Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Bladder pain syndrome/interstitial cystitis (BPS/IC) is a severely debilitating chronic disorder characterized by pain perceived to arise from the bladder, exacerbated by bladder filling, and associated with urinary urgency or frequency. The condition has been known to physicians since the early 19th century when Joseph Parrish first published his report of three patients with severe lower urinary tract symptoms and labeled the condition “tic doloureux,” presumed at that time to be a neuralgia of the bladder ( ). However, to this day its etiology still remains unknown, there are no pathognomonic clinical or pathological features, and its treatment remains elusive. Importantly, it is a diagnosis of exclusion that can only be made after other pathologies of the bladder, urethra, and other pelvic organs have been ruled out.
Nomenclature for this condition has undergone a number of changes over the past century, with the term IC (to describe a true inflammatory, end-organ, bladder disorder) being increasingly replaced by the preferred term BPS (a primary pain syndrome with symptoms of chronic pelvic pain, pressure, or discomfort, perceived to be related to the urinary bladder and accompanied by at least one other urinary symptom such as persistent urge to void or urinary frequency) ( ). This change in the way the disease is now conceptualized is summarized in Fig. 123.1 .
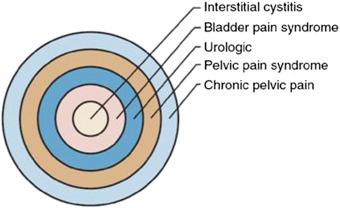
There may be many causes of chronic pelvic pain, arising from any of the intrapelvic organs. When a cause cannot be found, it is referred to as a pelvic pain syndrome, or it can be subdivided, based on the system of origin, if known (e.g., urological, gynecological, colorectal). Urological causes can be subdivided, based on the likely organ of origin (e.g., bladder, prostate, testicle). BPS can be further classified according to the ESSIC criteria ( Table 123.1 ). This system classifies patients into groups, depending upon findings at cystoscopy (normal bladder, presence of glomerulations, or presence of Hunner’s ulcers) and histological features on bladder biopsy (normal, inconclusive, positive histology showing inflammatory infiltrates and/or detrusor mastocytosis and/or granulation tissue and/or intrafascicular fibrosis). It is now clear that BPS is a large symptom syndrome, consisting of diverse phenotypes (such as those with classic Hunner’s ulcers, 1
1 Hunner’s ulcers, also called “Hunner’s lesions” or “Hunner’s patches,” are a subtype of interstitial cystitis (also called IC) and are not ulcers in the usual sense. They are distinctive areas of inflammation on the bladder wall that characterize the “classic” form of IC. Taken from the internet at http://www.ichelp.org/about-ic/symptoms-of-ic/hunners-ulcers/ .
i.e., International Society for the Study of BPS [ESSIC] 3 and those without) and accurate phenotyping is essential to direct optimal treatment.
| Cystoscopy With Hydrodistension | ||||
|---|---|---|---|---|
| Biopsy | Not Done | Normal | Glomerulations | Hunner Lesion |
| Not done | XX | 1X | 2X | 3X |
| Normal | XA | 1A | 2A | 3A |
| Inconclusive | XB | 1B | 2B | 3B |
| Positive | XC | 1C | 2C | 3C |
Over the past 30 years, a number of different organizations have attempted to standardize the definition of this heterogeneous condition for research purposes, so that individual data points (patients) and larger data sets (populations) from different countries could be compared ( Table 123.2 ). Although there is no global consensus on nomenclature, all definitions require a combination of pain and urinary symptoms in the absence of other pathology.
| International Association for the Study of Pain (IASP) | Bladder pain syndrome (BPS) is the occurrence of persistent or recurrent pain, perceived in the urinary bladder region and accompanied by at least one other symptom, such as pain worsening with bladder filling and daytime and/or nighttime urinary frequency. There is no proven infection or other obvious local pathology. BPS is often associated with negative cognitive, behavioral, sexual, or emotional consequences as well as with symptoms suggestive of lower urinary tract and sexual dysfunction. |
| International Society for the Study of BPS (ESSIC; 2008) ( ) | Chronic pelvic pain, pressure or discomfort of greater than six months duration, perceived to be related to the urinary bladder and accompanied by at least one other urinary symptom like persistent urge to void or urinary frequency. Confusable diseases as the cause of the symptoms must be excluded. |
| American Urological Association (AUA; 2011) ( ) | An unpleasant sensation (pain, pressure, discomfort), perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes. |
| European Association of Urology (EAU; 2016) ( ) | Persistent or recurrent pain, perceived in the urinary bladder region and accompanied by at least one other symptom, such as pain worsening with bladder filling and day-time and/or night-time urinary frequency. There is no proven infection or other obvious local pathology. BPS is often associated with negative cognitive, behavioral, sexual, or emotional consequences, as well as with symptoms suggestive of lower urinary tract and sexual dysfunction. |
The lack of a widely accepted definition and variations in nomenclature worldwide for BPS, as well as the absence of clear diagnostic criteria, has meant that true incidence and prevalence rates are difficult to determine. Furthermore, prevalence figures vary significantly, depending upon whether the data is from patient self-reports, physician diagnoses, or symptom-based surveys. Historically, using stricter diagnostic criteria, BPS was infrequently diagnosed, with a worldwide prevalence of 0.1% ( ). However, using contemporary, more inclusive diagnostic criteria, the prevalence has been reported to be much higher, up to 6.5% in women (up to 7.9 million adult women in the United States) ( ).
One of the earliest epidemiological studies of almost one million people in Finland reported a prevalence of BPS of 18.1 per 100,000 in women, and a joint prevalence in men and women of 10.6 per 100,000 ( ). Ten percent of the cases were in men and 10% were severe cases. Patient self-report surveys in the United States have also shown that this condition is common, with reported prevalence rates of 865 per 100,000 in women (approximately 0.5% of the population) ( ). Using symptom-based surveys, a prevalence rate of BPS symptoms was reported to be 1.7% in women under the age of 65, increasing to 4% in women over 80 years old. Another study reported a 17 times higher incidence in first-degree relatives of patients with BPS ( ). Despite this wide variation in prevalence figures and difficulties with accurate data collection, it is clear that the prevalence of BPS/IC is significantly higher than previously thought.
Studies consistently show a higher incidence in women when compared to men of at least 5:1, with men typically diagnosed at an older age and with a higher percentage of Hunner’s ulcers ( ). BPS/IC is typically a relapsing-remitting condition and symptoms plateau after approximately 5 years ( ). The Boston Area Community Health Survey, a community-based epidemiological survey, found that a history of emotional, sexual, or physical abuse were risk factors for developing BPS symptoms, and some cases of BPS can be associated with other conditions, such as irritable bowel syndrome, fibromyalgia, and chronic fatigue syndrome (in 20%–27% of patients), suggesting that BPS is part of a systemic condition and not one solely confined to the bladder ( ).
The etiology of BPS/IC remains unknown, but is likely to be multifactorial and more complex than previously thought. It is now thought that BPS is part of a more generalized somatic syndrome rather than an isolated, end-organ, bladder disease, and a number of theories regarding its pathophysiology exist. It is likely that many combined factors play a role in the pathogenesis of this condition.
It is thought that an initial unidentified insult to the bladder (possibly infection, autoimmune mechanisms, overdistension, or primary neurogenic inflammation) leads to urothelial damage. Consequent defects in the glycosaminoglycan (GAG) layer of the bladder result in increased permeability of the urothelium (“leaky” urothelium), allowing noxious substances in the urine to pass through to the submucosal nerve filaments, leading to bladder pain ( ).
Mast cells are thought to play a key role in the pathophysiology of bladder pain. They secrete significant amounts of proinflammatory mediators, such as histamine, leukotrienes, and cytokines, leading to chronic inflammation and pain. In support of this concept, the mast cell count in bladder tissue from patients with ulcer-type BPS is 10-fold higher than in those with nonulcer BPS and controls ( ). Many other inflammatory mediators, such as CRP and nerve growth factor, have also been found to be significantly increased in patients with BPS ( ). The use of mast cells as a biomarker for this condition has been investigated, and although subepithelial mast cell distribution was found to be characteristic of BPS with Hunner’s ulcers, detrusor mastocytosis had poor predictive value for BPS ( ).
Neurogenic inflammation, as a result of activation of sensory nerves with subsequent release of neuropeptides such as substance P, which in turn can stimulate mast cell degranulation, has also been hypothesized for the pathophysiology of BPS. In support of this concept, a number of studies have reported increased sympathetic nerve activity in patients with BPS ( ). Recent studies evaluating central nervous system (CNS) imaging have demonstrated characteristic brain white matter abnormalities in patients with BPS/IC, again suggesting neuropathological contributions to this condition ( ). Pelvic organ cross-sensitization, in which noxious stimulation in one pelvic structure can affect neighboring pelvic organs through convergent neural pathways, is also thought to play a role ( ).
Other theories for the pathogenesis of BPS have included autoimmune mechanisms with increased autoantibodies in BPS ( ), hypoxia-related mechanisms ( ), antiproliferative factor ( ), and urinary toxins ( ), but findings have been conflicting.
Studies using quantitative gene expression have shown upregulation of specific genes, encoding inflammatory mediators (e.g., FGF7 and CCL21) in BPS patients when compared to controls. CCL21 was also shown to be a pain mediator in an animal model of BPS, increasing bladder excitability and pain, and blockade of this inflammatory mediator could reduce the pain and inflammation seen in BPS ( ). Further research in these areas will provide greater insight into the pathophysiology of this condition and potential opportunities for targeted therapeutic approaches.
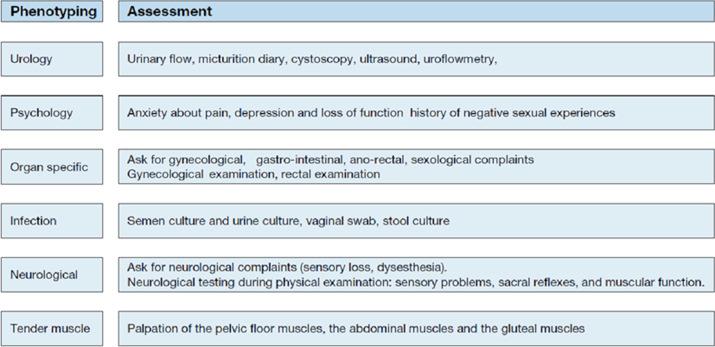
As described earlier, BPS is considered as one of the urological, chronic pelvic pain syndromes and diagnosis is largely based on clinical symptoms of pain, perceived to arise from the urinary bladder with associated urinary symptoms, in the absence of other identifiable causes (e.g., infection, radiation cystitis, cyclophosphamide cystitis, lower urinary tract stones, pelvic cancer, and urethral diverticulum). As such, it is therefore a diagnosis of exclusion, based on a thorough history and focused physical examination. It is suggested that patients with chronic pelvic pain be phenotyped using the “UPOINT” system to guide management strategies ( Fig. 123.2 ). Symptoms should be further evaluated using a bladder diary and a validated patient-reported symptom questionnaire, such as the O’Leary–Sant symptom score.
Although there is no diagnostic test for BPS, appropriate investigations should be performed that exclude other identifiable pathology. This should include urinalysis to exclude urinary infection or hematuria, pelvic MRI to identify pelvic pathology, and cystoscopy to better phenotype patients.
Although cystoscopy is not considered mandatory in simple cases, according to the American Urological Association (AUA) guidelines, the authors perform cystoscopy under anesthesia in all patients to assess bladder capacity and phenotype patients as nonulcer or ulcer-type BPS ( ). The presence or absence of ulcers can have implications for treatment decisions as patients with Hunner’s ulcers are reported to respond better to certain treatments than patients without them. Furthermore, cystoscopy with biopsy can help to rule out other pathologies such as carcinoma-in-situ or tuberculous cystitis and is recommended by the European Association of Urology (EAU) guidelines ( ). Patients with ulcer BPS (ESSIC type 3) will typically have a small capacity, fibrotic bladder with the presence of Hunner’s ulcers (red mucosal inflammatory lesions associated with small blood vessels radiating toward a central pale scar with a characteristic deep rupture through the mucosa and submucosa, on distension). After low-pressure hydrodistension (80 cm H 2 O for 1–2 min), the bladder is reinspected and the area of ulceration typically “cracks” and demonstrates waterfall bleeding. The presences of glomerulations (punctate petechial hemorrhages) were once considered a key feature of BPS, but glomerulations can be seen in patients without BPS and the severity of glomerulations does not correlate with the severity of symptoms ( ). A systematic review has concluded that there is no evidence that glomerulations should be included in the diagnosis or phenotyping of BPS/IC ( ). Other investigation, such as urine cytology or urodynamics, should be considered in individual patients, if appropriate.
Principles of management of patients with BPS are to improve quality of life and encourage realistic patient expectations. The optimal management, if possible, should involve a multidisciplinary approach that consists of urologists, gynecologists, colorectal surgeons, pain specialists, nurses, dieticians, physiotherapists, and psychologists. Treatments should follow a step-wise approach, starting with the most conservative interventions first ( Table 123.3 ).
| First line | Patient educationBehavioral therapyDietary modificationPsychological inputPelvic floor physiotherapyMultimodal pain therapy |
| Second line | Oral
|
Intravesical
|
|
| Third line | Bladder hydrodistensionTransurethral fulguration of ulcers (with electrocautery or laser) |
| Fourth line | Intravesical botulinum toxin ASacral neuromodulationCyclosporin A |
| Fifth line | Ileal conduit urinary diversion (+/− cystectomy)Cystectomy and orthotopic bladder substitute |
Conservative measures consist of patient education regarding normal bladder function, the chronic nature of BPS and promoting realistic expectations for management. Behavioral modification with timed voiding, fluid modification, and bladder training should be discussed and tried. Physiotherapy with biofeedback and myofascial release may promote pelvic floor muscle relaxation ( ). Dietary factors (e.g., acidic beverages, spicy foods, alcohol) have been reported to exacerbate symptoms in up to 90% of patients with BPS, so personalized dietary manipulation should be part of the treatment strategy for these patients ( ).
A large number of oral therapies have been trialed for patients with BPS. However, the evidence base for the majority is limited and so only a few of these oral therapies are recommended for use. Amitriptyline is an antidepressant that also blocks H1-histaminergic receptors and stabilizes mast cells. It has been shown in randomized controlled trials (RCTs) to improve symptoms of bladder pain, when compared to placebo, although a significant number of patients stop treatment due to side effects of the therapy; the beneficial effect is predominantly for those who can tolerate a dose of ≥50 mg of amitriptyline ( ). The antihistamines, hydroxyzine and cimetidine, inhibit bladder mast cell activation. Early studies of hydroxyzine, an H 1 -receptor antagonist, appeared promising, but a more recent US National Institutes of Health’s (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) RCT reported a global response rate of only 31%, when compared to 20% for placebo, and this did not reach statistical significance ( ). Cimetidine, an H 2 -receptor antagonist, has shown significant improvement of pain and frequency scores in an RCT of 36 patients, but the number of participants that were randomized to cimetidine when compared to placebo was not reported in this study and so the number of patients with successful outcomes is unknown ( ).
Pentosan polysulfate is a synthetic GAG analog and theoretically may replenish the damaged GAG layer of the bladder urothelium of BPS patients. Oral pentosan polysulfate is the most extensively studied oral therapy for BPS and has been investigated in a number of RCTs. Its beneficial effect is related to duration of therapy rather than dose, and is reported to have better results in patients with ulcer-BPS, although these trials have reported conflicting results ( ).
The EAU guidelines give a grade-A recommendation to amitriptyline and oral pentosan polysulfate, whereas the AUA guidelines give a grade-B recommendation to amitriptyline, oral pentosan polysulfate and cimetidine, and a grade C recommendation to hydroxyzine. Multimodal pain management with nonsteroidal antiinflammatories, short-term opioids, or neuropathic analgesics (membrane stabilizing agents), such as gabapentin, should also be used with input from physician pain specialists.
Repeated intravesical instillation of agents to restore the GAG layer remains the cornerstone of management for BPS. Instillation of lidocaine/sodium bicarbonate and pentosan polysulfate have both been given a grade-A recommendation by the EUA, with grade-B recommendations for hyaluronic acid and chondroitin sulfate. Pentosan polysulfate, hyaluronic acid and chondroitin sulfate all aim to replenish the damaged GAG layer of the bladder urothelium and small nonrandomized studies report moderate success rates with repeated instillation, but the effects wear off once the treatments are discontinued. Studies, investigating the use of electromotive drug administration (EMDA) with lidocaine and dexamethasone to enhance drug penetration across the urothelium, have shown promising results, but larger RCTs are required to assess the true benefit of this technique ( ).
Symptom flares may be provoked by factors including emotional or physical stress, diet, and sexual intercourse. Patient education that identifies and eliminates these factors is important for preventing symptom flares, but in cases of severe acute exacerbation of symptoms, management with acute pain medications, a short course of steroids or intravesical therapies have been used as “rescue” therapies ( ).
A number of intravesical “cocktails” have been described that reduces the symptoms of acute symptom flares. Parsons solution (a mixture of heparin, 2% lidocaine, and sodium bicarbonate) has been shown to result in an immediate improvement of symptoms in 94% of patients and an improvement in 68% of patients experiencing a flare. Using an intravesical mixture of sodium bicarbonate, heparin, hydrocortisone, bupivacaine, and gentamicin has also been reported ( ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here