Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The temporomandibular joint (TMJ) is a complex and unique joint unlike any other joint in the body, with both translational and rotational function, and repetitive complex movement patterns to accommodate the functions of speech, mastication, and swallowing. For these reasons, posttraumatic secondary reconstruction of this joint remains a challenging prospect for treating clinicians, and as TMJ reconstruction is performed far less commonly than other joints (knee and hip), this limits clinical experience in the field but also limits the amount of quantitative data for qualitative analysis. Following traumatic injury, it is not only the bony components of the joint, namely the mandibular fossa and condyle, but also the ligamentous and fibrocartilaginous components that may sustain injury, particularly the articular disk and the fibrocartilage joint lining. Condylar fractures account for around a quarter of all mandibular fractures highlighting the common nature of this type of injury. Potential late complications of traumatic TMJ injuries include facial asymmetry, malocclusion, growth disturbance, osteoarthritis, and ankylosis with potential functional problems. There are a variety of treatment modalities to manage these problems ranging from conservative to total joint replacement surgery, which largely depends on the extent of the problem and the clinical presentation. When the mandibular condyle is extensively damaged, degenerated or lost, replacement with either autogenous graft or alloplastic implant is an acceptable approach to achieve optimal functional and symptomatic improvement. The goals of TMJ reconstruction primarily are to improve mandibular form and function, to relieve pain where possible, provide cost-effective treatment and to avoid complications and morbidity. Mercuri reported indications for alloplastic joint reconstruction that include ankylosis or reankylosis with severe anatomical abnormalities and failed autogenous grafts in multiply operated patients. In this chapter, we will discuss these indications further, with emphasis towards posttraumatic secondary reconstruction.
Autologous TMJ reconstruction has been described in the literature since the early 1900s and has included the use of the metatarsal graft, costochondral graft, coronoid process, scapular tip, iliac crest, sternoclavicular, deep circumflex iliac artery flap and of increasing recent use, the fibula free flap. Indeed, with improved understanding and technical abilities of the reconstructive surgeon, autologous microvascular reconstructive techniques are now widely accepted as the “gold standard” for mandibular reconstruction. In the 1970s and 1980s, alloplastic joint reconstruction resulted in significant complications associated with prostheses containing Proplast–Teflon, where fragmentation on prolonged cyclical loading often resulted in a very locally destructive foreign body giant cell reaction. The subsequent litigation and FDA recall of these devices in the United States placed progress on hold for a period until the early 1990s where newer improved devices were introduced to the market. Currently, TMJ Concepts (Ventura, CA, USA) produces a patient-specific custom device utilizing CAD-CAM 3D technology, whereas Zimmer-Biomet Microfixation (Warsaw, IN, USA) produces both stock (in the United States) and custom devices (not available in United States). With now over 27 years of reported data, these devices have proven efficacy and safety, with outcomes similar or superior to standard orthopedic knee and hip prosthetic devices. Some common autologous and alloplastic TMJ reconstructive modalities will be discussed further in this chapter.
The TMJ is a bilateral ginglymoarthrodial (hinging and sliding) synovial joint between the condylar head of the mandible and glenoid or mandibular fossa on the undersurface of the squamous part of the temporal bone, together making a craniomandibular articulation (see Fig. 3.10.1 ). The joint is separated into an upper and lower compartment by a fibrocartilaginous disk that is biconcave in shape against the articulating surfaces within both compartments. The bony joint surfaces are covered with the same fibrocartilage which is less susceptible to degeneration and has a greater repair ability compared to hyaline cartilage found in other synovial joints. The mandible from condyle to condyle is a continuous entity and therefore movement in either TMJ is dependent upon the other whilst the extent and direction of movement is determined by the articulating surfaces, ligaments, and local musculature.
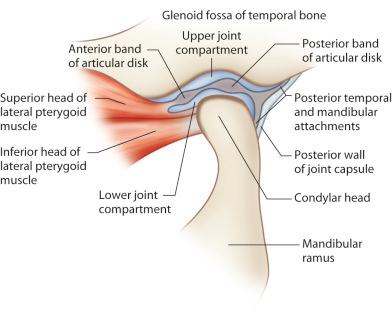
The collateral, capsular, and temporomandibular ligaments are direct anatomic components of the TMJs whilst the sphenomandibular and stylomandibular ligaments are attached at a distance from the joints. Collectively, they provide stability and control joint movement.
The muscles of mastication are the masseter, temporalis, medial pterygoid, and lateral pterygoid. The accessory muscles of mastication include the suprahyoid (digastric, geniohyoid, mylohyoid, and stylohyoid), and infrahyoid (sternohyoid, omohyoid, sternothyroid, thyrohyoid) muscle groups. When the mouth is opened, the condylar head undergoes rotation in the lower joint compartment while an anterior gliding motion occurs in the upper compartment. The lateral pterygoid and digastric are the main muscles involved in mouth opening whilst the masseter, temporalis, and medial pterygoids are the key muscles involved in mandibular elevation and subsequent mouth closure.
The potential long-term sequelae of TMJ trauma that may require reconstruction and management are:
Ankylosis
Condylar malunion/malposition with malocclusion and/or facial asymmetry
Degenerative joint disease
Failed primary reconstruction (autogenous/alloplastic)
Posttraumatic ankylosis of the TMJ injury is an uncommon complication of condylar injury and is of particular concern in pediatric cases where significant growth disturbances may result. This includes facial asymmetry, retrognathism, and secondary midface growth deficiency. In the adult patient, it may present as trismus with resultant compromised mastication, speech, oral hygiene, and even psychosocial distress. This complication usually results from comminuted intracapsular injuries, particularly when the articular disk is disrupted. It has also been suggested that concomitant anterior mandibular fractures, which allow posterior facial widening and consequent lateral displacement of fractured condyles, also increase the risk for this complication. Treatment can depend on the severity of the condition with various treatment modalities at the clinician's disposal, including gap arthroplasty, costochondral grafting, and total joint replacement. The growing patient offers additional reconstructive challenges and often requires further corrective surgeries consequential of dynamic changes in the growing patient. Complete bony TMJ ankylosis has been typically managed with gap arthroplasty, autogenous tissue graft or alloplastic arthroplasty. Autogenous grafting techniques usually require a period of immobilization postoperatively to allow adequate healing and limit the risk of graft failure resulting in mandibular functional delay. The lack of early mobilization and lack of soft tissue interface can risk reankylosis and should this occur, then total alloplastic reconstruction may be considered. In the growing patient, ankylosis of the TMJ may lead to asymmetrical mandibular growth resulting in height reduction of the affected ramus and subsequent facial asymmetry with chin deviation to the affected side, due to normal growth of the opposite side and impaired growth of the affected side. Compensatory occlusal disturbances may also occur such as overeruption and tipping of teeth to help reestablish functional occlusion. TMJ ankylosis in growing subjects has traditionally been managed by autogenous grafting, with the costochondral grafts as the most widely used method for these TMJ reconstructions. The rationale for autologous grafting is to maintain growth potential but growth and resorption can be unpredictable and other complications such as ankylosis have been reported.
Sawhney classified four types of pathological changes in the ankylosed TMJ. Type 1 describes flattening of the condylar head with surrounding dense fibrous adhesions making movement impossible. Type 2 includes a flattened or deformed condylar head, with close proximity to the articular surfaces, and a limited bony fusion of the outer, anterior or posterior surface. Type 3 includes a bony block bridging across the ramus and the zygomatic arch, with the displaced articular head fused to the medial side of the ramus, or the presence of an atrophic condylar head. Type 4 presents as a large bony block that completely replaces the usual joint architecture.
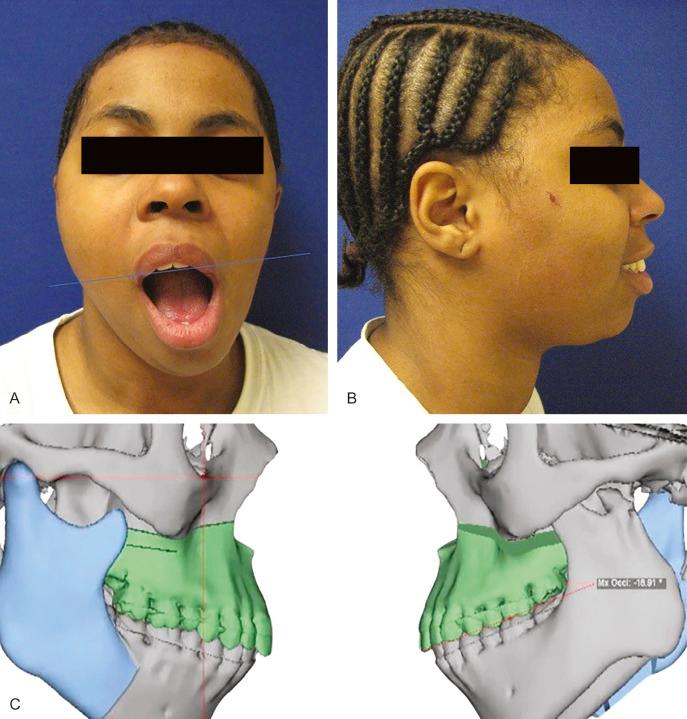
Loss of posterior mandibular vertical dimension due to traumatic injury can cause occlusal discrepancies as either an anterior open-bite where bilateral mandibular height is lost, or premature contact of the posterior teeth with contralateral open-bite where there is unilateral vertical height loss. Fig. 3.10.2 illustrates left condylar hypoplasia and the resultant loss of left vertical height in a young patient following an old traumatic fracture dislocation injury. In the absence of successful primary trauma reconstructive surgery or other management to help reestablish normal vertical height and correct occlusal discrepancies, then joint reconstruction (autogenous or alloplastic) or osteotomy may be considered. In the growing patient, loss of vertical height on the affected side may either be due to ankylosis and the resultant hypomobility or from direct injury to the condylar cartilaginous cap. It has been widely accepted for the growing patient where preservation of growth potential is desired, autogenous grafting such as the costochondral graft, is preferred over alloplastic TMJ reconstructive solutions. However, very good results using alloplastic devices in growing patients are emerging, with maintenance of facial symmetry in both unilateral and bilateral cases.
Traumatic injury to the TMJ, whether direct or indirect, can lead to osteoarthritic changes within the joint. Posttrauma joint effusion is well known in the orthopedic literature and has frequently been observed in posttraumatic imaging of the TMJ by magnetic resonance imaging (MRI), whilst other studies have shown arthroscopic evidence of TMJ articular damage following mandibular fracture injuries. The proinflammatory cytokine interleukin-6 (IL-6) has been shown to play a key role in the pathogenesis of arthritis and has been found in higher concentrations in TMJs with internal derangement and osteoarthritis when compared to TMJs without joint effusion. Nogami et al. found a correlation between MR evidence of joint effusion and concentration of IL-6 in washed-out synovial fluid samples collected from patients with mandibular condyle fractures. TMJ arthritis is one of the most common diseases affecting this joint and has a variety of other etiologies besides trauma, including inflammatory, infectious, metabolic, degenerative osteoarthritis, and systemic arthritides. Therefore, where preexisting disease is present, then certainly a traumatic insult can exacerbate the primary disease state. Symptoms depend on disease progression but patients may typically present with constant preauricular pain, with or without radiation and crepitus. Other symptoms may include TMJ locking, clicking, popping, and mandibular deviation on opening. Although a majority of patients earlier in the disease process will respond to nonsurgical treatment modalities or limited surgical intervention, when the mandibular condyle is extensively damaged, degenerated or lost, replacement with either autogenous graft or alloplastic implant is an acceptable approach to achieve optimal functional and symptomatic improvement.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here