Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ultrasound (US) has an important role in planning and guiding many gynecologic interventions.
Prior to endometrial ablation, US may be used to detect focal lesions (e.g., polyps or leiomyomas), assess for tubal disease such as hydrosalpinx, and search for uterine anomalies.
Whereas magnetic resonance imaging (MRI) remains the gold standard for evaluating patients prior to uterine artery embolization (UAE), US can be used to identify several relative contraindications. Following UAE, US has an important role in assessing post procedural complications such as necrosis or superinfection of the uterus or leiomyomas.
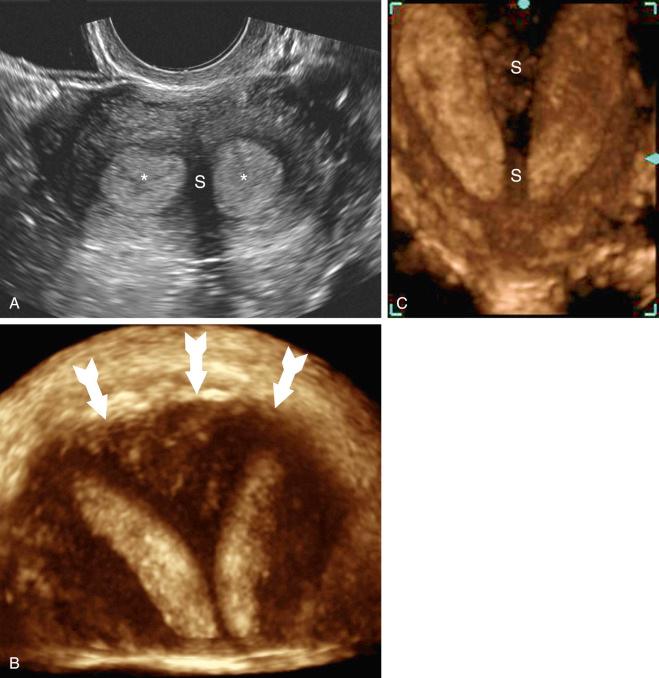
MRI remains the gold standard for diagnosis and classification of congenital uterine anomalies. However, three dimensional (3D) US can provide important information with significant impact on counseling regarding reproductive prognosis and approach to repair.
Transabdominal US guidance is extremely useful when accessing the endometrial cavity in patients with cervical stenosis and Asherman syndrome, or when placing brachytherapy devices; direct guidance reduces the risk of uterine perforation or creation of a false channel during instrumentation.
US is increasingly used to assess for correct placement of Essure microinsert devices in the proximal fallopian tube, although hysterosalpingography still remains the gold standard.
3D US is considered the gold standard to document correct IUD placement in the endometrial cavity.
US guidance can be used to safely guide transvaginal or transabdominal percutaneous biopsies of pelvic masses and drainage of pelvic fluid collections following careful consultation with the referring gynecologist.
Gynecologic interventions have undergone significant changes over the past few decades. Procedures once exclusively performed in the operating room under general anesthesia may now be performed under local anesthesia in an office setting. Sonography has been a factor in allowing better preoperative investigation by excluding certain gynecologic disease, and its use in the clinic can guide access that previously required surgical exploration. The goal of this chapter is to describe the information required from ultrasound imaging of the pelvis to assist in gynecologic interventions. This chapter is organized according to gynecologic intervention, in hopes of better conveying the information that is necessary for a safe and successful procedure. Seven common gynecologic interventions and treated conditions will be covered: endometrial ablation, uterine artery embolization (UAE), repair of congenital anomalies of the uterus, guidance for endometrial interventions for cervical stenosis and Asherman syndrome, confirmation of correct Essure microinsert placement for tubal sterilization, location of malpositioned IUDs, and pelvic biopsies and drainages. Chapters on abnormal uterine bleeding, adnexal masses, ectopic pregnancy, and infertility are presented elsewhere in this textbook and, therefore, are not covered in this chapter.
Key questions to consider before endometrial ablation:
Is an endometrial polyp or mass present?
Is a leiomyoma present? If so, is it submucosal?
Is there evidence of tubal disease such as hydrosalpinx?
Is a uterine anomaly present?
Endometrial ablation is an intervention offered to women who suffer from heavy menstrual bleeding that interferes with normal daily activities enough to warrant intervention, but without a known lesion causing bleeding. Known causes for uterine bleeding such as uterine leiomyomas, endometrial polyps, endometrial cancer or precancerous lesions are more effectively treated by other methods. Furthermore, endometrial ablation in the presence of an endometrial cancer or precancer may lead to a delay in diagnosis.
Historically, endometrial ablation was performed in the operating room under general anesthesia via hysteroscopy. Use of a hysteroscope provides the surgeon with the ability to look into the uterine cavity and manually ablate the endometrium with a ball electrode (rollerball). This procedure causes desiccation of the endometrium in hopes that the endometrium will no longer bleed. Laser energy has also been used, as well as a loop electrode to shave or resect the endometrium. However, these three methods require advanced hysteroscopic skills and may expose the patient to hypotonic fluids to distend the endometrial cavity, thus placing her at risk for hyponatremia which, in some cases, can be associated with life-threatening herniation of the brainstem. Because these surgeries can be difficult to perform, five newer endometrial ablation devices have been approved by the U.S. Food and Drug Administration (FDA). These newer endometrial ablation methods have been approved since 1997 and are often referred to as global endometrial ablation (GEA) devices because the endometrial cavity is treated as a whole through a more automated process, rather than by a manual approach that ablates sections of the endometrium with a rollerball, laser, or loop resection. GEA methods employ a variety of modalities to ablate the endometrium, including a thermal balloon, circulated hot fluid, cryotherapy, radiofrequency electrosurgery, and microwave energy. GEA devices allow endometrial ablation to be performed with greater ease in the office, without the risk of fluid overload syndrome that has been associated with traditional hysteroscopic surgery performed with electrolyte-poor fluid. Though rates of amenorrhea have a wide range (14-55%) among GEA methods, patient satisfaction rates are uniformly high, at approximately 85%.
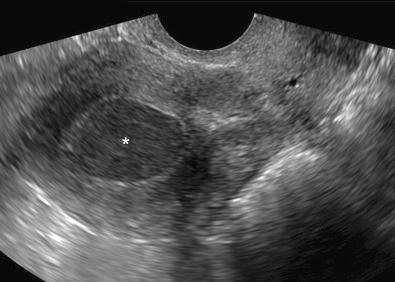
Before considering endometrial ablation, a number of contraindications should be excluded ( Table 37-1 ). Gynecologic ultrasound and particularly saline infusion sonohysterography (SIS) are helpful in assessing for submucosal leiomyomas ( Fig. 37-1 ) and endometrial polyps, which would be optimally treated with hysteroscopic resection. Excluding such conditions prior to endometrial ablation avoids exposing patients to unnecessary risks of a treatment that will have a lower efficacy as a result of underlying abnormality.
|

Complications of endometrial ablation may be found on ultrasound examination in the postoperative patient who presents with pain or bleeding. Such complications include infection; uterine perforation; thermal injury to bladder, bowel, or ureter; hematometra ( Fig. 37-2 ); pregnancy-related complications; and the development of subsequent endometrial cancer (not detected with the preoperative biopsy). In a meta-analysis comparing endometrial ablation procedures, the incidence of infectious complications included endometritis (1.4-2.0%), myometritis (0-0.9%), pelvic inflammatory disease (1.1%), and pelvic abscess (0-1.1%).
Pregnancy following ablation has been reported to occur in 0.7% of women who have undergone endometrial ablation and is associated with poor obstetric outcomes. It has been reported as early as 5 weeks after ablation and as late as 12 years postoperatively (following tubal reanastomosis in a planned pregnancy). The chance of pregnancy occurring after endometrial ablation with tubal sterilization is even lower, estimated to be 0.002%, or 1 in 50,000. Though successful pregnancies have been reported, there appears to be a greater risk of complications including preterm birth, intrauterine scarring/uterine chambering (creating separate uterine compartments), and postpartum hemorrhage. It is hypothesized that the risk of preterm birth is in part due to narrowing or chambering of the endometrial cavity, resulting in a smaller area for the gestation. One of the unintended consequences of office endometrial ablation is the inability to perform concomitant tubal sterilization, which could lead to an undesired increased incidence of pregnancy in this population.
Contracture and scarring of the endometrium constitute an expected effect of endometrial ablation. However, when focal areas of normal endometrium persist after a partial ablation, obstructed egress of menses with associated pain may occur. This can manifest as hematometra within the body of the uterine cavity (central hematometra) or at the cornual region. Postablation tubal sterilization syndrome (PATSS) was initially reported in 1993 in a series of six patients presenting with unilateral or bilateral pelvic pain and vaginal spotting subsequent to tubal sterilization and endometrial ablation. The patients were all noted to have scarring of the endometrial cavity with swelling of the proximal portion of one or both fallopian tubes. Symptomatic relief was achieved in five out of six patients with removal of the fallopian tubes. The incidence of PATSS is approximately 6% to 8%, and it usually develops within 2 to 3 years of endometrial ablation. A high index of clinical suspicion is key to the diagnosis of PATSS, as patients typically present with cyclic cramping with or without menses in the setting of prior endometrial ablation and tubal sterilization. The role of sonography in diagnosing PATSS has not been well evaluated. Usually the confirmatory diagnosis is made surgically. However, magnetic resonance imaging (MRI) during periods of symptomatic cramping may be useful using T2-weighted images to look for blood trapped in the uterine cornu. Another concern regarding the scarring of the endometrium that accompanies endometrial ablation is the difficulty with subsequent evaluation of the endometrium with endometrial sampling, sonography, or SIS. The safety of endometrial ablation has not been well studied in women who are at an increased risk of developing endometrial cancer or endometrial hyperplasia. These risks include nulliparity, chronic anovulation, obesity, diabetes mellitus, tamoxifen or selective estrogen receptor modulator (SERM) therapy, and hereditary nonpolyposis colorectal cancer.
Approximately half of the serious complications associated with contraindications to endometrial ablation may be identified preoperatively, as was demonstrated in a series of patient reports entered using the FDA Manufacturer and User Facility Device Experience (MAUDE) database. The initial MAUDE database report described 85 complications in 62 patients. They included major complications, such as 8 cases of thermal bowel injury, 30 cases of uterine perforation, 12 cases requiring emergent laparotomy, and 3 intensive care unit admissions. One patient developed necrotizing fasciitis and eventually underwent vulvectomy, ureterocutaneous ostomy, and bilateral below-the-knee amputations. One of the patients with thermal injury to the bowel died. The contraindications to GEA are summarized in Table 37-1 .
Though pelvic ultrasound examination is often performed as part of the preoperative evaluation, a strong case for the use of SIS could be made as a better modality to exclude contraindications such as submucosal leiomyomas. If a polyp is present, endometrial ablation is not necessary, as a simple polypectomy can be performed and bleeding will most often resolve. Likewise, if submucosal leiomyomas are present, hysteroscopic resection of the leiomyoma is indicated; this is an outpatient procedure not associated with the same risk of endometrial scarring as endometrial ablation. Tubal disease such as hydrosalpinx or tubo-ovarian abscess should be treated prior to endometrial ablation to avoid postoperative infectious complications. Lastly, the presence of a uterine septum or other uterine anomaly would make several of the described automated ablation technologies impossible to perform, as the devices may not fit within the endometrial cavity and thus would place the patient at risk for unnecessary anesthesia. Of note, superficial adenomyosis is reasonable to treat with endometrial ablation, although there are reports of decreased efficacy if adenomyosis is extensive.
Key questions to consider for UAE:
Is the leiomyoma pedunculated?
Is the leiomyoma submucosal in location?
Is there leiomyoma growth in a postmenopausal woman?
Is there concurrent endometrial disease that may be causing bleeding?
Is adenomyosis present?
Is there unsuspected adnexal abnormality?
UAE for the treatment of leiomyomas was first described in 1995. In most circumstances, this procedure is performed by interventional radiologists. A 4F or 5F catheter is placed into the uterine arteries via a transcutaneous femoral approach. Polyvinyl alcohol particles or tris-acryl gelatin microspheres are injected into the uterine arteries to devascularize the uterus and therefore cause shrinkage of leiomyomas. Supplemental metal coils may be used to assist with vascular occlusion. The patient is usually able to return home within 23 hours of the procedure. There is typically a period of ischemic pain for 2 to 3 hours after embolization, followed by a plateau of pain, and then gradual reduction of pain over the next 2 to 3 days. The advantages of this procedure compared to myomectomy or hysterectomy are a faster recovery and return to normal activities.
Since 1995, there has been considerable progress in the successful performance of UAE. Most initial published reports were case series describing the technique or reports of short-term outcomes. Subsequently, larger multicenter series and nonrandomized controlled studies and, finally, randomized clinical trials (RCTs) have been published. Unfortunately, the information from RCTs regarding long-term outcomes is limited owing to short follow-up intervals, although long-term outcomes have been reported in nonrandomized trials. Broder and associates reported up to 5-year follow-up data in an observational study of UAE compared to myomectomy. In the UAE group, there was a higher reoperation rate of 29% (15/51) compared to 3% (1/30) in the myomectomy group ( P = 0.004). When considering subjective variables, such as worsening of symptoms and being dissatisfied, 39% (20/51) were considered clinical failures in the UAE group compared to 30% (9/30) in the myomectomy group, a nonsignificant difference ( P = 0.4). Additional 5-year follow-up data were published in a case series by Spies and colleagues. In patients undergoing UAE, they reported a 20% reoperation rate (hysterectomy 13.7%, myomectomy 4.4%, repeat embolization 1.6%) and a 25% chance of failure to control symptoms. Short-term failure (at 12 months) was three times more likely in those with less than the median shrinkage of a dominant leiomyoma. Failure to shrink at the 12-month interval was associated with a five times greater likelihood of long-term failure.
Regarding short-term outcomes, a large multicenter study of over 500 patients undergoing UAE in eight Ontario hospitals reported favorable 3-month outcomes with regard to dominant leiomyoma volume reduction (42%), median leiomyoma life-impact scores, mean menstrual duration, dysmenorrhea, and urinary frequency/urgency.
The EMMY trial (EMbolization vs. hysterectoMY) was a RCT involving 28 Dutch hospitals and compared UAE to hysterectomy. Comparison of safety demonstrated a similar major complication rate of 4.9% for UAE and 2.7% with hysterectomy ( P = 0.68), but a higher rate of readmission and minor complications in the UAE group (11.1% vs. 0%; P = 0.003 and 58.0% vs. 40.0%; P = 0.024; risk ratio 1.45 [1.04-2.02]), respectively. Another multicenter comparative trial of UAE versus myomectomy reported similar clinical findings. A second EMMY publication reported a comparison of the short-term outcomes of pain and time until return to daily activities. Compared to patients undergoing hysterectomy, patients undergoing UAE had significantly less pain during the first 24 hours postoperatively ( P = 0.012) and returned to work sooner (28.1 vs. 63.4 days). Five RCTs comparing UAE to myomectomy and hysterectomy were also evaluated in a Cochrane review. The review found that outpatient UAE resulted in a similar satisfaction rate compared with hysterectomy and myomectomy, but offered the advantage of a shorter hospital stay and quicker return to activities. However, UAE was associated with a higher minor complication rate and an increased likelihood of surgical intervention within 2 to 5 years of the initial intervention.
The overall complication rate of UAE has been reported to be 5% and is similar when applying the American College of Obstetricians and Gynecologists (ACOG) criteria for perioperative morbidity. Complications range from fever to uterine necrosis and, very rarely, death. Collateral damage to the ovary resulting in premature ovarian failure has also been reported. However, this complication has been reported primarily in patients over age 45 years and may be associated with reduced ovarian reserve.
Pregnancy after UAE remains understudied, with variable complication rates reported. An observational study reported a higher rate of preterm delivery compared to laparoscopic myomectomy (odds ratio 6.2 [1.4, 27.7]). Other studies have raised concerns regarding abnormal placentation (12.5%) and high cesarean delivery rates (88%), but did not report other major risk factors. The effect of UAE on pregnancy is therefore uncertain. However, careful surveillance is required should a patient become pregnant following UAE.
Although MRI has become the standard preprocedural imaging tool in women considering UAE, most women with symptoms first undergo pelvic ultrasound imaging for confirmation of the presence of leiomyomas. Though ultrasound imaging is not as useful as contrast-enhanced MRI in determining leiomyoma characteristics such as tissue viability, ultrasound imaging can be helpful in assessing for pedunculated submucosal and subserosal ( Fig. 37-3 ) leiomyomas, both of which have been associated with an increased risk of complications following UAE.
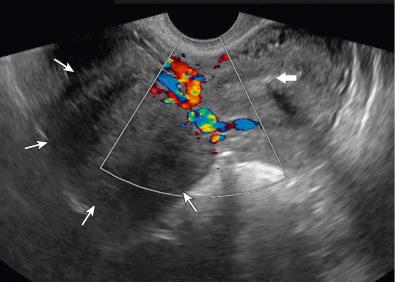
Pedunculated submucosal (type 0) leiomyomas are defined as being located entirely within the endometrial cavity with no myometrial extension. It should be noted that although leiomyomas may be associated with abnormal uterine bleeding or pelvic pressure symptoms involving the bladder or rectum, leiomyomas are also commonly asymptomatic. Therefore, it is important to exclude other causes of abnormal uterine bleeding (especially endometrial cancer) and to assess for possible endometrial polyps or submucosal leiomyomas. Ultrasound imaging may also detect adenomyosis, which may cause similar symptoms as leiomyomas and, if present, may decrease the efficacy of UAE. Lastly, enlarging leiomyomas, though usually not associated with sarcoma in reproductive age women, are of great concern in postmenopausal women. An increase of more than 20% in measured leiomyoma diameter by ultrasound imaging is considered to represent true growth, not measurement variation. Typically, leiomyomas will reduce in size during menopause. Thus, treatment of leiomyomas with UAE is generally contraindicated in postmenopausal women. The prevalence of sarcomas is approximately 0.2% (1 in 500) in women undergoing hysterectomy or myomectomy for presumed benign leiomyomas; this potential complication has gained attention with recent publicity regarding the dangers of power uterine morcellation. There are currently no ultrasound imaging or MRI features that allow the accurate diagnosis of uterine sarcoma. Contrary to prior belief, rapidly enlarging leiomyomas in reproductive age women have specifically not been found to predict sarcoma. Contraindications to UAE are summarized in Table 37-2 .
Key questions to consider for repair of congenital anomalies of the uterus:
Does the patient have two structurally normal kidneys?
If there is a midline septum, is there notching at the uterine fundus?
Are two ovaries present?
Is a vagina present?
Is there a portion of uterine tissue that may become obstructed?
Are there one or two cervices?
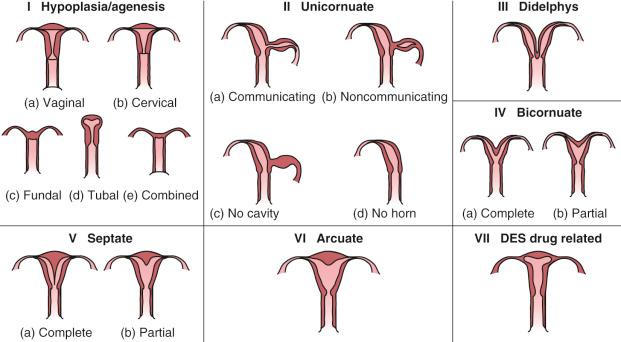
The prevalence of congenital anomalies of the reproductive tract is estimated to be as high as 7% in the female population. These anomalies are usually not recognized until they present with pain (obstructed menses), pregnancy complications (fetal malpresentation, preterm labor, recurrent pregnancy loss), or infertility. There are a number of classification systems for müllerian anomalies. The American Fertility Society/American Society of Reproductive Medicine (AFS/ASRM) proposed a standard classification of müllerian anomalies based on vertical fusion defects ( Table 37-3 and Fig. 37-4 ). Because of the many variations and complexities associated with these defects, a system known as the Vagina Cervix Uterus Adnexa-associated Malformation (VCUAM) classification system was proposed after being validated in a group of 99 women. ( Table 37-4 ). In 2013, the European Society of Human Reproduction and Embryology (ESHRE) and the European Society for Gynaecological Endoscopy (ESGE) established a common working group and developed a classification system based largely on anatomy that is clinically oriented ( Fig. 37-5 ).
|
| Vagina (V) | 0 | Normal |
| 1a | Partial hymenal atresia | |
| 1b | Complete hymenal atresia | |
| 2a | Incomplete septate vagina <50% | |
| 2b | Complete septate vagina | |
| 3 | Stenosis of the introitus | |
| 4 | Hypoplasia | |
| 5a | Unilateral atresia | |
| 5b | Complete atresia | |
| S1 | Sinus urogenitalis (deep confluence) | |
| S2 | Sinus urogenitalis (middle confluence) | |
| S3 | Sinus urogenitalis (high confluence) | |
| C | Cloacae | |
| + | Other | |
| # | Unknown | |
| Cervix (C) | 0 | Normal |
| 1 | Duplex cervix | |
| 2a | Unilateral atresia/aplasia | |
| 2b | Bilateral atresia/aplasia | |
| + | Other | |
| # | Unknown | |
| Uterus (U) | 0 | Normal |
| 1a | Arcuate | |
| 1b | Septate <50% of the uterine cavity | |
| 1c | Septate >50% of the uterine cavity | |
| 2 | Bicornuate | |
| 3 | Hypoplastic uterus | |
| 4a | Unilaterally rudimentary or aplastic | |
| 4b | Bilaterally rudimentary or aplastic | |
| + | Other | |
| # | Unknown | |
| Adnexa (A) | 0 | Normal |
| 1a | Unilateral tubal malformation, ovaries normal | |
| 1b | Bilateral tubal malformation, ovaries normal | |
| 2a | Unilateral hypoplasia/gonadal streak (including tubal malformation if appropriate) | |
| 2b | Bilateral hypoplasia/gonadal streak (including tubal malformation if appropriate) | |
| 3a | Unilateral aplasia | |
| 3b | Bilateral aplasia | |
| + | Other | |
| # | Unknown | |
| associated Malformation (M) | 0 | None |
| R | Renal system | |
| S | Skeleton | |
| C | Cardiac | |
| N | Neurologic | |
| + | Other | |
| # | Unknown |
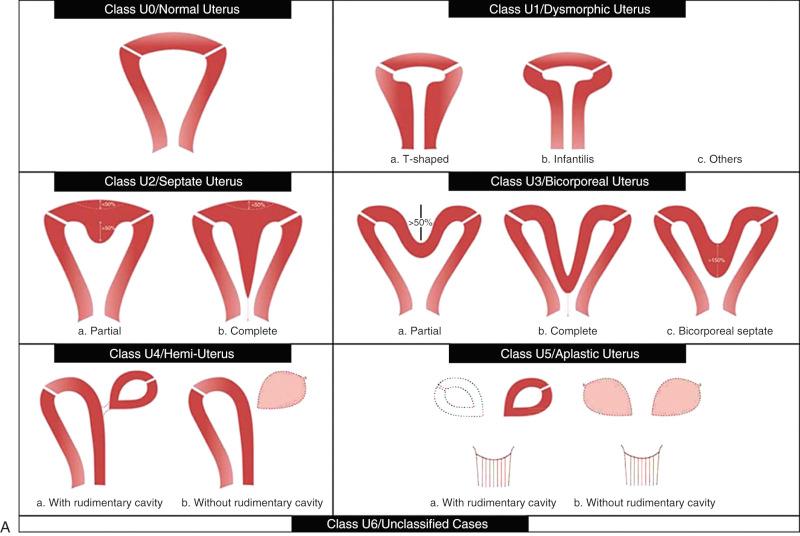
In a review of the clinical implications of uterine anomalies, the frequency of anomalies by type was septate (35%), bicornuate (26%), arcuate (18%), unicornuate (10%), didelphys (8%), and agenesis (3%). Of the developmental defects, there are three categories to consider: agenesis, lateral fusion defects, and vertical fusion defects. Historically, the workup of these anomalies was quite cumbersome and invasive, typically involving hysterosalpingography often with concomitant hysteroscopy, and laparoscopy under general anesthesia. More recently, MRI has become the standard diagnostic imaging modality, obviating the need for these invasive tests. With the refinement and availability of three-dimensional (3D) sonography ( Fig. 37-6 ), some groups have argued that this may become the new gold standard, offering excellent diagnostic imaging at lower cost and with less discomfort than MRI.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here