. U.S. youth are at persistent risk for HIV infection (see Chapter 302 ). In 2015, youth age 13-24 yr accounted for 22% (8,807) of all new HIV diagnoses in the United States, with most (81%) occurring among gay and bisexual males. Of those new infections, 55% (4,881) were among blacks, 22% (1,957) among Hispanic/Latinos, and 17% (1,506) among whites. Only 10% of high school students have been tested for HIV. Among male students who had sexual contact with other males, only 21% have ever been tested for HIV.
Human papillomavirus (HPV) is the most frequently acquired STI in the United States. According to NHANES, prevalence of HPV vaccine types 6, 11, 16, and 18 ( 4vHPV ) declined between the prevacccine (2003–2006) and vaccine (2009–2012) eras: from 11.5% to 4.3% among females age 14-19 yr and from 18.5% to 12.1% among females age 20-24 (see Chapter 293 ).
Herpes simplex virus type 2 (HSV-2) is the most prevalent viral STI (see Chapter 279 ). NHANES data show that among 14-19 yr olds, HSV-2 seroprevalence has remained low (<2%, in 1999–2010 surveys). In addition, according to NHANES, HSV-1 seroprevalence among 14-19 yr olds has significantly decreased, from 39% in 1999–2004 to 30% in 2005–2010, indicating less orolabial infection in this age-group. Studies have also found that genital HSV-1 infections are increasing among young adults. Youth who lack HSV-1 antibodies at sexual debut are more susceptible to acquiring a genital HSV-1 infection and developing symptomatic disease from primary genital HSV-2 infection. Increasing oral sex among adolescents and young adults also has been suggested as a contributing factor in the rise in genital HSV-1 infections.
During puberty, increasing levels of estrogen cause the vaginal epithelium to thicken and cornify and the cellular glycogen content to rise, the latter causing the vaginal pH to fall. These changes increase the resistance of the vaginal epithelium to penetration by certain organisms (including Neisseria gonorrhoeae ) and increase the susceptibility to others ( Candida albicans and Trichomonas ; see Chapter 310 ). The transformation of the vaginal cells leaves columnar cells on the ectocervix, forming a border of the 2 cell types on the ectocervix, known as the squamocolumnar junction. The appearance is referred to as ectopy ( Fig. 146.3 ). With maturation, this tissue involutes. Prior to involution, it represents a unique vulnerability to infection for adolescent females. The association of early sexual debut and younger gynecologic age with increased risk of STIs supports this explanation of the pathogenesis of infection in young adolescents.

Early detection and treatment are primary STI control strategies. Some of the most common STIs in adolescents, including HPV, HSV, chlamydia, and gonorrhea, are usually asymptomatic and if undetected can be spread inadvertently by the infected host. Screening initiatives for chlamydial infections have demonstrated reductions in PID cases by up to 40%. Although federal and professional medical organizations recommend annual chlamydia screening for sexually active females <25 yr old, according to the National Center for Quality Assurance, in 2015 among sexually active 16-20 yr old females, approximately 42% of commercial health maintenance organization (HMO) members and 52% Medicaid HMO members were tested for chlamydia during the previous year. The lack of a dialog about STIs or the provision of STI services at annual preventive service visits to sexually experienced adolescents are missed opportunities for screening and education. Comprehensive, confidential, reproductive health services, including STI screening, should be offered to all sexually experienced adolescents ( Table 146.2 ).
Routine screening for C. trachomatis and N. gonorrhoeae of all sexually active females aged <25 yr is recommended annually.
Routinely screen sexually active adolescent and young adult MSM at sites of contact for chlamydia (urethra, rectum) and gonorrhea (urethra, rectum, pharynx) at least annually regardless of condom use. More frequent screening (i.e., at 3-6 mo intervals) is indicated for MSM who have multiple or anonymous partners or who have sex with illicit drug use.
Consider screening for C. trachomatis of sexually active adolescent and young adult males annually who have a history of multiple partners in clinical settings with high prevalence rates, such as jails or juvenile corrections facilities, national job training programs, STD clinics, high school clinics, or adolescent clinics.
HIV screening should be discussed and offered to all adolescents at least once by age 16-18 yr and throughout young adulthood in healthcare settings. HIV risk should be assessed annually for >13 yr and offered if HIV risk factors identified.
Routinely screen sexually active adolescent and young adult MSM at least annually regardless of condom use. More frequent screening (i.e., at 3-6 mo intervals) is indicated for MSM who have multiple or anonymous partners or who have sex with illicit drug use.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here