Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The autonomic nervous system can be viewed as the interface between the central nervous system and the viscera, glands, and blood vessels. Integration of the neural trafficking among the afferent and efferent autonomic nerves and their associated autonomic neurons, maintains a delicate homeostasis of the function of the entire body. In mammalian hearts, the efferent sympathetic preganglionic neurons are located in the intermediolateral columns of the gray matter of the spinal cord; the preganglionic fibers of these neurons pass through or synapse with the paravertebral ganglia (e.g., the stellate ganglia). The stellate ganglia, receiving neural inputs mainly from spinal nerves C6–T2, are the key neural structures for cardiac sympathetic innervation. The efferent parasympathetic preganglionic neurons are located in the motor nuclei of the vagus nerves (e.g., nucleus ambiguous) in the brainstem, from which the vagus nerves carry the preganglionic parasympathetic fibers to the heart. The parasympathetic postganglionic neurons are concentrated mainly in the ganglionated plexi (GP) embedded in epicardial fat pads, and the efferent postganglionic parasympathetic fibers are distributed over the entire heart. The afferent autonomic fibers, both sympathetic and parasympathetic, course along the cardiac plexus in the thorax and eventually reach the sensory neurons in the nodose ganglia at the base of the skull and the dorsal root ganglia of the spinal cord. These afferent nerves and ganglia mediate important cardiorespiratory reflexes (e.g., baroreflex) and the pain sensation from the heart to the brain. ,
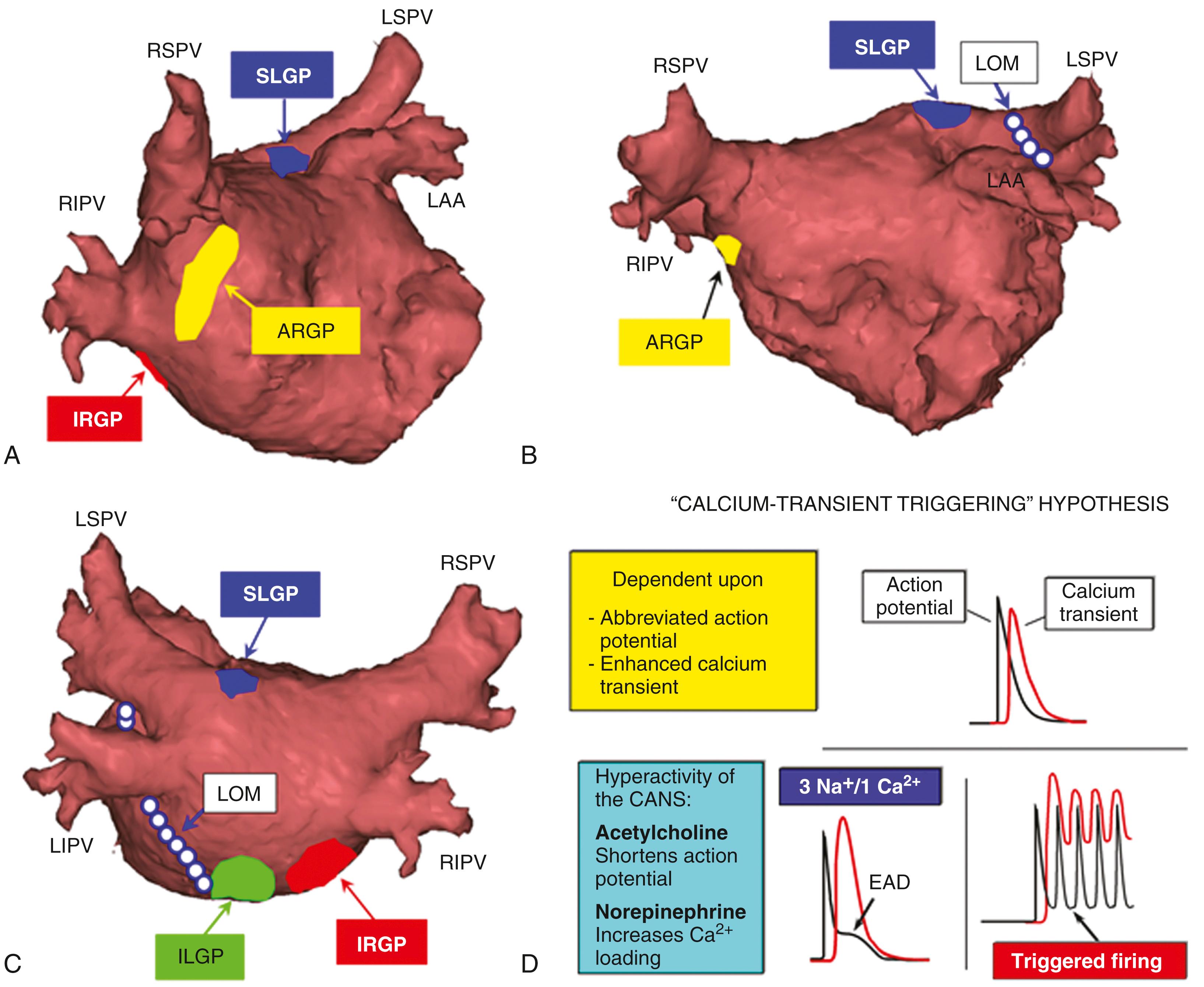
The cardiac autonomic nervous system (CANS) regulates vascular tone, contractility, and electrophysiology by transducing and integrating the afferent and efferent autonomic trafficking. , Autonomic control of the heart is mediated by highly integrated intrinsic and extrinsic CANS. , The extrinsic CANS mainly consists of ganglia and their axons located outside the heart. The nucleus ambiguous, dorsal vagal nucleus, and vagus nerves constitute most of the parasympathetic limb of the extrinsic CANS, whereas the neurons in the intermediolateral column of the spinal cord, the stellate ganglia, and their axons en route to the heart make up most of the sympathetic limb of the extrinsic CANS. The intrinsic CANS is mainly composed of sympathetic and parasympathetic nerves and GP on the heart itself or along the great vessels in the thorax such as pulmonary artery, aorta, superior vena cava (SVC), and pulmonary veins (PVs). The stellate ganglia serve as the “head stage” for the sympathetic innervation of the heart. The postganglionic sympathetic fibers, mainly from the stellate ganglia, constitute the vast majority of the sympathetic innervation to both the atrium and ventricle. The major atrial GP are embedded in the epicardial fat pads and contain up to several hundred autonomic neurons ( Fig. 42.1A–C ). The distribution of the major ventricular GP is limited to the proximal segments of the coronary arteries; they are in general small and not as extensive on the ventricles.
The intrinsic CANS appears to function interdependently and independently from the extrinsic CANS, evidenced by its retaining nearly full control of the cardiac physiology after autotransplantation. , A cooperative interaction between the extrinsic and intrinsic CANS maintains a homeostasis that facilitates balanced cardiac physiologic functions. The major atrial GP are located adjacent to the PV-atrial junction or the junction of the right atrium (RA) and the superior or inferior vena cava. Chiou and colleagues discovered that the efferent parasympathetic fibers in the vagus nerves converge at a GP before innervating the heart. This right pulmonary artery-aortico (RPA-Ao) GP, at the junction of the right pulmonary artery, aorta, and SVC was coined as the head stage GP because the bradycardia response induced by vagal stimulation in canine hearts was nearly abolished if the RPA-Ao GP was ablated.
The different nomenclature used by anatomists introduced a great deal of confusion for scientific communication. In this chapter, we use the nomenclature based on clinical anatomy, that is, GP’s relation to PVs (see Fig. 42.1A–C ). The superior left GP (SLGP) and inferior left GP (ILGP) are located adjacent to the PV-atrial junction of the left superior PV (LSPV) and left inferior PV, respectively. The anterior right GP (ARGP) is situated near the right superior PV-atrial junction. The inferior right GP (IRGP) extends from the inferior right PV-atrial junction to the crux of the heart near the junction of the RA and inferior vena cava.
It was once thought that the ARGP specifically innervates the sinus node, whereas the IRGP at the crux of the heart only innervates the atrioventricular (AV) node. Recent studies indicate that the intrinsic CANS forms a complex neural network and GP serve as the “integration centers” to control the physiologic functions of the heart. , , For example, high-frequency stimulation (HFS; 20 Hz) to the SLGP also markedly slowed the sinus rate (SR), proving that the ARGP is not the only GP innervating the sinus node. Ablation of the ARGP greatly attenuated, but did not eliminate, the SR slowing response induced by SLGP stimulation, indicative of ARGP’s role as the gateway GP for the sinus node and the presence of other neural pathways bypassing the ARGP. Ablation of the four major atrial GP and ligament of Marshall (LOM) exerts potent inhibitory effects on the activity of the CANS, supporting clinical implications targeting these GP to treat atrial fibrillation (AF).
Until the last 2 decades, it was believed that the sympathetic component of the intrinsic CANS is composed exclusively of postganglionic sympathetic fibers and all the cardiac autonomic neurons are parasympathetic neurons expressing cholinergic markers. With the advances of immunohistochemistry, subpopulations of cardiac autonomic neurons expressing various neurotransmitter markers have been identified. The presence of the peptidergic, nitrergic, and noradrenergic neurons along with their associated neurotransmitters such as neuropeptide Y, vasostatin, vasoactive intestinal peptide, nitric oxide synthase, and angiotensin II strongly indicate that autonomic control of cardiac physiology involves a milieu of neurotransmitters beyond acetylcholine and norepinephrine. Neuropeptide Y, coreleased by prolonged sympathetic activation, reduces acetylcholine release from the neighboring vagal nerve ending; it is a good example of sympathovagal cross talk. Notably, coronary sinus neuropeptide Y levels originating from increased neuronal trafficking and release from stellate ganglion neurons predict adverse outcomes in patients with chronic heart failure with reduced ejection fraction. These noncholinergic, nonadrenergic neurotransmitters often exert effects similar to cholinergic or adrenergic agonists or antagonists. Using cholinergic and adrenergic blockers alone to “eliminate” the CANS control is clearly an oversimplified approach. , Liu and coworkers demonstrated that until an antagonist of VIP ([Ac-Tyr1,D-phe2]-VIP) was administered, vagal stimulation continued to induce AF in canine hearts despite GP ablation + atropine + esmolol. The release of these neurotransmitters/modulators is often highly dependent on the level of neuronal stimulation, and they tend to be slowly diffusing molecules that often function as neuromodulators rather than classical neurotransmitters. Better understanding of the arrhythmogenic potential of these noncholinergic, nonadrenergic neurotransmitters may facilitate the development of new antiarrhythmic agents to treat AF.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here