Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
See Chapter 21 Scapholunate Ligament Repair.
This chapter reviews reconstruction options for stage III and IV scapholunate ligament injuries. Unlike stage I and II injuries, the ligament is not repairable because of poor tissue quality, and thus reconstruction should be attempted.
As discussed in Chapter 21 , stage I and II injuries still have good ligament quality after partial or complete injury. Therefore repair should be attempted.
For stage V and VI injuries, where either irreducible malalignment of the carpus (stage V) or cartilage loss with arthritis is present (stage VI), salvage procedures should be pursued ( Chapter 27 Salvage Procedures for Scaphoid Nonunion). Options include proximal row carpectomy, four-corner fusion, or wrist arthrodesis ( Chapter 53 Total Wrist Fusion).
See Chapter 21 .
See Chapter 21 .
See Chapter 21 .
See Chapter 21 .
One indication is dynamic scapholunate dissociation in which the ligament cannot be repaired primarily.
Bone-tissue-bone (BTB) reconstruction can be performed for static, reducible instability through a ligament reconstruction; a three or four ligament tenodesis should be considered.
BTB reconstruction is contraindicated where there is evidence of radiocarpal or midcarpal arthritis.
Standard posteroanterior (PA), oblique, and lateral wrist radiographs will not show scapholunate (SL) widening with dynamic SL instability.
Clenched-fist views, when the wrist is loaded, will reveal gapping between the scaphoid and lunate if the ligamentous injury is significant.
Arthroscopy can be performed to confirm the diagnosis and to rule out articular wear that would preclude reconstruction in favor of a salvage operation, such as wrist fusion.
The dorsal SL ligament is the strongest portion of the U-shaped ligament that also has a proximal and volar component.
Repair or reconstruction of the dorsal portion of the ligament is desired.
Scaphoid stabilization with extensor carpi radialis longus (ECRL) tenodesis is also an option for this stage of injury and may be more predictable.
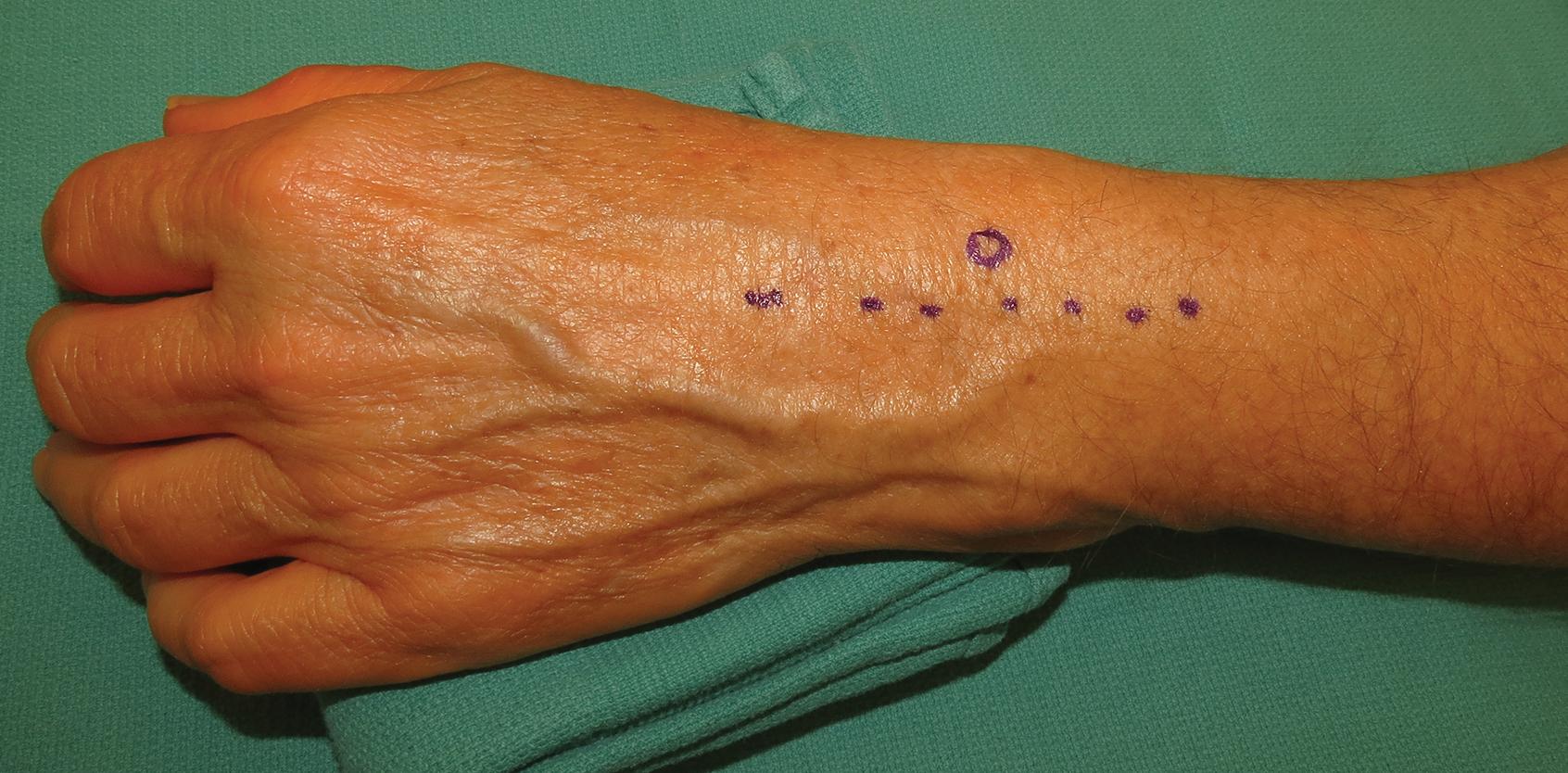
A 6-cm longitudinal incision is designed on the dorsal wrist, ulnar to the Lister tubercle ( Fig. 22.1 ).
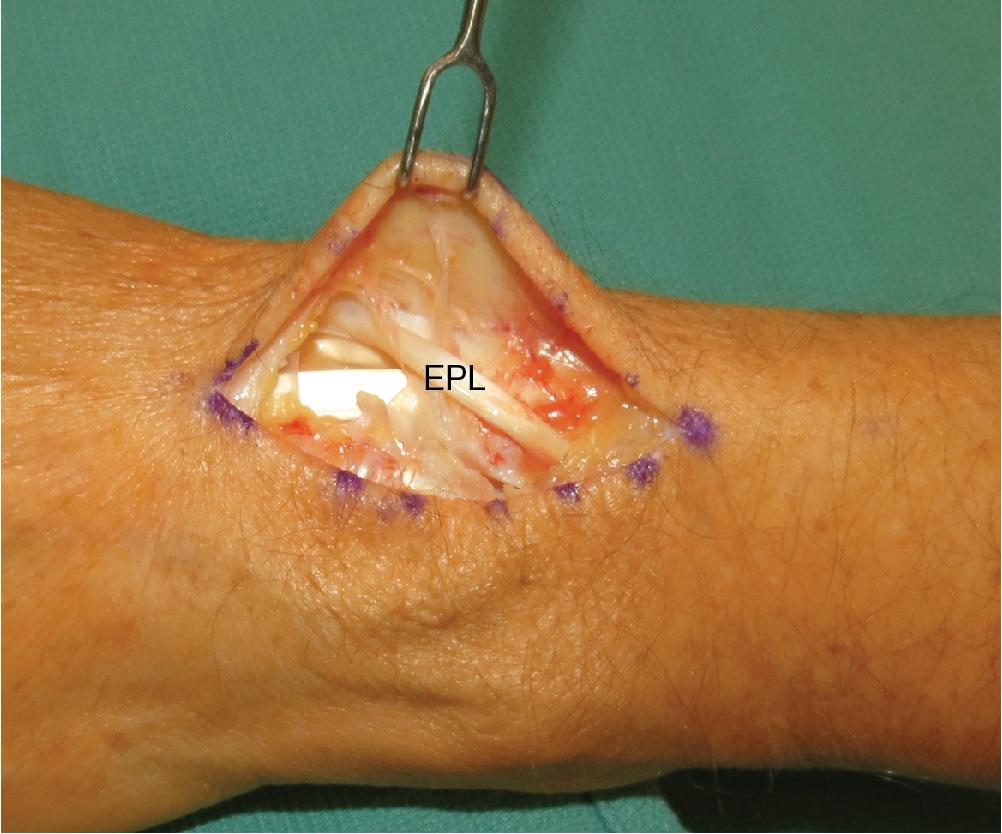
After incising the extensor retinaculum between the third and fourth compartments, the extensor pollicis longus (EPL) is identified and retracted radially ( Fig. 22.2 ).
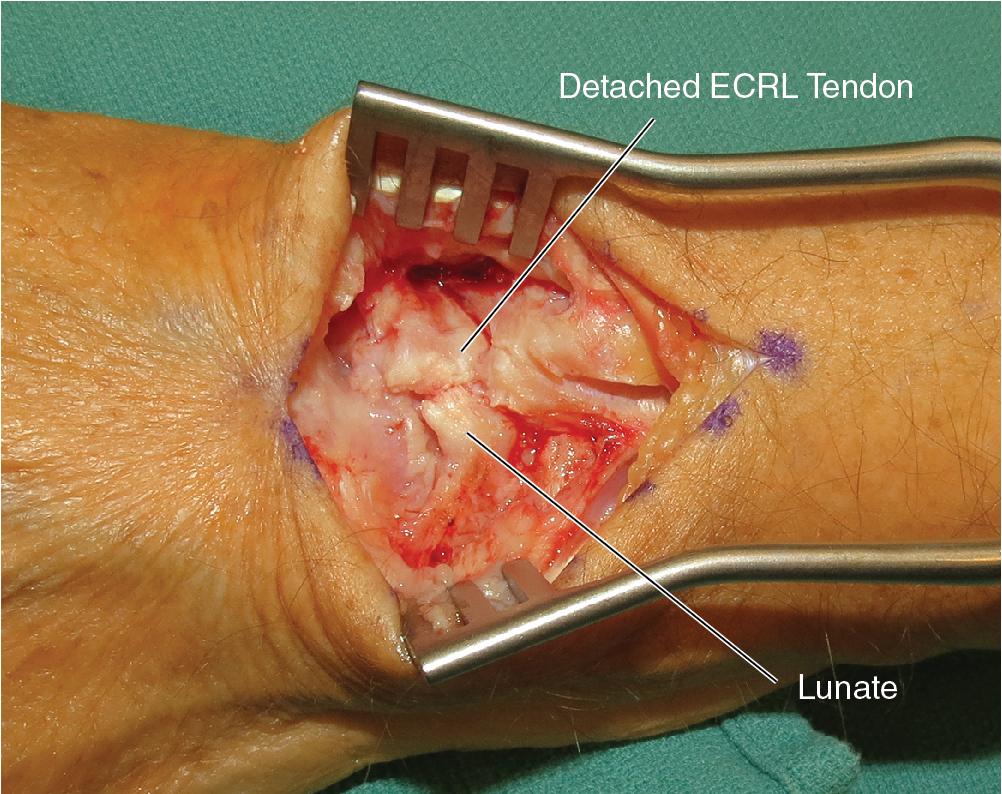
The wrist capsule is opened longitudinally to expose the SL interval.
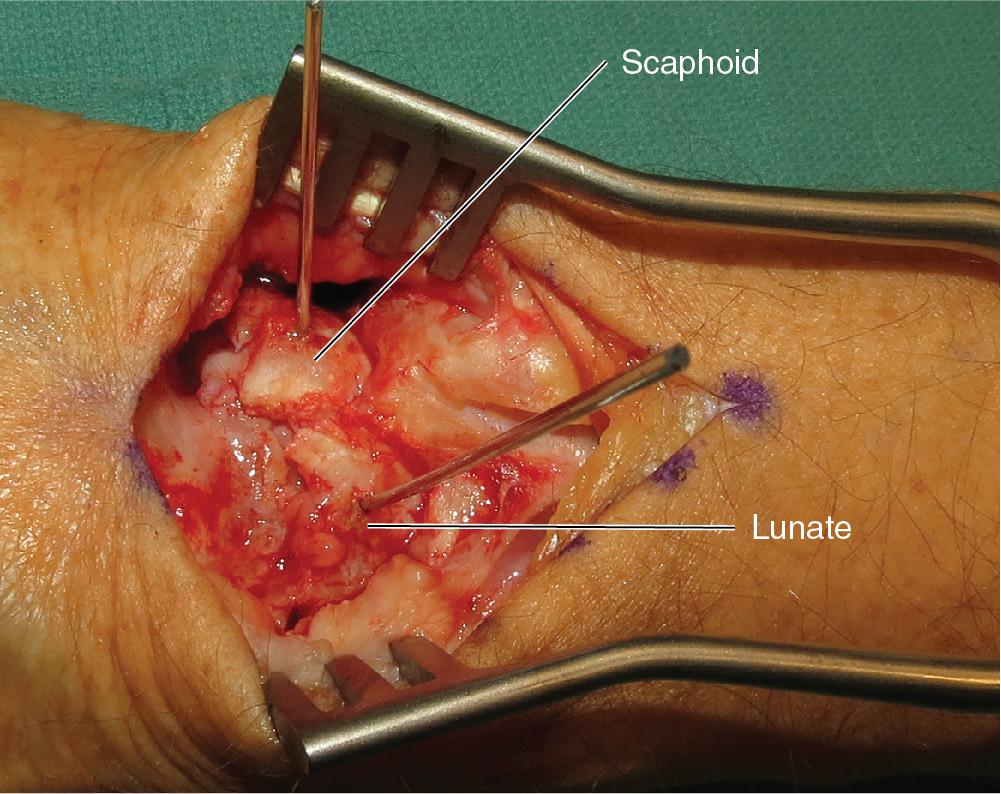
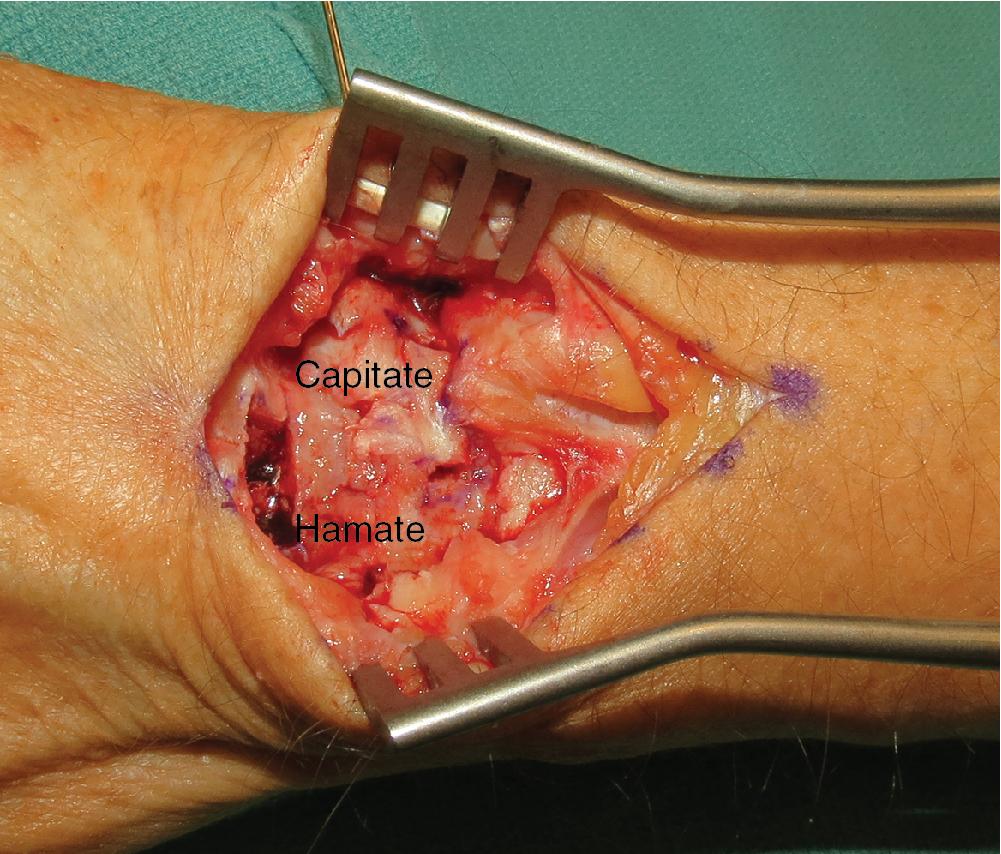
After exposing the SL interval, scar tissue should be debrided back to healthy bleeding tissue ( Fig. 22.3 ).
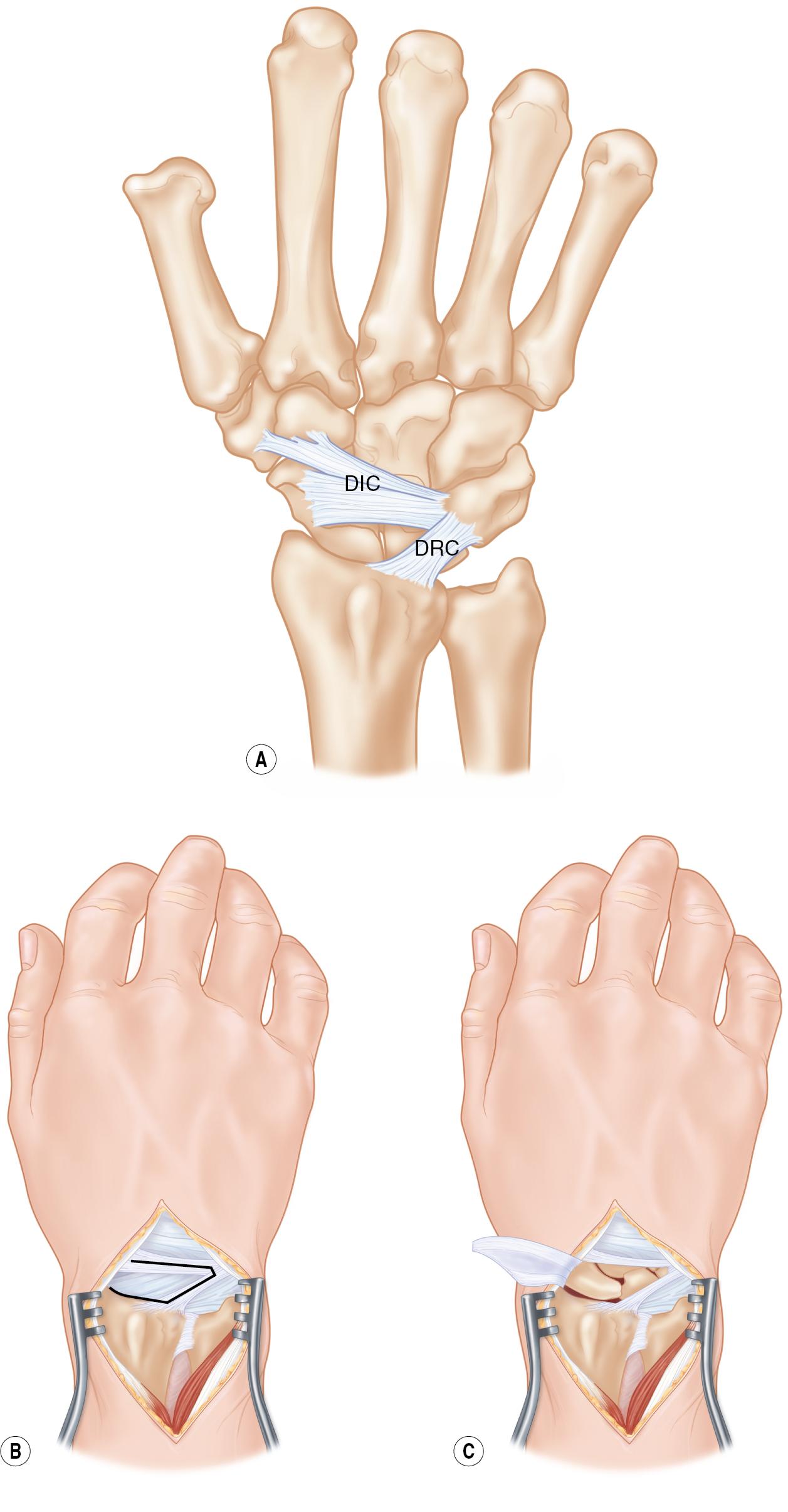
A ligament-sparing approach to the wrist can be performed. The design of this radially based triangular flap splits the fibers of the dorsal radiocarpal and dorsal intercarpal ligaments ( Fig. 22.4A–C ).
If static, reducible instability is present, the scaphoid will need to be anatomically reduced to correct any dorsal intercalated segment instability (DISI) deformity.
Two 0.062-in (1.57-mm) Kirschner wires (K-wires) can be used to reduce the scaphoid and lunate into preinjury anatomic alignment ( Fig. 22.5 ).
Because the scaphoid is flexed and the lunate is extended with a DISI deformity, the K-wires should be placed from distal to proximal in the scaphoid and proximal to distal in the lunate.
Using the K-wire, the lunate should be flexed maximally toward the fingers to ensure that it is neutral with respect to the long axis of the radius.
The scaphoid can be extended to ensure that the flexed, pronated posture is corrected ( Fig. 22.6 ).
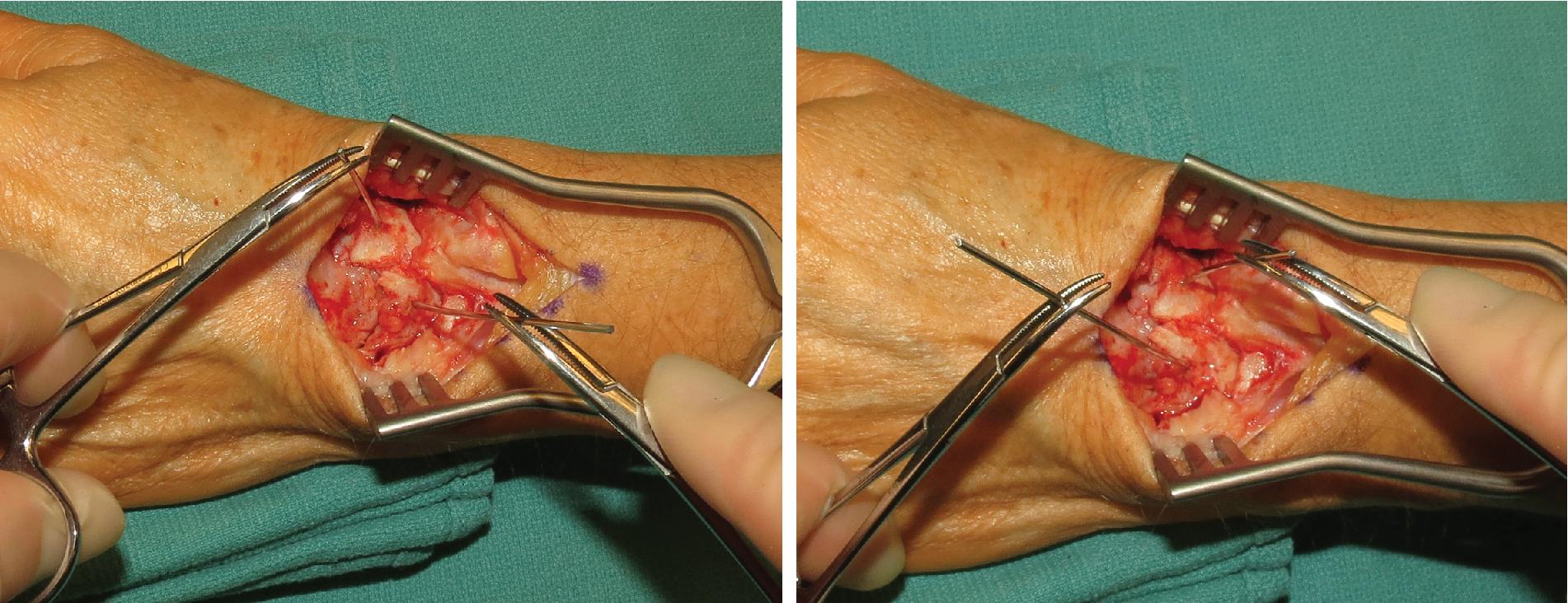
To close the gap between the two bones, the wires are compressed.
Because the scaphoid has assumed a flexed position and the lunate is extended, the wires should be placed from distal to proximal in the scaphoid and proximal to distal in the lunate. This will facilitate reduction.
Stouter 0.062-in (1.57-mm) K-wires are used instead of 0.045-in (1.14-mm) wires.
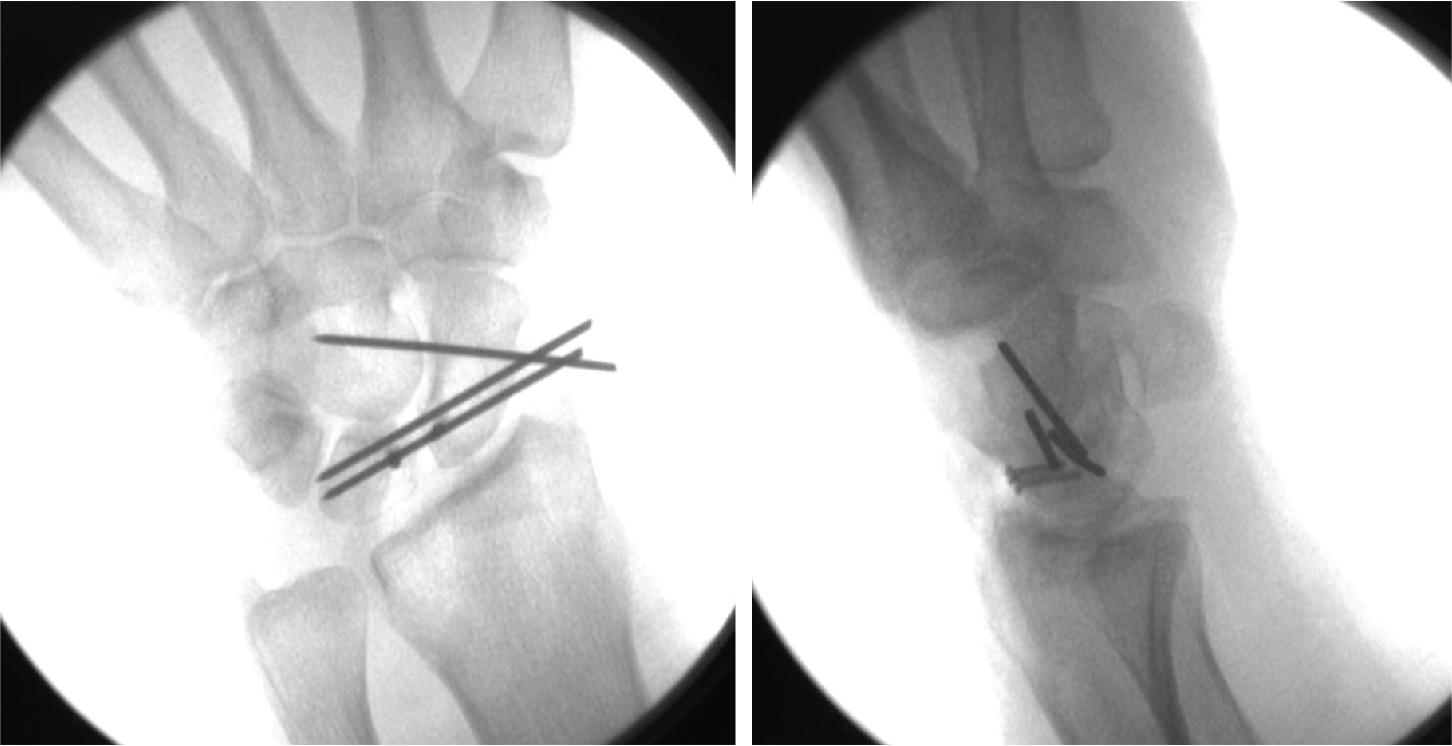
Reduction is maintained by pinning the scapholunate interval. This can be achieved with one 0.062-in (1.57-mm) K-wire. The entry point for the K-wire is just distal to the radial styloid. The wire should be directed perpendicular to the long axis of the forearm to capture the scaphoid and lunate. Reduction of the scapholunate gap and restoration of the normal scapholunate angle (30–60 degrees) should be confirmed fluoroscopically.
A second 0.062-in (1.57-mm) K-wire can be driven across the scaphocapitate (SC) interval to prevent midcarpal motion ( Fig. 22.7 ).

The SL angle should be corrected and confirmed radiographically: normal scapholunate angle is 30–60 degrees and normal radiolunate angle is 0–15 degrees.
Gapping between the scaphoid and lunate should be eliminated.
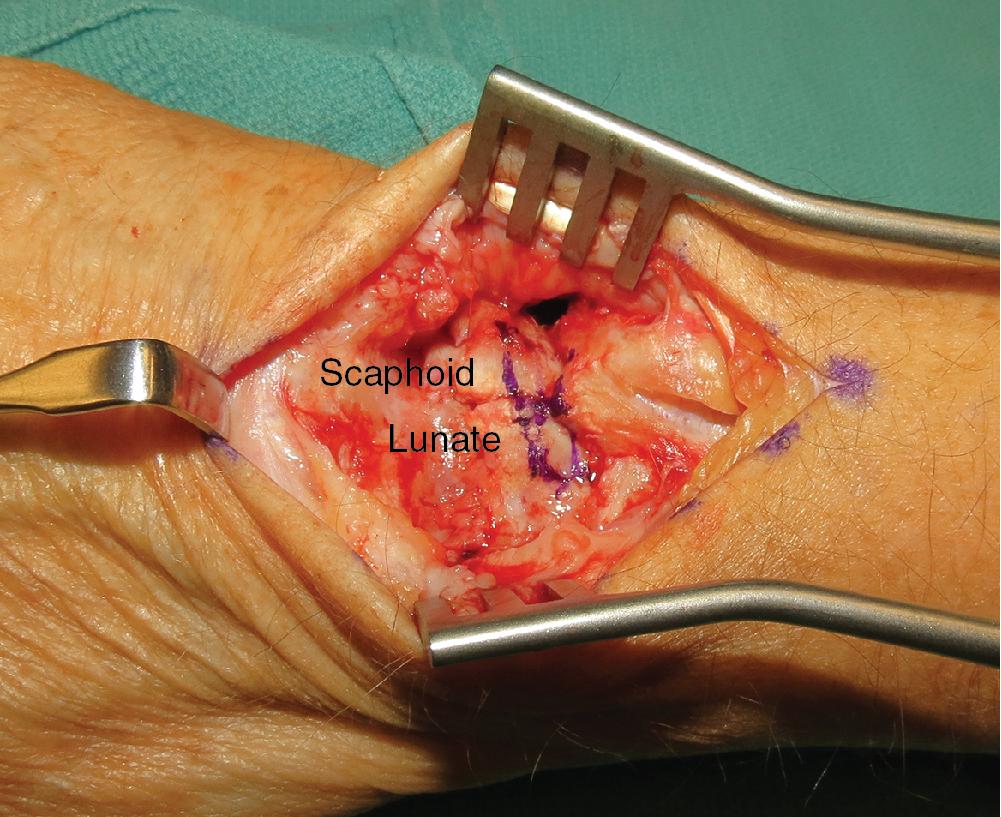
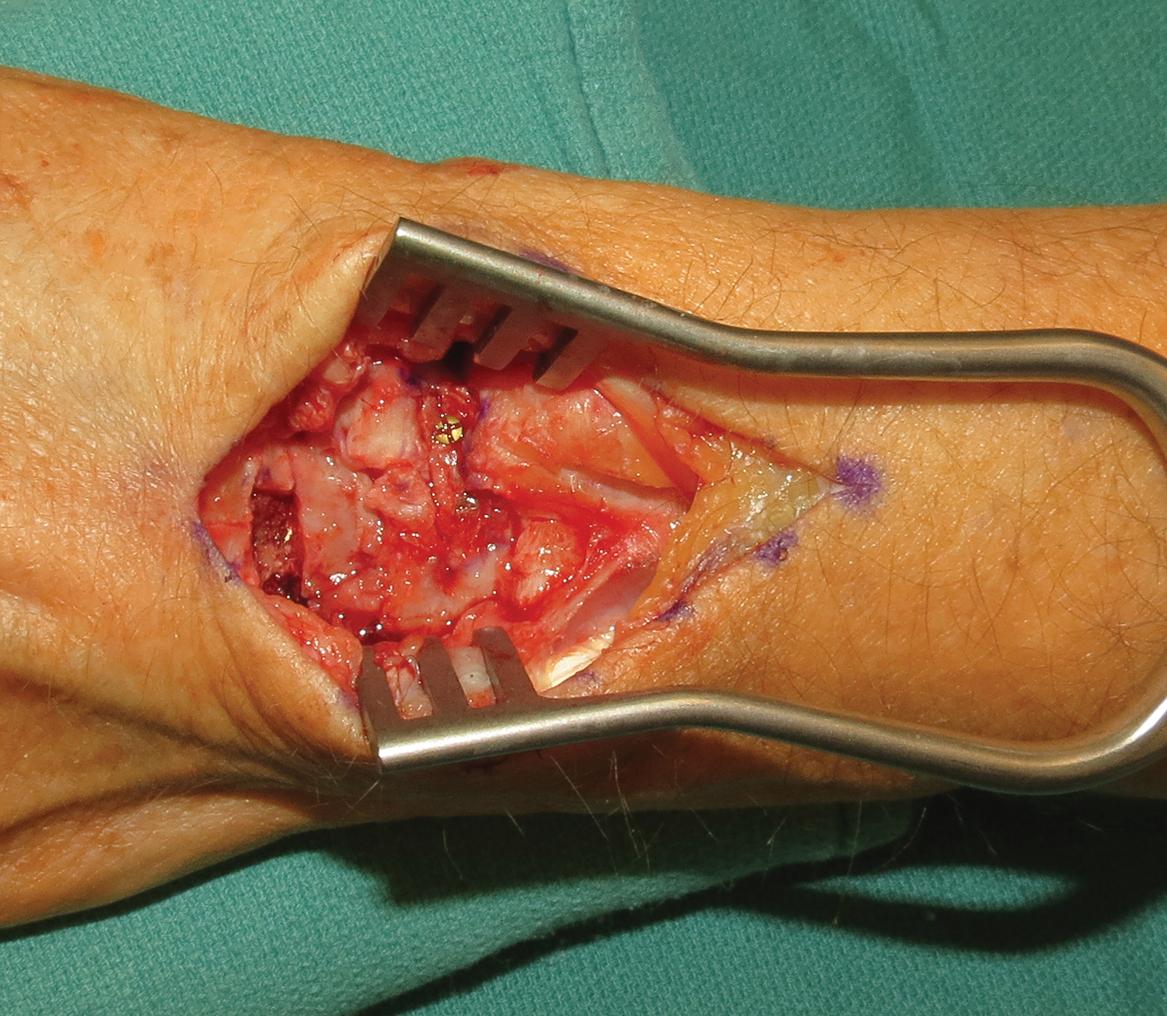
Using a 5-mm osteotome, create a trough on the dorsal surface of the scaphoid and lunate to accept the BTB graft.
The dimensions of this trough measured 12 mm long, 6 mm wide, and 6 mm deep ( Fig. 22.8 ).
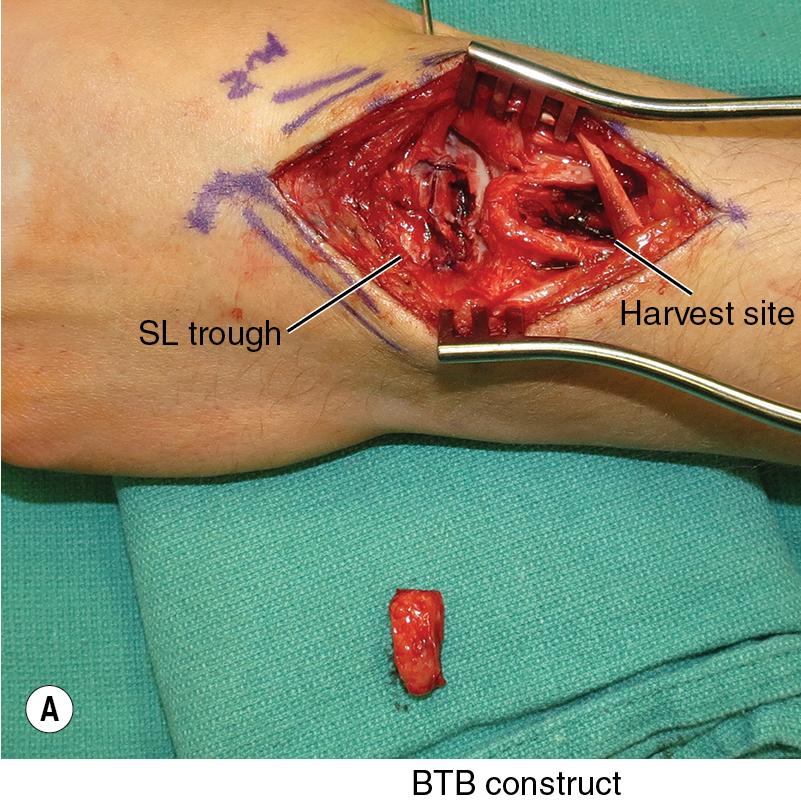
After measuring the defect created in the dorsum of the scaphoid and lunate, transpose this template onto the capitohamate ( Fig. 22.9A–B ).
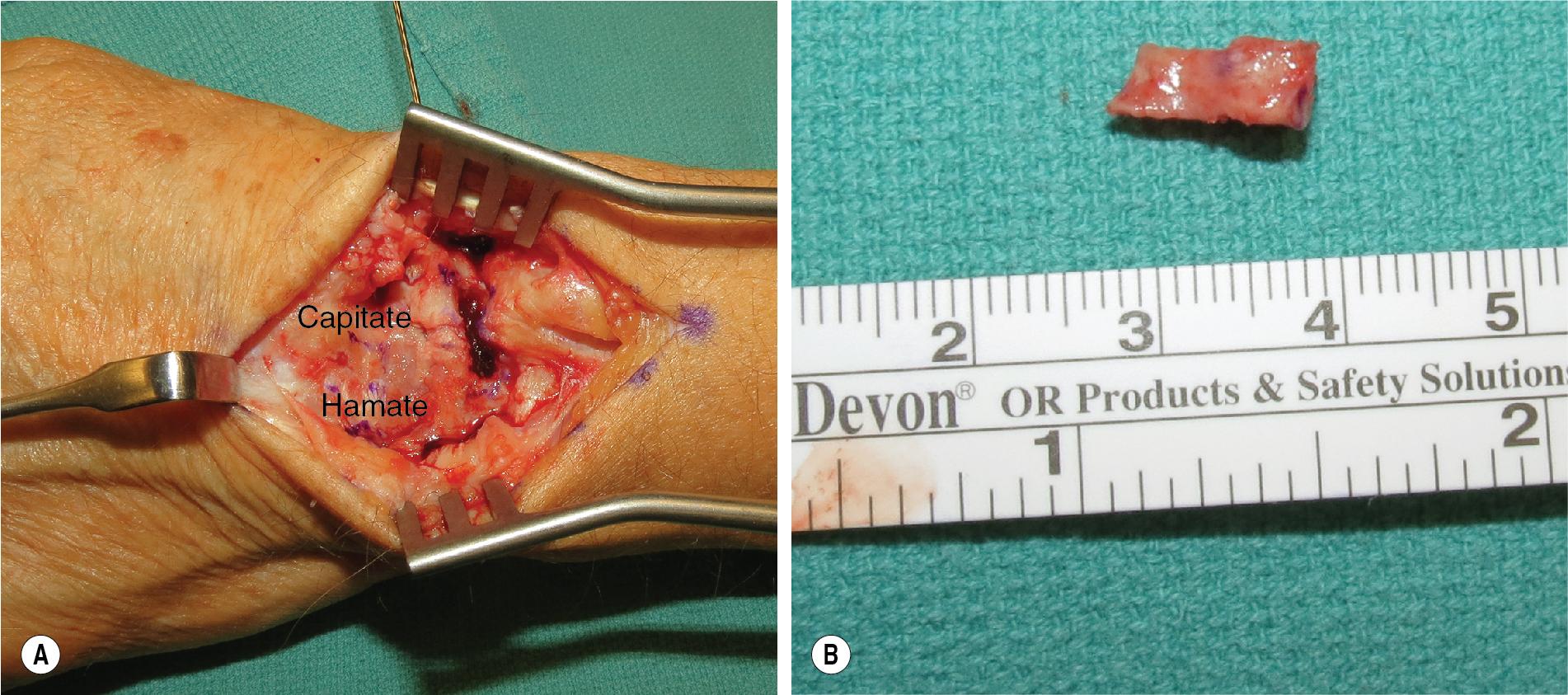
Using the 5-mm osteotome, harvest the BTB graft ( Fig. 22.10 ).
When harvesting the graft, it is important to center your template over the capitohamate ligament and preserve this attachment to both the capitate and hamate.
Alternatively, you can harvest BTB from the distal radius over the Lister tubercle ( Fig. 22.11 ); however, the capitohamate ligament is more accessible because it is at the same operative field, just distal to the SL interval. It is important to remove a segment of bone from this BTB graft ( Fig. 22.12 ). The goal is to reconstruct the dorsal ligament and avoid bony fusion between the scaphoid and lunate.

After contouring and placing the graft in the trough on the dorsum of the scaphoid and lunate, 1.3-mm or 1.5-mm screws can be placed through each side of the graft into the corresponding carpal bone ( Fig. 22.13 ). Alternatively, if precise measurements are obtained, then the graft can be press fit into the trough by gently tapping the bone grafts into the slot with a bone tamp.
The K-wire should be buried and left in place to maintain reduction of the SL interval ( Fig. 22.14 ).
After the tourniquet is deflated and hemostasis is ensured, the dorsal capsule and extensor retinaculum can be closed using 3-0 or 4-0 Vicryl suture.
The skin can be closed using 4-0 Monocryl or 4-0 PDS.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here