Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
There has been a contemporary resurgence in the desire to understand scapula fractures in a way that aligns its diagnosis and treatment with other fractures considered by the orthopaedic surgeon. Perhaps this resurgence relates to the recognition that the significant deformity of scapula malunion leads to substantial dysfunction, supporting the well-known AO axiom that musculoskeletal function follows skeletal form. Additionally, rendering stability to the unstable and displaced shoulder blade fracture expedites pain relief and functional recovery, as it does with other fractures surgically treated with open reduction and internal fixation (ORIF).
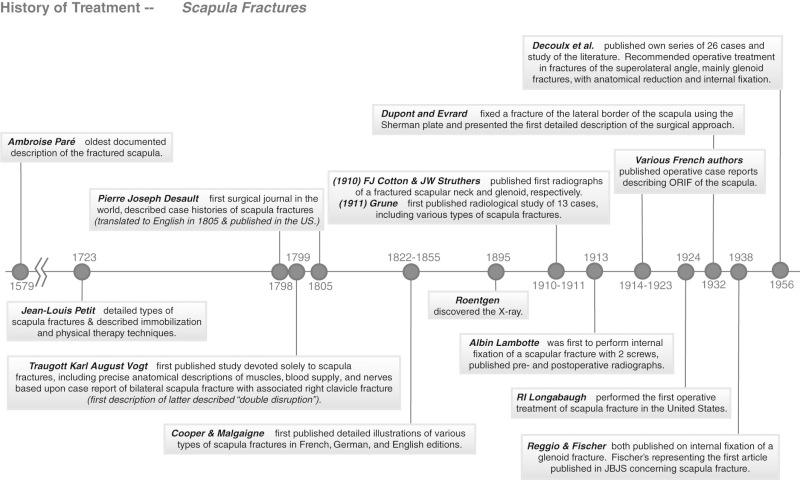
Contextually, it is important to understand, however, that the surgical treatment of scapula fractures is neither a new phenomenon nor a by-product of a surgically oriented culture in orthopaedics. A timeline of historic milestones in the diagnosis and management of scapula fractures lends credence to a contemporary frontier in orthopaedic trauma ( Fig. 49.1 ). Scapula fractures were first elucidated, distinguishing fractures of the body, neck, and processes, in 1723 by the extraordinary work of Jean Louis Petit and then described and documented radiographically by Grune in 1911. In 1913 the Belgian, Albin Lambotte, published the first report of scapular fracture treated with ORIF from a case completed in 1910. Several important operative case reports followed through the early part of the 20th century, with the greatest documented track record in France. It was not until 1924 that Longabaugh published the first series from the United States, and then in the same decade Reggio and then Fischer published intraarticular scapula fracture series. Despite larger surgical series emerging by Decoulx et al., Tondeur, and Judet, a nonoperative opinion of management was being espoused by Rowe and Schnepp and colleagues, which influenced a new generation of orthopaedic surgeons through the latter part of the past century. During this period, patients were simply exhorted to immobilize in a sling until pain resolved to an extent that would allow them to move again. This approach of expectant management retained a foothold through the first decade of this millennium under the guise that nearly all scapula fractures heal, and the shoulder has a capacity for compensating due to its global motion. This rationale was applied to nearly all patients except for the most significantly displaced intraarticular glenoid fractures, where there was general acceptance of the need to restore articular congruency. The problem remained, however, that there were few trained in the treatment of this fracture, and no detailed descriptions of the surgical approaches.
This chapter builds on a new perspective of operative intervention in cases of marked displacement, by elucidating newer evidence that highlights dysfunction in subgroups of patients with malunion. The results from large operative series of severely displaced fractures will be detailed, the current evidence on outcomes after surgical and nonsurgical treatment will be highlighted, and new as well as historical operative approaches will be described to aid the surgeon in operative management of indicated patients.
Surgical indications will be clearly defined and placed within the context of the patient as a potential surgical candidate. Diagnostic approaches along with methods of measuring displacement and angulation will be clearly described to aid the surgeon in decision making. In addition, since surgical scapula fractures rarely occur in isolation, we will highlight the importance of a careful survey and consideration of the whole patient beyond the scapula, given the enormous associated injury rate with these fractures.
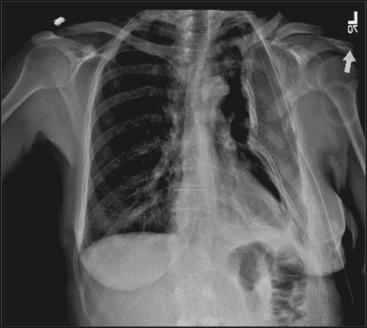
The majority of scapula fractures are the result of high-energy blunt trauma, as evidenced by an associated injury rate of 80% to 95% in operative series. The two most common mechanisms are motor vehicle collisions and falls ranging from 37% to 78% and 4% to 23%, respectively. Recreational motorized vehicles and cycling injuries are also very common mechanisms seen in practice today, but nearly all result from forces to the superior and lateral shoulder causing an implosion of the thoracic cavity ( Fig. 49.2 ). More recently, periprosthetic fractures have also been reported, and there is evidence that the incidence in fragility fractures of the shoulder blade is increasing. Further work by the senior author, examining the National Trauma Databank for the past decade, emphasizes this growing trend in scapula fragility fractures, while overall, those from motor vehicle accidents has declined.
The proximal forequarter's extraordinary mobility is attributed to the shallow glenoid fossa in which most of the stability is maintained by the compressive loading of opposing shoulder muscles and the labrum. The well-developed shoulder capsule provides the remainder of the restraint, and these structures become much more relevant in scapula malunion where muscular force vectors are imbalanced and aberrant in opposing muscles.
The dynamic relationship of the humeral head to the glenoid, with all the muscles acting across this joint, has been likened to the balance of a ball on the nose of a seal with all the adjustments necessary to maintain equilibrium. The extensive musculature often can sufficiently compensate for alterations in its lever system, inclusive of the anatomic bone structure as well as correct activation of vector and force of the parascapular musculature. Recent studies have suggested that muscle dysfunction may contribute to multidirectional instability and impingement syndrome. Additionally, biomechanical and clinical studies have shown that severe displacement can result in functional alterations and unsatisfactory outcomes if treated nonoperatively.
Scapula neck malunions have been shown in biomechanical models to result in a loss of strength and altered muscle activation during abduction. As the glenoid medializes or rotates inferior relative to the body and lateral border of the scapula, the rotator cuff shortens; this takes tension off these muscles, which have essential upper extremity function, including the proper loading (vector and force) of the glenoid fossa. Compressive muscular forces change to shear forces as a function of this aberrancy. Gauger et al. documented by quantitative three-dimensional (3-D) shoulder motion analysis the altered motion in a scapular malunion patient, which was shown to be normalized after surgical reconstruction of the scapula and clavicle. Correct muscle vector and force of the parascapular muscles are imperative for glenohumeral joint stability. Eighteen muscles originate, insert, or cross the scapula and glenohumeral joint, and recent studies have shown that these parascapular muscles do contribute to dynamic stabilization that occurs during motion.
A recent series of reconstructions of highly symptomatic scapula malunions was published by the senior author (PAC), demonstrating marked recovery of function, motion, and strength 2 years after surgery, yielding clinical support to the bench research and theoretical arguments about the relevance of aberrant muscular force vectors. A more recent larger series was presented by the senior author at the 2017 Orthopaedic Trauma Association (OTA) in which 26 patients with 34 malunions and/or nonunions of the scapula also demonstrated statistically significant improved motion, strength, and functional outcome (see ).
Fractures of the glenoid rim and fossa affect shoulder stability by decreasing the surface area of the joint, much as would happen to a golf ball when the head of a tee is partly missing. Typically, in isolated glenoid fractures, if greater than approximately one-fourth of the anterior or posterior glenoid is displaced, there is inadequate constraint. The intact labrum itself is 2 to 4 mm in depth and matches the pear-shaped glenoid to provide proper constraint. Certainly the extent of the associated labral and capsular injury factors into this phenomenon and contributes to the threshold for subluxation, which leads to more progressive posttraumatic degenerative joint disease.
It is vital to perform a thorough evaluation of any patient presenting with a scapula fracture because of the great associated injury rate detailed in operative series. From these operative series, which represent the severe end of the energy spectrum, we know that a keen workup will yield positive findings for associated upper extremity fractures in up to 50% of patients, brachial plexus and peripheral nerve lesions in about 10%, significant chest injury in over 80%, and cervical spine and traumatic brain injury in 15%. Thus it is paramount that a thorough physical examination with a critical secondary survey should augment the three radiograph views of the shoulder and a chest radiograph. Clearly, prioritization of injuries in terms of treatment is necessary alongside the full trauma resuscitation of patients.
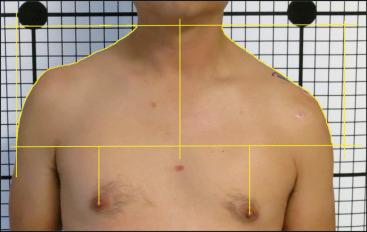
In awake and cooperative patients, ask where they have pain and allow the response to direct the physical examination. Observe the patient for shoulder asymmetry. The displaced scapula fracture will be associated with a slumped or depressed shoulder, if not medialized, due to the common displacement ( Fig. 49.3 ). This deformity becomes more apparent in some patients, particularly those who are upright and ambulatory after the injury. This deformity can be rather grotesque, and often serves as the clearest motivation for the patient to consider surgery. The skin should be inspected for abrasions and scabs, particularly over the prominent acromion ( Fig. 49.4 ). This finding should affect surgical timing.

In a patient with a known scapula fracture, the neck should be assessed for tenderness, and deep palpation of the clavicle and thorax should be performed to direct further radiographic assessment for the common ipsilateral rib and clavicle fractures. It should be assumed that the shoulder will hurt with motion, but active forward elevation should be attempted to delineate minimally displaced variants not requiring surgery from those variants in which shoulder motion of any magnitude is extremely painful. Specifically palpate the acromioclavicular (AC) and sternoclavicular joints, sites of sometimes subtle but relevant findings. Take the wrist and elbow through a full active and passive range of motion examination. Next, pulses at the wrist and a detailed neurologic examination of C5-T1 should be documented. Axillary nerve lesions are particularly common, yet may only be detected by sensory examination because of the inability for active motion of the patient's shoulder. Likewise, suprascapular nerve lesions are very common in displaced scapula fractures, but due to most patients’ inability to externally rotate because of pain, these findings often manifest later in treatment.
In the intubated or obtunded patient, palpation and motion to detect crepitance is important, including subcutaneous crepitance along the thorax and neck region, which will be positive in many patients with pneumothoraces. This finding may direct the placement of a chest tube unless already performed by the trauma service. As stated previously, every bone and joint should be palpated and inspected to assess for swelling, crepitance, instability, and pain because of the associated injury rate in up to 90% of all patients that meet surgical indications.
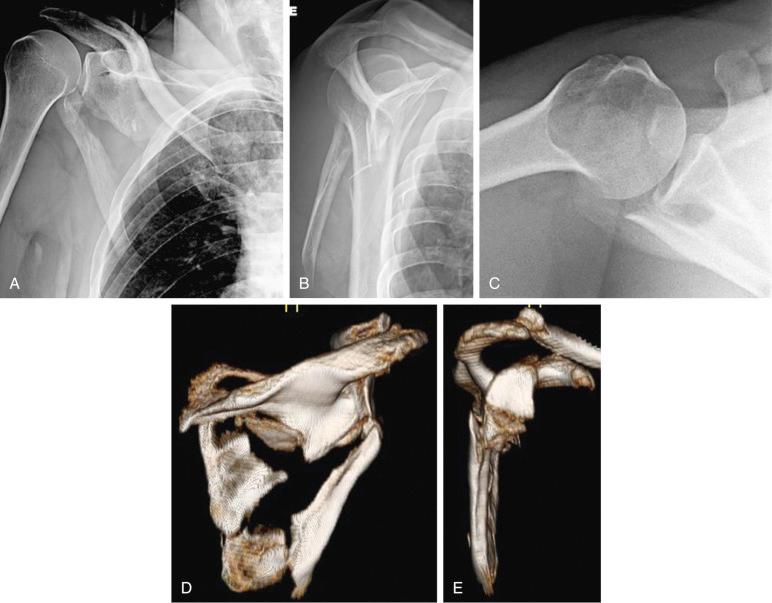
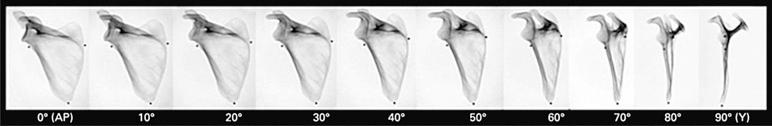
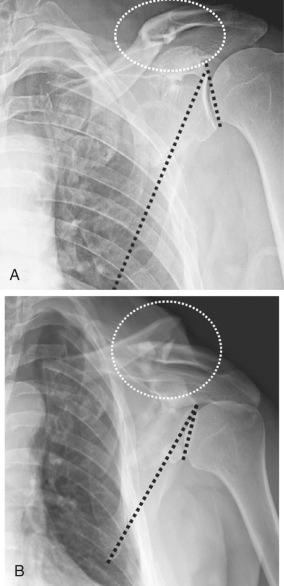
A chest radiograph and computed tomography (CT) scan will often be the first opportunity to identify a scapula fracture presenting in the emergency department. Chest radiograph alone can often miss a scapula fracture, particularly poorly executed chest radiographs. Therefore blunt chest trauma associated with shoulder pain, deformity, or the radiographic presence of other ipsilateral injuries warrants dedicated shoulder imaging. Three plain radiograph views should be evaluated: anterior-posterior (AP) Grashey, scapula-Y, and axillary views ( Fig. 49.5A–C ). Correct positioning and exposure are imperative to both diagnosis and evaluation of displacement. The glenoid articular surface will appear as a sharp crescent when a satisfactory true AP view is obtained ( Fig. 49.6 ). A satisfactory transscapular Y view is characterized by the radiodensity from the acromion base oriented posteriorly, and the coracoid anteriorly with the overlapping superomedial angle, and finally the distal arm consisting of the bony overlap of the lateral and medial borders of the body, at least in the intact or nondisplaced state. Often the radiology technician will claim not to be able to obtain an axillary view due to the infliction of pain to the patient; however, patient tolerance is increased by having the patient hold an intravenous (IV) pole during 30 degrees of shoulder abduction and elevation, while the radiograph gantry is positioned parallel to the patient's body shooting up into the axilla.
It is not uncommon to be misled by displacement and fracture patterns seen on conventional shoulder radiographs.
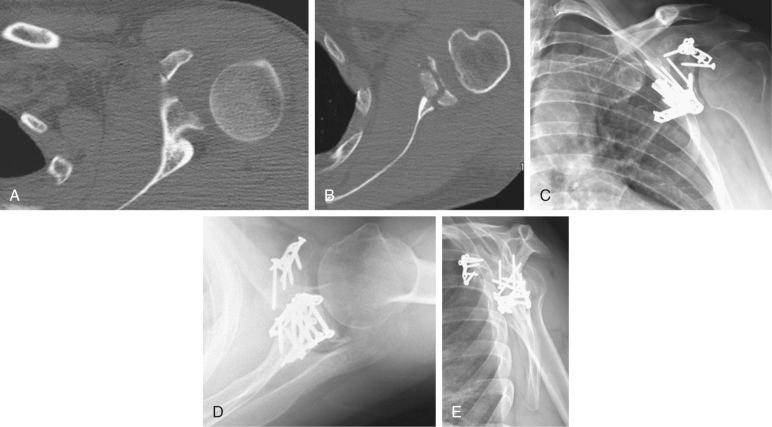
CT scans with 3-D reconstructions (see Fig. 49.5D and E ) have proven to be a gold standard and should be obtained in patients under surgical consideration for ORIF of displaced scapula body and neck fractures. In the study performed by Anavian et al., the measurement of medialization, angulation, glenopolar angle, and translation of scapula was assessed in 45 patients having both radiographs and 3-D CT of their shoulder fractures. Three-dimensional CT showed higher intrarater and interrater reliability in measuring displacement accurately.
Certain extraarticular injury patterns may be prone to progressive deformity in the early postinjury period. Therefore it is recommended that serial radiographs be obtained on a weekly basis for up to 3 weeks after injury.
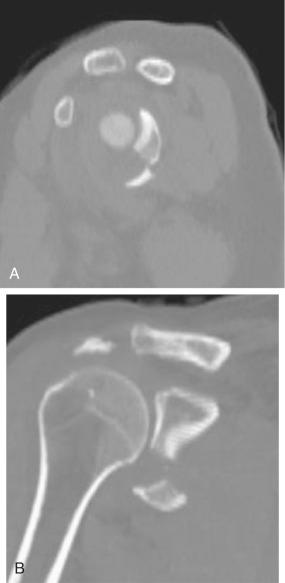
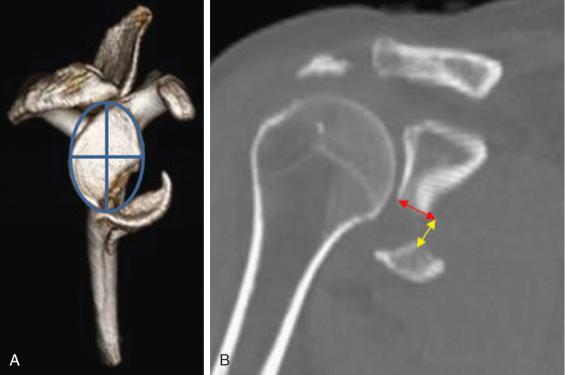
Articular displacement and measurement of step and gap, is best visualized on two-dimensional (2-D) CT ( Fig. 49.7 ). Critical assessment of each scapula process and the articulations at each end of the clavicle is also important.
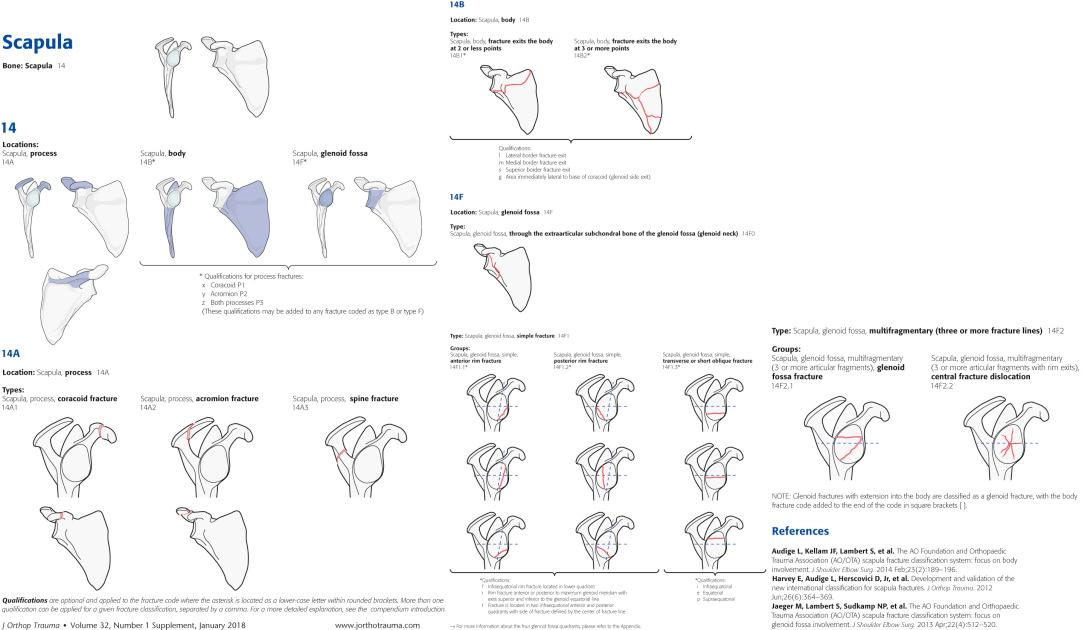
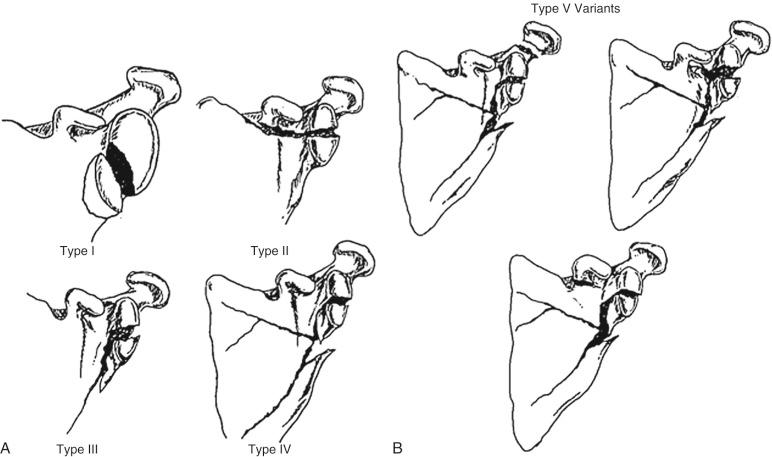
Several classifications have been developed for scapula fractures. However, the unique scapular anatomy creates a challenge in developing one classification system that is both comprehensive and prognostic. Comprehensive classifications include those of Hardegger et al., Ada and Miller, and OTA. Both Ada and Miller and Hardegger et al. are beneficial in that their subclassifications reflect patterns commonly encountered in practice. The OTA and AO Fracture and Dislocation Classification Compendium recently published an updated scapula classification, which divides the scapula into three basic segments: processes, body, and glenoid fossa. The glenoid fossa fractures are further subdivided based on the quadrant and number of fracture lines involved ( Fig. 49.8 ).
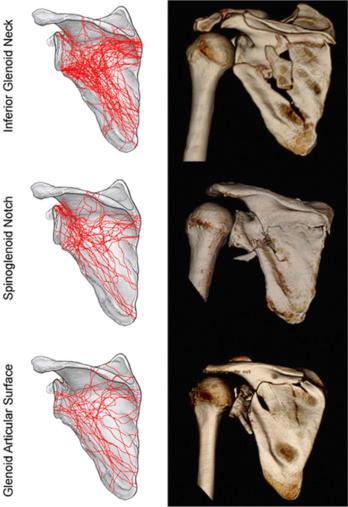
Scapula fractures have also been mapped from analysis of 3-D reconstructions to clearly illustrate the true nature of fracture patterns, and perhaps should serve as a basis for a comprehensive classification scheme ( Fig. 49.9 ).
Focused classifications exist for the glenoid, acromion, and coracoid, as well. The classification scheme developed by Mayo et al. for intraarticular fractures is a reorganized version of the Ideberg classification and was developed based on the imaging and operative findings of 27 intraarticular glenoid fractures ( Fig. 49.10 ), making it particularly useful to the surgeon.
Ogawa and colleagues proposed a classification system specific to the acromion and coracoid. Coracoid fractures were classified based on whether the fracture line runs anterior or posterior to coracoclavicular ligaments, whereas the acromion was classified based on the fracture proximity to the spinoglenoid notch. Anavian and colleagues mapped fractures of 26 operatively treated process fractures. There was a higher prevalence of coracoid base fractures that extended into the glenoid with the fracture line running posterior to the coracoclavicular ligaments (an Ogawa type I fracture) and acromion fractures that extended into the region of the spinoglenoid notch, or included the entire scapular spine (Ogawa type II fracture). Again, this specific series only included fractures displaced more than 1 cm, which was the surgical indication for the senior author.
Scapula fractures in and of themselves generally do not pose emergent threats, or conditions that warrant immediate surgical treatment, other than the occasional open fracture. Open fractures usually occur at the level of the acromion, after a direct superior blow, due to the superficial osseous structure of this area. This condition should be treated using the principles of open fracture management, and ideally stabilized with internal fixation if the treating surgeon on call is familiar with techniques to fix the acromion. Direct exposure and compression with pointed bone reduction forceps, followed by lag screw fixation perpendicular to the fracture, is advised. A neutralization minifragment 2-mm plate can also be used to augment lag fixation in this thin bone, depending on the fracture pattern and the presence of comminution. A superior-based thin plate on the tension surface to augment lag fixation is an important biomechanical principle to employ in certain variants such as for large patients or comminuted fractures ( Fig. 49.11 ).

The high-energy scapula fracture is often associated with other life-threatening injuries that do warrant emergent treatment. This fracture should serve as a harbinger of critical injuries to the cervical spine, the head, and ipsilateral chest, especially warranting careful radiographic review and a secondary survey of the patient. Have a high index of suspicion for such injuries, and review carefully the chest radiograph for multiple rib fractures and a pneumothorax, which may require chest tube placement. The orthopaedic team should be working closely with the general surgery trauma team in the management of such patients and timing of the scapula surgery if warranted ( Fig. 49.12 ).
Indications for definitive care of scapular fractures remain relative; however, there is a growing body of evidence to suggest that outcomes are good or excellent and risks of surgery are low. Several authors have suggested surgical indications based on personal experience and most report qualitative descriptions with only a few reports defining quantitative measures for operative indications.
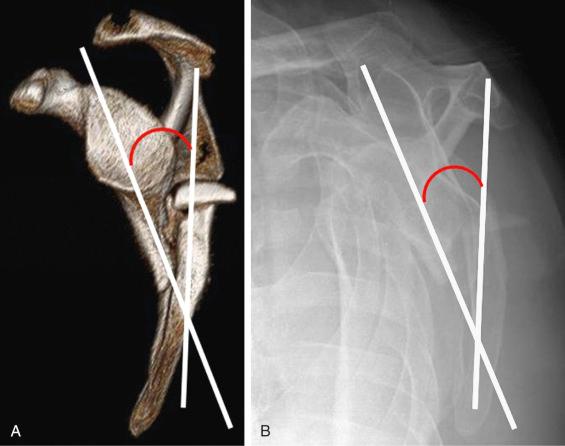
More recently, explicitly defined measures of scapula fracture characteristics have been reported and shown to be valid. Anavian et al. reported, from the study of 45 patients with scapular fractures, a detailed illustration of medialization or lateral border offset (LBO) ( Fig. 49.13 ), angulation ( Fig. 49.14 ), and glenopolar angle ( Fig. 49.15 ). This measurement technique has been validated in an interreader and intrareader reliability study.
![Fig. 49.13, Measurement of lateral border offset is performed on (A) a three-dimensional computed tomography (3-D CT) oriented in the semicoronal scapula plane (mimicking the anterior-posterior [AP] view) and (B) Grashey radiographs. The common displacement pattern is for the inferior scapula fragment to lateralize in relation to the superior fragment. The lateral border offset is measured drawing a line from the lateralmost extent of the inferior fragment and another perpendicular line from the lateralmost aspect of the superior fragment. Fig. 49.13, Measurement of lateral border offset is performed on (A) a three-dimensional computed tomography (3-D CT) oriented in the semicoronal scapula plane (mimicking the anterior-posterior [AP] view) and (B) Grashey radiographs. The common displacement pattern is for the inferior scapula fragment to lateralize in relation to the superior fragment. The lateral border offset is measured drawing a line from the lateralmost extent of the inferior fragment and another perpendicular line from the lateralmost aspect of the superior fragment.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/ScapulaFractures/12_3s20B9780323611145000495.jpg)
![Fig. 49.15, Measurement of glenopolar angle is performed on (A) a three-dimensional computed tomography (3-D CT) oriented in the coronal scapula plane (mimicking the anterior-posterior [AP] view) and (B) Grashey radiographs. The glenopolar angle measurement is made by drawing a line from the inferior to the superior pole of the glenoid fossa and another line from the superior pole to the apex of the scapula body's inferior angle. Fig. 49.15, Measurement of glenopolar angle is performed on (A) a three-dimensional computed tomography (3-D CT) oriented in the coronal scapula plane (mimicking the anterior-posterior [AP] view) and (B) Grashey radiographs. The glenopolar angle measurement is made by drawing a line from the inferior to the superior pole of the glenoid fossa and another line from the superior pole to the apex of the scapula body's inferior angle.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/ScapulaFractures/14_3s20B9780323611145000495.jpg)
Authors such as Hardegger et al., Ada and Miller, Nordqvist and Petersson, and Romero et al. clearly influence and inform the surgical indications that have evolved into contemporary literature. Findings from these authors indicated a clear relationship in patients with the most severe injuries resulting in persistent shoulder disability and residual deformity, seen radiographically. These patients have been shown to be most likely to have functional complaints and pain after nonsurgical treatment.
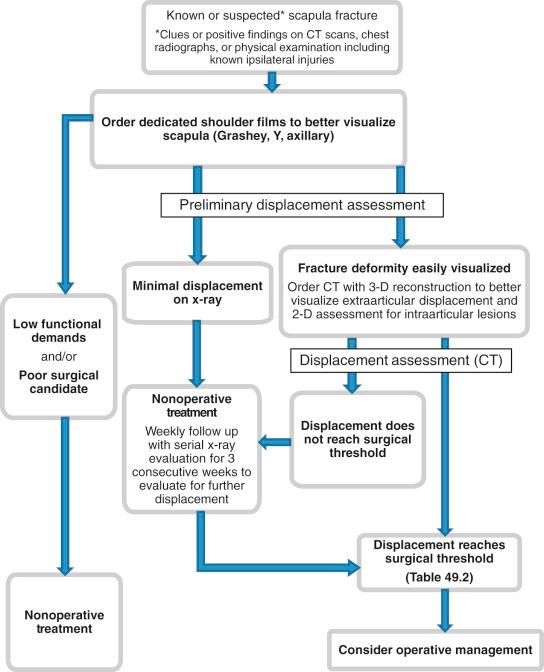
Defined surgical indications gleaned from the literature can be categorized by injury type. Several authors have used nonspecific terms of “displaced” or “unstable,” and a select few have proposed measured radiographic guidelines ( Fig. 49.16 and Table 49.1 ; see Figs. 49.13 to 49.15 ). The senior author's preferred guidelines for surgical indications are summarized in Table 49.2 .
| Threshold | ||
|---|---|---|
| Articular step-off/gap | Kavanagh BF et al. (1993) | >2 mm |
| Mayo KA et al. (1998) | >5 mm | |
| Herrera DA et al. (2009) | ≥4 mm | |
| Jones CB et al. (2009) | >3 mm | |
| Jones CB et al. (2011) | >3 mm | |
| Anavian J et al. (2012) | ≥4 mm | |
| Lateral border offset | Ada JR and Miller ME (1991) | ≥10 mm |
| Herrera DA et al. (2009) | ≥15 mm | |
| Jones CB et al. (2009) | ≥20 mm | |
| Jones CB et al. (2011) | ≥20 mm | |
| Gauger EM et al. (2012) | ≥20 mm | |
| Cole PA et al. (2012) | ≥20 mm | |
| Angulation | Ada JR and Miller ME (1991) | ≥40 degrees |
| Herrera DA et al. (2009) | ≥25 degrees | |
| Jones CB et al. (2009) | ≥45 degrees | |
| Jones CB et al. (2011) | ≥45 degrees | |
| Bartoníček J and Fric V (2011) | ≥30 degrees | |
| Cole PA et al. (2012) | ≥45 degrees | |
| Gauger EM et al. (2012) | ≥45 degrees | |
| Glenopolar angle | Labler L et al. (2004) | ≤30 degrees |
| Izadpanah K et al. (2011) | ≤30 degrees | |
| Cole PA et al. (2012) | ≤22 degrees | |
| Gauger EM et al. (2012) | ≤22 degrees | |
| Intraarticular fractures | ≥4 mm step or gap |
| Open fracture | |
| Symptomatic malunion and nonunion | |
| Extraarticular fractures | ≥20 mm lateral border offset (LBO) |
| ≤22 degrees' glenopolar angle (GPA) | |
| ≥45 degrees' angulation | |
| Combination of ≥30 degrees' angulation and ≥15 mm and LBO | |
| Double disruption to the superior shoulder suspensory complex (SSSC) with ≥10 mm at both lesions | |
| Open fracture | |
| Symptomatic malunion or nonunion | |
| Process fractures | ≥10 mm displacement |
| Acromial depression | |
| Open fracture | |
| Symptomatic malunion or nonunion |
For extraarticular scapular fractures with or without concomitant ipsilateral shoulder girdle fractures, four articles, beginning with Ada and Miller in 1991, have proposed medial displacement or LBO of greater than 1 cm to greater than 2.5 cm as one indication for surgery. These same authors state that angular deformity of greater than 25 to greater than 45 degrees would also be an indication for operative treatment, as well as combined injuries with intraarticular involvement, or multiple disruptions of the superior shoulder suspensory complex (SSSC) ( Fig. 49.17 ).
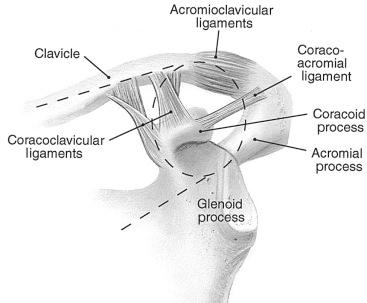
Goss first described the concept of the SSSC to characterize the osseoligamentous ring that includes the glenoid, coracoid, clavicle, and acromion process along with the connecting soft tissues between these structures (i.e., coracoclavicular ligament and AC joint capsule). Goss taught that the interruption of two structures within this ring constitutes a “double disruption of the SSSC” that resulted in a disruption of the suspension system between the axial and appendicular skeleton.
Three-dimensional CT has been advocated for the accurate visualization of these severe injuries. If operative indications are suspected based on the two-dimensional radiographic images, by obtaining 3-D CT reconstructions, a full and accurate assessment of LBO, angular deformity, and glenopolar angular deformity can be quantitatively measured. As well, the 3-D CT reconstruction allows the surgeon to more fully understand the deforming forces acting on the fractured scapula and therefore plan the necessary operative reduction maneuvers required to reduce the fracture fragments.
There are reports of satisfactory outcomes for nonoperatively treated scapular fractures in the literature. Though some authors used only subjective surgeon assessments for determination of “good” outcomes, others made conclusions based on the scoring systems of Rowe or Constant and Murley. However, it is impossible to discern from these reports the severity of injury because no discrete radiographic measures indicating degree of displacement are used. As with principles of fracture treatment in most other areas of the anatomy, minimally to moderately displaced, stable extraarticular fractures should be treated nonoperatively with a sling for 2 to 3 weeks until fracture consolidation and pain subsidence occur.
It is notable that patients often experience pseudoparalysis during early stages of healing and many times report altered or lack of function of the injured shoulder. Secondarily, certain injury patterns may be prone to progressive deformity in the early postinjury period ( Fig. 49.18 ). In a report from our center, 8 of 49 (16%) consecutive extraarticular scapular fracture patients were treated initially without surgery but found to have increasing deformity. For this reason, serial radiographs should be obtained on a weekly basis for up to 3 weeks after injury. Though not established through biomechanical or kinematic study, we hypothesize that the possibility for increasing deformity occurs through fracture instability, muscular spasm, and gravitational forces when patients are upright and mobile. Likely, scapular fractures associated with multiple consecutive rib fractures or double lesions of the SSSC are most at risk, due to the compromised thoracic and appendicular skeletal support, though this hypothesis has not been tested.
Due to the lack of randomized coltrolled trials in the literature on this topic, there are conflicting opinions and only level IV evidence of therapeutic outcomes to advise surgical indications. In our center, nonoperative treatment is reserved for those patients with less than 20 mm of LBO (or medialization) or less than 40 degrees of angular deformity of the body or neck on a scapula Y view. In the presence of clinical healing and pain subsidence, management with a sling and progressive physical therapy generally provides good results in these patients.
Once the decision has been made to operate, it is vital to choose the best approach to most effectively accomplish reduction and fixation with the least amount of trauma to the soft tissues. These principles will promote the fastest rehabilitation and allow for the most complete recovery.
Any isolated anterior glenoid or coracoid fracture should be operated through the deltopectoral interval, unless small enough to treat arthroscopically, as in small bony Bankart lesions more common to sports-related mechanisms. Sometimes the isolated glenoid fractures are more inferior fragments, and the surgeon must determine whether an anterior or posterior approach offers best access. A 3-D CT reconstruction can help to visualize where the apex of the fracture is in these variants. An isolated coracoid fracture can be accessed through a 4- to 6-cm incision centered over the coracoid itself. There is a common superior glenoid fracture variant (Ideberg type III), which often extends just inferior to the coracoid, and this fracture is best accessed through a deltopectoral approach if the surgeon desires to visualize the articular surface ( Fig. 49.19 ). Furthermore, this variant requires intraarticular exposure when the patient is delayed to treatment because of the need to clean out the fracture and remove callus, which needs to be done from the intraarticular vantage point.

Other considerations that influence the anterior surgical approach is whether or not there is an associated AC dislocation or clavicle fracture. The incision is modified and extended as necessary to accommodate fixation of these entities when present. For example, an incision over the AC joint can be extended caudal and anterior over the coracoid and down the deltopectoral interval, or an anterior incision to address a clavicle fracture can be extended distal and caudad over the coracoid and down the deltopectoral interval ( Fig. 49.20 ). These injury combinations are not uncommon and must be considered.
When operating on a displaced scapula fracture involving the scapula neck or body, a posterior approach is almost always favored, whether or not the articular surface is involved. The variations of the posterior approach then depend on the pattern and chronicity of the fracture, in addition to whether intraarticular inspection and access are necessary. These variations will be described in the following section.
Occasionally in severe associated scapula fractures, combined anterior and posterior approaches are necessary. This situation occurs when there is an associated scapula body and/or neck fracture, with extensive comminution of the glenoid and/or a coracoid fracture. In such circumstances, our preference is to start with the posterior approach to restore the proper rotation and relationship of the body and neck and posterior glenoid surface, and then proceed to an anterior approach to restore stability to the coracoid or anterior glenoid, now with a stable neck to which the surgeon can build ( Fig. 49.21 ).
Arthroscopic techniques have emerged for fixation of isolated glenoid fractures. Injuries most amenable to such techniques represent the Bankart lesion and generally involve unstable, younger patients with a minimal portion of the articular surface involved. Potential benefits to arthroscopic treatment are that the surgeon has direct articular surface visualization and the ability to assess labral and capsular integrity. These methods are best reserved for fractures managed within 2 weeks of injury. Screws and suture anchors are reported methods for fixation.
The scapula is part of the superior shoulder suspensory mechanism, which attaches the upper extremity to the axial skeleton by the clavicle. Eighteen muscular origins and insertions on the scapula aid in its function to provide a stable base from which glenohumeral mobility can occur. It is important to understand the deforming vectors for these muscles, which will aid in the interpretation of reduction techniques.
The scapula is a relatively flat and triangular bone, with a thin body surrounded by a well-developed periphery, which are the key opportunities for plate and screw fixation. Deforming forces from muscle insertions determine displacement of the individual fragments ( Fig. 49.22 ), with the common superior fragment often medialized and rotated caudal, whereas the inferior body lateralizes. The scapular spine divides the cephalad supraspinatus from the posterior infraspinatus fossa, which are origins for their respectively named muscles. The concave anterior body surface of the scapula serves as the origin for the subscapularis muscle, which provides a robust blood supply to operated fragments even when elevating the entire rotator cuff from the infraspinatus fossa.
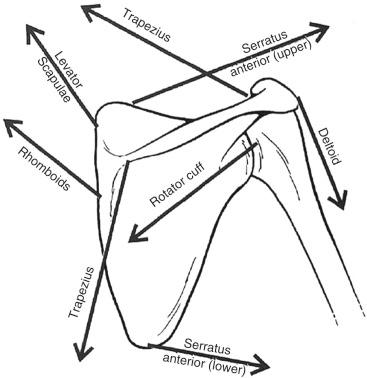
The acromion is the prominent, lateral, cephalad structure at the distal end of the scapular spine. The acromion and clavicle serve as the origin for the deltoid muscle, which requires detachment during certain approaches to the acromion or posterior scapula as described shortly. The trapezius also originates on the acromion and scapular spine anteriorly. The anterior medial border of the scapula is the site of attachment of the serratus anterior, the main scapula protractor, and the rhomboid muscles inserting posterior medial, which function as scapula retractors. The levator scapulae muscle inserts on the superior medial border and is specifically named for its function. It is responsible partially for the inferior tilt of the fractured superior fragment commonly seen in fractures, manifesting in the decreased glenopolar angle measured radiographically.
The lateral border of the scapula sweeps up from the inferior angle, forming a thick condensation of bone that ends in the neck of the scapula. The lateral border, sometimes referred to as the pillar of the scapula, is the site of origin of the teres major and minor muscles, as well as the insertion for the long head of the triceps on the neck, and it provides the most important osseous fixation points for rendering fracture stability. The latissimus dorsi inserts at the inferior angle and its contractile forces are responsible for this largest region of the scapular body.
The coracoid process is the long, curved osseous projection medial to the anterior neck of the scapula, which serves as the origin for the coracoacromial and coracocalvicular ligaments, as well as for the coracobrachialis, short head of the biceps, and pectoralis minor muscles. Just medial to the coracoid process on the superior margin of the scapula is the scapular incisura, traversed by the transverse scapular ligament, above which runs the suprascapular artery and below which lays the suprascapular nerve.
The glenoid fossa has a fibrocartilaginous peripheral labrum that is confluent with the long head of the biceps tendon at the supraglenoid tubercle. The labrum increases the depth of the glenoid by 50%. The glenoid fossa is approximately 39 mm in a superior-inferior direction and 29 mm in an anterior-posterior direction in its lower half, which is 20% wider than the top half.
The patient is placed in a beach chair position with an arm board attached to support the extremity. Place the arm board sufficiently distal so as to be out of the way of shoulder fluoroscopy, and a table with a shoulder “cut-out” is very useful to facilitate imaging as well. A radiograph plate may be positioned before draping posterior to the shoulder for an intraoperative film, but it is helpful in complex glenoid fracture variants to have the use of an intraoperative C-arm during the procedure to evaluate fracture reduction and ensure there is no intraarticular penetration by hardware.
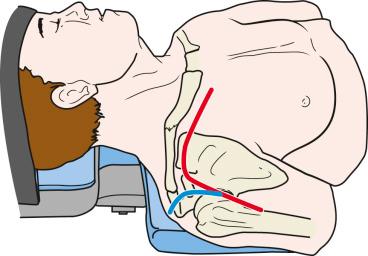
The patient is placed in the lateral decubitus position, falling slightly forward for access to the posterior shoulder. An axillary roll is positioned to protect the brachial plexus. Arm rests, towels, or blankets can be used to support the upper extremities, but specially designed positioning bumps (BoneFoam Inc., Cocran, MN) are optimal to support the extremity in 90 degrees of forward flexion and slight abduction ( Fig. 49.23 ). The entire upper extremity and forequarter should be prepped and draped to allow for manipulation of the shoulder after fixation. The prep should include the patient's neck superiorly, the vertebral column medially, and the latissimus fold caudally to ensure maximal exposure and orientation.

Many surgical approaches and variations on those approaches are used for different scapula fracture patterns and associated injuries to the clavicle and scapular processes. These are discussed in this section, but Table 49.3 serves as a guide to the more commonly encountered fractures. Though different possible approach options are noted, the author's preferred method is detailed to assist with this decision making. As there are many nuances in this decision-making process, Table 49.3 should only serve as a guideline.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here