Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
After the liver, the lung is the second most common site for metastatic involvement in neoplastic disease when all tissues and organs are considered, and 20% to 54% of patients with cancer will have pulmonary metastases at some point in the natural history of their disease ( Boxes 23-1 and 23-2 ). In the absence of extrathoracic metastases (i.e., in approximately 25% of patients with disseminated disease), retrospective data have shown that complete resection can be associated with increased survival, regardless of histology, in appropriately selected patients. Cures have been reported with either resection alone or in combination with chemotherapy. Surgical forms of palliation can improve quality of life. For some patients, surgery may have a complementary role, such as defining residual disease that is potentially amenable to salvage forms of therapy or obtaining adequate tissue for molecular testing for targeted therapies.
* Most common because of greater prevalence.
Breast
Colon
Kidney
Uterus
Prostate
Oropharyngeal carcinoma
Choriocarcinoma
Osteosarcoma
Testicular tumors
Melanoma
Ewing sarcoma
Kaposi sarcoma
During the 19th century, in the European literature there were sporadic reports of lung resections for metastatic tumors. The first of these reports was in 1855, by the French surgeon Sédillot, who removed a chest wall tumor and excised disease extending into the lung. The first case of a true pulmonary metastasectomy was described by Weinlechner in 1882 in a patient with a rib sarcoma, who was found to have two incidental pulmonary metastases at the time of the sarcoma resection. Kronlein reported the first long-term survivor after pulmonary metastasectomy in a patient with recurrent chest wall sarcoma and a metastatic lung nodule. The patient went on to survive 7 years, eventually succumbing to recurrent pulmonary disease.
The first, and perhaps most famous, report of a planned pulmonary metastasectomy in the United States was performed in 1933 by Barney and Churchill. Soon after resection of a renal cell carcinoma, they noted that the patient's pulmonary nodule, seen on a chest radiograph preoperatively and presumed to be tuberculosis, had doubled in size. The lesion, now thought to represent metastatic disease, was treated with radiation therapy. They noted a poor response and elected to resect the nodule. The patient went on to live 23 years, eventually dying of coronary artery disease with no evidence of tumor recurrence at autopsy. Despite the early discovery (in the late 1800s) that survival could be improved by resection of metastatic disease, it was not for another 40 years that metastasectomy was performed as a separate procedure by Divis in Europe. This was followed soon after by similar reports in the American literature by Torek and Tudor Edwards in the early 20th century.
These early reports, and others like them, paved the way toward general acceptance of pulmonary metastasectomy. Although initial indication for surgery was reserved for those with a solitary metastasis, with time and experience, surgeons began to perform more aggressive metastasectomies. In 1947, Alexander and Haight described the first case series of 24 patients who underwent pulmonary metastasectomy. In this series, they described a young woman with a spindle cell neurogenic sarcoma. She initially underwent a right lower lobectomy for metastatic disease in 1939. She had a recurrence in 1940 for which she underwent a left upper lobectomy. This article was the first to define criteria for resection of pulmonary metastases, including control of the primary tumor, absence of extrathoracic disease, and sufficient pulmonary reserve.
The largest effort aimed at evaluating patients undergoing pulmonary metastasectomy was undertaken by the International Registry of Lung Metastases (IRLM). Established in 1991, the IRLM accrued 5206 patients in North America and Europe. This landmark report demonstrated that complete resection, long disease-free interval, and single lesions were associated with better long-term survival. This and other studies have helped to develop current criteria for performing pulmonary metastasectomies and to define anticipated survival after resection.
In 1889, British surgeon Stephen Paget observed that metastatic disease followed a nonrandom pattern. Using autopsy records of patients with a variety of primary tumors, he hypothesized that factors in certain tumors have an affinity for certain factors in target organs. Theories have subsequently evolved that attempt to explain the propensity for metastases to spread to specific organs. The “cascade spread” theory hypothesizes that a single organ represents the first site of spread, followed by systemic dissemination. This metastatic cascade is considered to be a complex series of events culminating in the generation of metastases. The initial phase of the cascade involves tumor growth via neovascularization, which is stimulated by growth factors secreted by the tumor cells and local host cells. The invasive phase of tumor growth involves the local production and activation of proteolytic enzymes (matrix metalloproteinases, collagenases, serine proteinases, cysteine proteinases) derived from both the host and tumor tissue. These enzymes decrease cell adhesiveness, stimulate cell migration, and enhance chemotaxis and subsequent tumor cell detachment.
Metastasis is most likely initiated after cell detachment from the primary tumor mass. Typically, epithelial cells undergo anoikis (apoptosis) because of the loss of cell-cell interactions once they are separated from parent tissue. Metastatic cells are thought to resist anoikis by forming cell-cell attachments with other tumor cells or host cells and through the overexpression of proteins that inhibit anoikis.
Movement from the extracellular space into a vascular compartment is termed intravasation . Cancer cells have been shown to degrade basement membranes via local release of extracellular matrix-degrading proteins (matrix metalloproteinases), facilitating migration into the lymphatic and circulatory system. Once in the circulatory system, tumor cells must avoid recognition and destruction by the host immune system. Only 0.1% of tumors cells in circulation go on to generate metastases. Mechanisms that cancer cells use to survive include human leukocyte antigen (HLA) class I downregulation (mediator of immune cell recognition) and loss of immunogenic antigens. Cancer cells also downregulate the immune system via the production of immunosuppressive cytokines. Some evidence suggests that clots form around tumor cells that protect these cells from immunologic and physiologic stresses in the bloodstream.
Tumor cells bind to pulmonary vasculature, which, via a platelet-induced reaction, stimulates endothelial cell retraction. The lung is thought to play a role as the primary capillary filter for drainage of most organs, and its rich capillary network provides an ideal environment for deposition. Movement of tumor cells from the circulatory system into the interstitium is called extravasation . Basement membrane disruption is thought to occur in a manner similar to intravasation.
Once extravasated, tumor cells may remain quiescent or they may proliferate. Proliferation and local invasion require neovascularization, which is induced via a shift toward the intracellular and extracellular production of pro-angiogenic factors. Epidermal growth factor (EGF), platelet-derived growth factor (PDGF), and transforming growth factor-α (TGF-α) foster tumor cell proliferation in the new environment. On the other hand, the host organ produces inhibitors, such as TGF-β, mammastatin, and amphiregulin, to prevent metastatic implantations. These compounds are under investigation to assess their ability to control metastatic disease.
It is thought that metastases need to follow the same steps as the primary tumor to metastasize: angiogenesis, intravasation, arrest, and extravasation. In 1975, Hoover and Ketcham demonstrated, experimentally, that metastases do have the ability to metastasize. In this experiment, the primary tumor in mice was amputated after pulmonary metastasis developed. These mice were then placed into parabiosis with normal syngeneic partners. Metastases were demonstrated in the non–tumor-bearing partners, supporting the theory that metastases can re-metastasize. In addition, both autopsy and experimental data have defined the concept of metastases from metastatic disease. Further support of this concept is provided by the presence of intrathoracic lymph node metastases among patients who undergo anatomic resection and lymph node dissection for metastatic lung disease, especially for renal cell carcinoma (46.6%) and colon cancer (9.8%). On the other hand, Sugarbaker and colleagues took pieces of healthy lungs and transplanted them into mice that had established pulmonary metastases. Their results demonstrated no evidence of secondary tumor development, this leading to the conclusion that metastases do not metastasize.
Whether metastases metastasize is still poorly understood and remains a challenge for medical oncologists and surgeons as they struggle to determine the best treatment and the proper timing of that treatment for patients with pulmonary metastases.
Lung cancer can metastasize via lymphatic channels to the ipsilateral lung and, as suggested by some autopsy series, less commonly to the contralateral lung. These are patients with one primary lung cancer and intrapulmonary metastases. According to the seventh revision of the lung cancer staging system of the International Association for the Study of Lung Cancer (IASLC), ipsilateral nodules in the same lobe as the primary tumor will be considered T3 and nodules in a different ipsilateral lobe from the primary tumor will be considered T4. It is difficult, however, to determine if these patients have synchronous lesions or a primary lung cancer with intrapulmonary metastases. Ichinose and coworkers have used DNA flow cytometry to evaluate these lesions. Using this technique, lesions are determined to be synchronous if they demonstrate completely different DNA ploidy. If both tumors show diploidy, or when at least one DNA index of abnormal clones between two aneuploidy tumors is the same or almost identical, they are considered metastatic. In addition, loss of heterozygosity and p53 mutational status have been used to distinguish multicentric lung cancers from intrapulmonary metastases. Using these criteria, it appears that lung cancer can metastasize to lung, albeit less commonly than synchronous tumors.
Because approximately 75% to 90% of patients with secondary pulmonary malignancies are asymptomatic, their disease is most commonly discovered incidentally on routine or follow-up radiologic examinations. Absence of symptoms is predominantly due to the usual peripheral location of pulmonary metastases. The asymptomatic nature of pulmonary metastases makes necessary the practice of obtaining lung-imaging studies in the follow-up of most cancer patients.
Symptoms, when they do occur, typically occur with endobronchial or pleural involvement, large bulky disease, or central venous obstruction. Patients may have symptoms of cough and hemoptysis suggesting an endobronchial lesion and thus warrant bronchoscopic examination. Endobronchial metastatic lesions are extremely rare in patients who die of solid tumors, with breast, kidney, pancreas, colon, and melanoma as the most common sources. Dyspnea may occur, which is usually secondary to airway obstruction, a pleural effusion, extensive parenchymal replacement by multiple metastatic lesions, or lymphatic spread. Finally, chest pain, wheezing, or pneumothorax may occur, but these are unusual presenting symptoms.
During physical examination, wheezing may be heard, which is a sign of airway obstruction. Occasionally, a pericardial rub is heard, representing pericardial involvement. Pleural or pericardial involvement is usually the result of ovarian, breast, or lung adenocarcinomas. Thymic malignancies are notorious for pleural involvement when they metastasize. In addition, decreased breath sounds and egophony may be appreciated when an obstructing lesion is present with associated lobar or segmental atelectasis, which could be seen on a chest radiograph as postobstructive pneumonia.
Most pulmonary metastases are detected by chest radiography ( Fig. 23-1 ) or computed tomography (CT) ( Fig. 23-2 ) during routine follow-up for the primary cancer. Radiologic testing is used to define the extent of the disease and to determine whether an individual is a candidate for pulmonary metastasectomy. A search for extrathoracic disease may involve imaging the original primary disease site as well as looking for distant disease. A new pulmonary nodule in a patient with a prior malignancy should be considered cancer until proven otherwise.
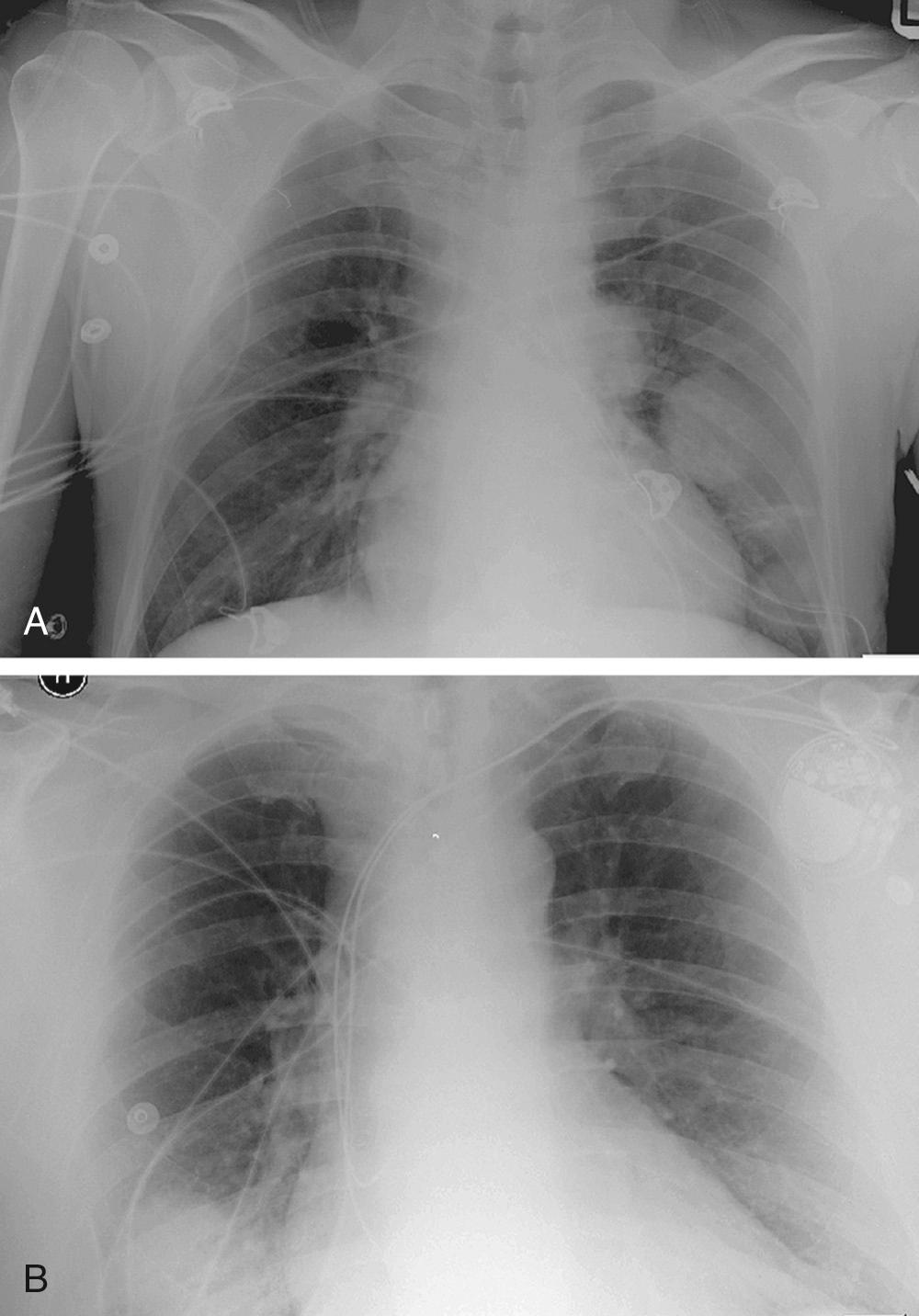
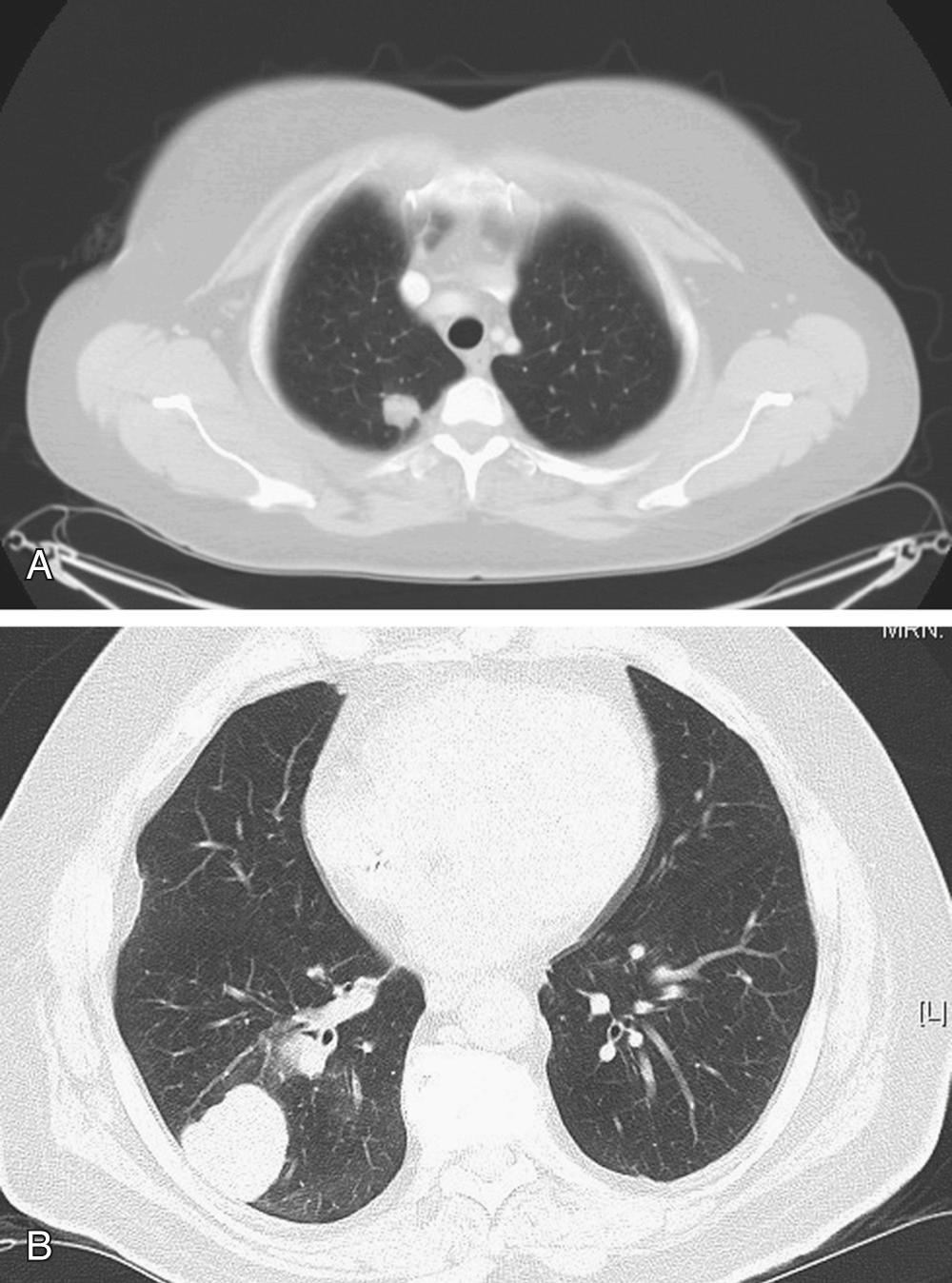
Because of its higher resolution, helical CT is the gold standard imaging modality for evaluation of the lungs and characterization of metastatic lesions. Lung metastases can be small (usually less than 1 cm), and they appear as multiple lesions in 75% of cases. Most metastatic lesions to the lung are found on the lung periphery, and they have a predilection for the basilar lung fields, probably because of increased blood flow to this region when the patient is in an upright position. Distinguishing between a metastatic lesion and other malignant or benign lung lesions can be difficult. CT characteristics of metastatic lesions include spherical shape with well-circumscribed, smooth borders. Lesions with irregular or spiculated borders with associated linear densities are more commonly associated with primary lung cancers, although this is not a universal finding. Calcifications in lung nodules are rarely seen in metastatic pulmonary disease. Metastases that may have associated calcifications include osteosarcomas, chondrosarcomas, and breast and ovarian cancer. Cavitation can occur in benign lesions such as those caused by lung abscess, aspergillosis, or tuberculosis. Malignant nodules that can cavitate include squamous cell carcinoma (primary lung or metastatic carcinomas), sarcoma, and testicular tumors.
Positron emission tomography (PET) is imperative when considering patients for metastasectomy. In a series of patients with melanoma, 18 F-fluorodeoxyglucose (FDG)-PET had a sensitivity of 92%, a specificity of 88%, and accuracy of 91%. PET is helpful in assessing extent of disease, including the primary disease site as well as thoracic and extrathoracic potential sites of metastases. However, PET positive findings should be interpreted with caution because of the low specificity of positive results. When considering surgical management of metastatic lung disease, all potential sites of metastatic disease identified on CT and PET should be thoroughly evaluated, particularly in the mediastinum, because tissue confirmation of multiple organ involvement will likely change management. Although CT is useful for identifying and characterizing pulmonary metastases, caution must be exercised because intraoperative pulmonary palpation may identify smaller parenchymal lesions not detected with imaging.
Multiple nonsurgical options are available for confirmation of a histologic diagnosis. These options, including endoscopic procedures and percutaneous needle aspiration, should be used when management will change based on the results. This is particularly true for patients that are borderline surgical candidates or who refuse surgery but desire alternative treatment.
Sputum cytology is of historical interest and has been replaced by bronchoscopy, as it is often nondiagnostic because of the peripheral location of most pulmonary metastases. Bronchoscopic examination and diagnosis of pulmonary metastases is useful in the case of endobronchial or centrally located lesions. Peripheral radial ultrasound probes or electromagnetic guidance systems may increase the yield of endobronchial sampling. Percutaneous fine-needle aspiration (FNA) is another option for obtaining a tissue diagnosis. It is associated with a risk of pneumothorax, in some series as high as 27%. Unfortunately these procedures are plagued by low sensitivity, such that equivocal or “negative” results do not establish a diagnosis of benign disease. In addition, in the current era of molecular and genomic testing, obtaining ample tissue for processing with these less invasive techniques can be difficult and could require multiple procedures. If tissue diagnosis is desired but less invasive means have failed to obtain adequate tissue, video-assisted thoracic surgery (VATS) with excisional biopsy is recommended. VATS has a sensitivity and specificity approaching 100%. It is a more invasive procedure than FNA and requires general anesthesia with selective lung ventilation. Also, when extent of metastatic disease is limited, it may be therapeutic as well as diagnostic, as the nodules can be completely excised. Occasionally, there is a role for thoracoscopic core needle biopsy, such as in cases of multiple lesions not amenable to complete surgical resection when treatment hinges on a tissue diagnosis and all less-invasive diagnostic modalities have proved fruitless or are deemed less safe than a VATS approach.
Because the pretest probability of malignancy is high in a patient with a lung nodule and history of malignancy, the negative predictive value is low if cancer is not identified on a specimen obtained percutaneously or with bronchoscopy. For this reason, nonsurgical procedures aimed at obtaining a histologic diagnosis should be used selectively, and multidisciplinary evaluation with a surgeon and oncologist is of the utmost importance. In this setting, diagnostic procedures can be selected based on risk profile, local expertise, and anatomic location of the lesion with the aim of proceeding to an appropriate therapy.
Reasons to perform surgery for secondary pulmonary malignancy include curative resection, tissue diagnosis, or evaluation of residual disease. Before proceeding with resection, a number of questions should be considered in the preoperative assessment of the patient.
Does the pulmonary nodule represent one site of multiorgan spread, thereby contraindicating resection? Pulmonary metastases are common in the advanced stages of cancer, with as many as one third of patients presenting with secondary nodules. Of these patients, however, most pulmonary nodules (75% to 85%) are a manifestation of widespread disease. Consequently, only 15% to 25% of patients have lesions confined to the lung and are appropriate candidates for curative resection ( Table 23-1 ). Preoperative evaluation, therefore, should exclude extrathoracic disease.
| Histology | Most Common Site of Metastasis (%) | Second Most Common Site of Metastasis | Those with Isolated Pulmonary Metastases (% of All Patients) |
|---|---|---|---|
| Breast carcinoma | Lung (59-65) | 22 | |
| Colorectal | Liver | Lung | 2-4 |
| Germ cell tumors | Lung | ||
| Head and neck squamous cell carcinoma | Lung (75) | ||
| Melanoma | Lung * † (18-36) | 5 | |
| Osteosarcoma | Lung (85) | ||
| Renal cell carcinoma | Lung | 4 | |
| Soft tissue sarcoma | Lung (80-90) | 20 | |
| All histologies | Liver | Lung | 15-20 |
* Secondary to skin, subcutaneous, lymph nodes.
† In clinical series; however, 70% to 87% in autopsy series.
When pleural or pericardial effusion is present, thoracentesis or pericardiocentesis should be performed to evaluate for malignancy. Positive cytology contraindicates resection. Cytology may be falsely negative, however, in up to 40% to 60% of cases. Consequently, a negative cytology returned in the context of a high index of suspicion for malignant effusion warrants pericardial or pleural biopsy, or both. A VATS approach can be used to access the pleural space, and it offers a minimally invasive transthoracic approach to the pericardium. It also affords the option of visualizing and palpating the lung as well as sampling the mediastinal lymph nodes. Bronchoscopy should always be performed before thoracoscopy or thoracotomy, to evaluate for endobronchial lesions.
Is a nonsurgical therapeutic option available? Although surgical resection of secondary pulmonary malignancies may give patients a significant survival advantage, nonsurgical management may be more appropriate for certain cancers. For example, in the context of nonseminomatous germ cell tumors, great success has been obtained with chemotherapy, with cure rates approaching 90% (see “ Germ Cell Tumors ,” later). In addition, alternative therapies such as radiofrequency ablation or stereotactic body radiation may be appropriate in selected cases (see “ Alternative Treatment Options ,” later).
Will the patient tolerate the procedure? Risk factors associated with metastatic disease (e.g., smoking and advanced age) require that patients being considered for surgical resection receive a thorough medical assessment with particular attention to their pulmonary and cardiac status. Stress testing, echocardiograms, arterial blood gases, pulmonary function testing, and ventilation-perfusion scans may be necessary to assess patients' tolerance for a proposed resection or their ability to undergo single-lung ventilation. Also, previously administered chemotherapeutic agents such as bleomycin or mitomycin may result in additional compromise of pulmonary function, and doxorubicin may be associated with cardiac impairment. In addition, the thoracic surgeon expecting to perform a metastasectomy must always be prepared to perform a formal lobectomy should the pathology reveal a primary lung cancer or should wedge resection result in incomplete resection. Thus, performing the preoperative assessment with consideration for anatomic resection and its attendant risk is prudent.
Are the lesions resectable? Unresectability is defined as noncontiguous involvement beyond the visceral pleural envelope. This is best determined at operation. Preoperatively, imaging modalities can only provide an estimate of resectability. In addition, thoracoscopy can sometimes be useful to assess for disseminated disease or bulky tumors that involve major structures and preclude complete resection. If the pericardium or pleura is involved with neoplastic disease from direct extension of an underlying parenchymal lesion, but there is no associated effusion, they should be resected en bloc with the specimen. Direct metastases to the pleura or pericardium in a discontinuous manner (i.e., disseminated spread) and malignant pleural or pericardial effusions are generally contraindications for resection.
Is the primary tumor controlled? Efficacy of pulmonary metastasectomy depends on, among other factors, the ability to control the primary site of disease. The primary neoplasm should generally be addressed before resection of the pulmonary metastases. Therefore, thorough preoperative testing should be performed to rule out other possible metastatic sites or local recurrence of the primary tumor prior to pulmonary metastasectomy ( Box 23-3 ).
* Approximately one third of patients with metastatic disease meet these criteria.
for Metastasectomy
Local control of the primary tumor or ability to completely resect the primary with synchronous presentations
Radiologic findings consistent with metastatic disease
Absence of extrathoracic metastases (i.e., metastasis is confined to the lung)
Ability to perform a complete resection of the metastases
No significant comorbidity that would preclude surgery
No alternative therapy that is superior to surgery
Alexander and Haight, in the 1940s, were the first to describe specific selection criteria for consideration of pulmonary metastasectomy. They realized that the benefits of surgical resection depended on primary tumor control, absence of extrathoracic spread, and adequate patient selection. Approximately one third of patients meet these selection criteria and can appropriately undergo metastatic resection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here