Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Magnetic resonance imaging (MRI) is a problem-solving tool and has greater accuracy and specificity for characterization of gynecologic masses than sonography or computed tomography (CT), but should generally be performed after pelvic sonography.
High resolutionT2-weighted sequences are the mainstay images for evaluation of nonobstetric gynecologic disorders.
T1-weighted imaging must be performed with and without fat suppression if characterization of fat or blood products is required.
The uterine corpus is best assessed in the parasagittal plane.
The cervix is best assessed in the axial plane.
MRI is the method of choice for evaluation of congenital uterine anomalies, including associated renal anomalies.
Water-based gel instilled into the vagina is helpful in cervical and vaginal cancer assessment.
Gadolinium is helpful in defining the extent and vascularity of tumors.
Many tumors demonstrate restricted diffusion.
Staging of gynecologic malignancy is based on the International Federation of Gynecology and Obstetrics (FIGO) system, and cross-sectional imaging is helpful in preoperative planning.
This chapter describes the main indications for MRI in the evaluation of nonobstetric gynecologic disorders. In the first two sections, normal anatomy of the female pelvis and common congenital anomalies are discussed. In subsequent sections, the use of MRI in the setting of common benign diseases, namely leiomyomas, adenomyosis, and endometriosis is outlined. Finally, the role of MRI in patients with malignant neoplasms of the reproductive organs is discussed. The main clinical and epidemiologic aspects of gynecologic disease are presented, in addition to the imaging features, in order to emphasize a practical clinical approach to patient management.
Although a detailed discussion of imaging techniques and protocols used in MRI is beyond the scope of this chapter, some of the most important basic concepts with regard to MRI techniques are included to aid in interpretation of images presented herein, targeting those readers unfamiliar with MRI.
T2-weighted images provide the foundation for MRI of the female pelvis. These images are used for evaluation of normal anatomy and detection of most uterine and adnexal abnormalities. T1-weighted images, especially when used in conjunction with fat suppression, are helpful in characterizing the content of adnexal lesions, namely in the identification of blood and fat. When used after the administration of intravenous gadolinium, T1-weighted images also assist in the characterization of some benign and malignant tumors. As a general rule, on T1-weighted images, fat-containing lesions are bright (high signal intensity), whereas water, such as urine in the bladder, is dark (low signal intensity). However, water is bright on T2-weighted images. Therefore, tissues with higher amounts of water, such as tumors and cysts, have high signal intensity on T2-weighted images. Water-based gel instilled into the vagina can be used to distend the vaginal lumen and outline the cervical contour, but this technique is not widely used. Gadolinium-based contrast agents are most commonly used as intravenous contrast media in MRI. Tissues that are infused with gadolinium increase in signal intensity on T1-weighted images when compared with images acquired before contrast administration. Hence, gadolinium is used to increase the contrast between normal and abnormal tissues in the body and to detect vascularity of tissues. For instance, many neoplastic processes enhance more avidly than adjacent normal tissues and thus become more easily visible. Newer techniques such as dynamic multiphase contrast-enhanced MRI (DCE-MRI) and diffusion-weighted imaging (DWI) provide functional information. In DCE-MRI, images are acquired at multiple times following injection of contrast agent, allowing assessment of tissue vascularity and enhancement patterns. DWI does not use intravenous contrast, but displays contrast between tissues based on different rates of diffusion of water molecules. Many malignant tumors are bright on DWI.
Although it is not within the scope of this chapter to fully discuss the normal anatomy of the female pelvis, a few words regarding specific features on MRI are important. A basic concept that must be remembered is that the patient's hormonal status affects the imaging features of the female reproductive organs, irrespective of the imaging modality.
The uterus typically measures from 6 to 9 cm in length in women of reproductive age; the cervix accounts for approximately 30% to 50% of the total uterine length in this age group, but is proportionally larger before the menarche. Uterine zonal anatomy is best visualized using T2-weighted images, typically acquired in the axial and sagittal planes, and may be described by considering two separate regions, the cervix and the uterine body.
The cervical anatomy is divided into three zones on T2-weighted sequences: the endocervical mucosa centrally, which demonstrates high signal intensity as a result of the presence of mucus within glands; the cervical stroma, which demonstrates low signal intensity owing to the presence of fibrous connective tissue; and the peripherally located smooth muscle, which demonstrates intermediate signal intensity ( Fig. 36-1 ). Varying amounts of mucus may be seen within the endocervical canal, which has a very high signal intensity similar to that of fluid.
The zonal anatomy of the body of the uterus also consists of three distinct regions on T2-weighted sequences: centrally, the endometrium demonstrates very high signal intensity; subjacent to the endometrium, the junctional zone, which represents the innermost layer of the myometrium, demonstrates low signal intensity; and the outer myometrium, which demonstrates intermediate signal intensity ( Fig. 36-2 ). At its inferior aspect, the junctional zone is continuous with the low signal intensity fibrous cervical stroma.
Identification of the junctional zone is extremely important when evaluating the uterine magnetic resonance zonal anatomy. Studies have shown that the appearance of the zonal anatomy on MRI is influenced by female hormones. Normally, the junctional zone should not measure more than 11 mm in thickness in women of reproductive age. In postmenopausal women, women taking oral contraceptives, or in girls before menarche, the zonal anatomy is frequently indistinct and the junctional zone may be very thin.
The MRI appearance of the endometrium is also hormonally influenced and varies with the menstrual cycle. The endometrium becomes progressively thicker between the early follicular (proliferative) phase and ovulation, increasing from 1 to 3 mm in thickness to an average of 8 to 9 mm. The endometrium should not measure more than 15 mm in thickness in women of menstrual age, and typically it measures 11 mm or less in postmenopausal women who are not on hormonal replacement therapy. The endometrium is highest in signal intensity during the luteal (secretory) phase. It is imperative to recognize that the evaluation of endometrium thickness using T2-weighted images may result in overestimation because fluid within the endometrial cavity is also high in signal intensity on T2-weighted sequences ( Fig. 36-3 ).
Unlike the uterine corpus, the cervical zonal anatomy does not demonstrate significant changes during the menstrual cycle. In addition, because the cervix is composed largely of fibrous elastic tissue, enhancement of the cervix following the administration of intravenous gadolinium differs from enhancement of the uterine corpus. The uterine corpus is a very vascular structure when compared to the cervix and enhances earlier and more avidly than the cervix ( Fig. 36-4 ). This is important because this difference in enhancement pattern may give the appearance of a pseudomass and lead to a misdiagnosis of cervical cancer.
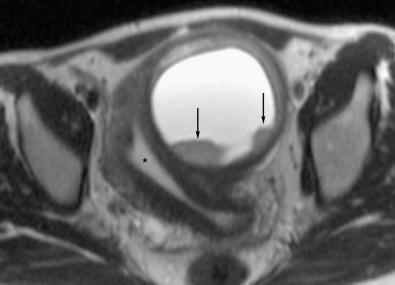
The normal ovaries demonstrate homogeneous intermediate T1-weighted signal intensity; however, on T2-weighted sequences, an outer high signal intensity cortex and a hypointense central medulla will be observed. The ovaries measure approximately 2 × 2 × 3 cm; however, their size fluctuates according to hormonal status, largely because of follicle production and enlargement during the menstrual cycle. The ovaries are most readily identified in women of reproductive age by the presence of such follicles, which appear as small simple cysts of high signal intensity on T2-weighted sequences and low signal intensity on T1-weighted sequences ( Fig. 36-5 ). Primordial follicles are usually smaller, measuring up to 9 mm in diameter, whereas stimulated graafian follicles may reach up to 3 to 5 cm. Other features of these physiologic cysts seen on T2-weighted sequences include imperceptible or thin walls (less than 3 mm) and absence of mural nodules (see Fig. 36-5 ). The number of ovarian follicles decreases following menopause in women who are not taking hormonal replacement therapy. However, simple ovarian cysts are a common incidental finding in postmenopausal women, seen in 14% of women over 55 years of age, and may resolve or remain stable. Ovarian stroma enhances after intravenous contrast agent administration and the use of fat-suppressed sequences helps to identify the ovaries when follicles are not visible. The normal fallopian tubes are not visualized on MRI.
MRI is the imaging method of choice for evaluation of congenital anomalies of the female reproductive tract. Advantages of MRI include noninvasiveness, lack of ionizing radiation, multiplanar capability enabling visualization of the fundal contour of the uterus, and excellent soft tissue characterization. The use of MRI may reduce the number of invasive procedures and related costs by guiding management decisions.
The müllerian ducts are paired embryologic structures that normally fuse between the 6th and 11th weeks of gestation, forming the uterus, fallopian tubes, cervix, and most of the upper vagina. However, in 0.1% to 10.0% of the general population, either fusion fails to occur or the ducts do not develop normally, resulting in one of the multiple types of anomalies. Although müllerian duct anomalies may be asymptomatic depending upon the exact type, they may be associated with primary amenorrhea, infertility, obstetric complications, and endometriosis. It is estimated that as many as 25% of women who present with infertility and miscarriage have müllerian duct anomalies. In addition, 30% to 50% of these women have concurrent renal anomalies, which include renal agenesis, ectopia, fusion, malrotation, and duplication. Patients suspected of having müllerian duct anomalies are often initially investigated with transvaginal sonography, because it is widely available, safe, and of relatively low cost. Although MRI is considered the reference standard for the evaluation of müllerian duct anomalies with a diagnostic accuracy of almost 100%, it is frequently reserved for indeterminate cases or cases in which further information is needed. T2-weighted sequences are the most useful because identification of the zonal anatomy is necessary for complete evaluation and analysis. In addition, the study must include an oblique coronal and axial plane to ensure adequate visualization of the uterine fundal contour.
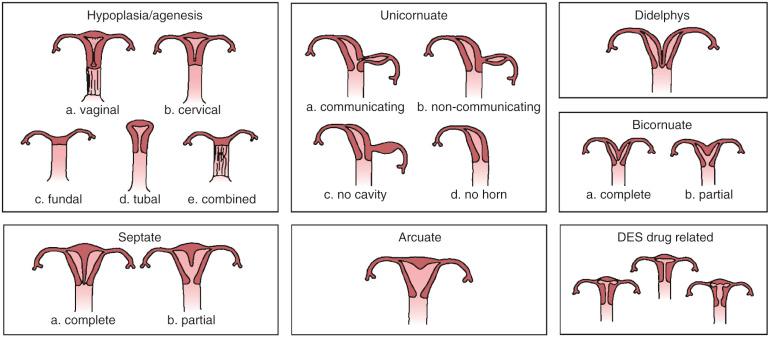
Although there are many different classifications of müllerian duct anomalies, the American Society for Reproductive Medicine classification is perhaps the most widely used and the best known ( Fig. 36-6 ).
The anomalies within this group result from bilateral nondevelopment or arrested development of the müllerian ducts. Agenesis of the upper vagina and uterus is the most common anomaly in this group and part of the spectrum of the Mayer-Rokitansky-Küster-Hauser syndrome. Patients with this syndrome may present with an atrophic uterus, however, and vaginal abnormalities can range from hypoplasia to agenesis. Urinary system malformations are sometimes associated with the Mayer-Rokitansky-Küster-Hauser syndrome. The second most common anomaly in this class is segmental vaginal agenesis. Isolated agenesis or hypoplasia of the uterus is very rare. In complete uterine agenesis, MRI demonstrates only a short blind-ending vagina, whereas in cases of uterine hypoplasia, the uterus is small and the intercornual diameter of the endometrial cavity is reduced, measuring less than 2.0 cm.
A unicornuate uterus is the consequence of complete arrest or partial development of one müllerian duct in utero. In 90% of cases, partial development of the duct occurs, with an ensuing rudimentary horn, which may or may not contain functioning endometrium. The rudimentary horn may be obstructed or may communicate with the main uterine cavity. Clinical associations include very high rates of spontaneous miscarriage, obstetric complications, and endometriosis. A unicornuate uterus will have normal zonal anatomy and has a characteristic banana-shaped configuration. A rudimentary horn can be seen as an adjacent soft tissue mass and may be distinguished from a tumor by virtue of signal intensity characteristics that are similar to myometrium on T2-weighted images. An obstructed (noncommunicating) rudimentary horn may become enlarged as a result of distention from blood products, identified as high signal intensity central material on T1-weighted sequences.
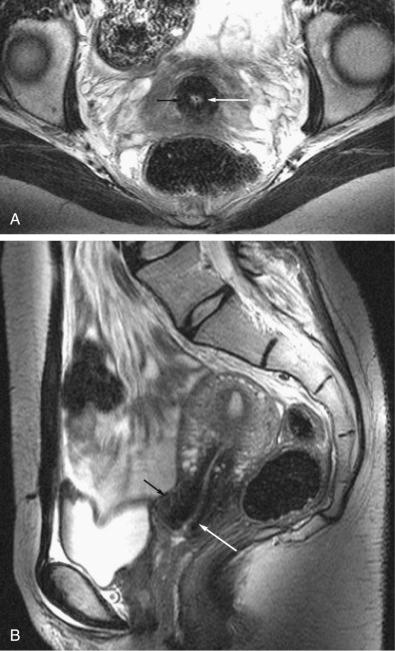
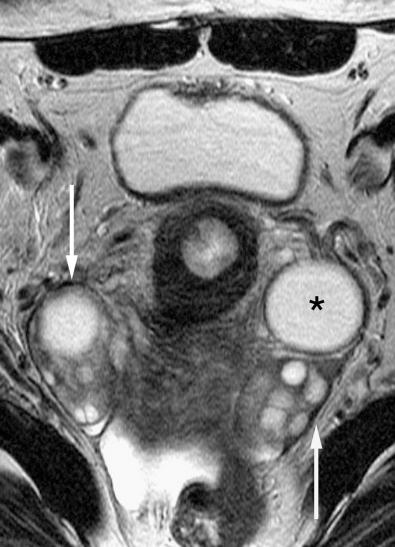
Uterus didelphys arises through complete failure of müllerian duct fusion in utero and is characterized by the presence of two separate uteri and cervices with a vertical septum in the upper vagina. Very rarely, two completely separated vaginas and vaginal orifices may be present. Patients are usually asymptomatic, but hematometrocolpos may occur in the presence of an obstructing transverse hemivaginal septum. Clinical complications are similar to those associated with a unicornuate uterus. MRI may be used to readily diagnose uterus didelphys by demonstration of two widely separated uterine horns and two cervices ( Fig. 36-7 ). The zonal anatomy is preserved. Vaginal septa may not always be identified with MRI, and physical examination may be necessary for confirmation and differentiation from a bicornuate bicollis uterus.

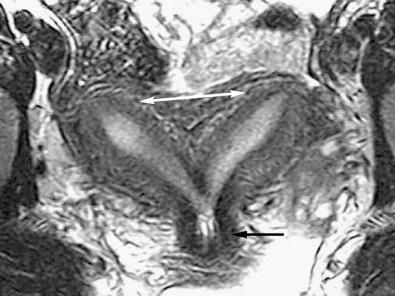
This anomaly is the result of partial failure of fusion of the müllerian ducts. It is characterized by an increased intercornual distance, reportedly measuring wider than 4 cm; a concave external contour of the fundus, measuring more than 1 cm in depth; and a fibrous-muscular septum bisecting the endometrial cavity. The septum may be incomplete, partially dividing the uterine cavity (bicornuate unicollis [ Fig. 36-8 ]), or complete, extending all the way to the external cervical os (bicornuate bicollis). The vagina develops normally. Images obtained in the oblique coronal plane, along the long axis of the uterus, are useful in assessing the fundal contour. The dividing septum often exhibits signal characteristics similar to myometrium, but may be of low signal intensity inferiorly when fibrous tissue is present.
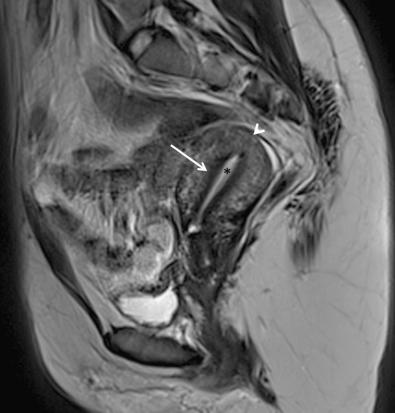
Septate uterus is the most common müllerian duct anomaly and is thought to result from failure of resorption of a fibrous septum in later stages of development. The result of such failure of resorption is a characteristically small endometrial cavity with a dividing septum, which may be partial or may extend to the external cervical os. Reproductive complications are greatest in this class of müllerian duct anomaly and are attributed to difficulties of implantation. Identification of a convex, flat, or minimally indented fundal contour without a fundal cleft on MRI obtained in the coronal plane ( Fig. 36-9 ) is decisive in distinguishing a septate from a bicornuate uterus. Other diagnostic MRI features include an intercornual distance of less than 4 cm (i.e., not increased) and a thin, dividing, often fibrous septum typically of low T1- and T2-weighted signal intensity, although the septum may have a signal intensity similar to that of myometrium if myometrial smooth muscle is the primary component of the septum. The septum may be partial or complete.

This anomaly is recognized by mild indentation of the myometrium into the fundal aspect of the endometrium, attributed to minimally incomplete resorption of the uterovaginal septum. It is classified separately because it is a benign variant without clinical significance. On MRI, the arcuate uterus is typically of normal size with a single endometrial cavity that is minimally indented superiorly by the small nonresorbed septal remnant and may be associated with a small fundal cleft less than 1.0 cm in depth.
Diethylstilbestrol is a synthetic estrogen that was historically prescribed to prevent miscarriages until 1971. It is estimated that approximately two thirds of patients exposed to this drug while in utero have uterine anomalies. The most common of these anomalies is the classic hypoplastic T-shaped uterus, but other deformities of the uterine horns and endometrial cavity have been reported.
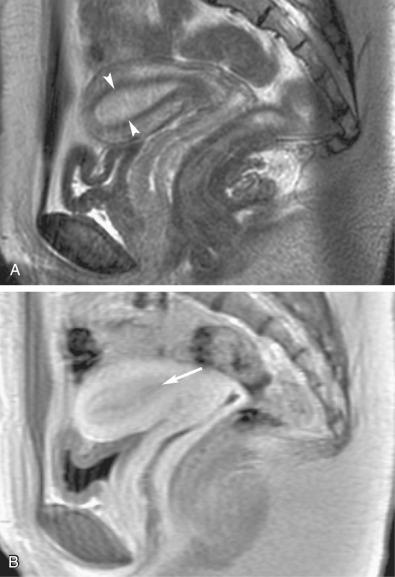
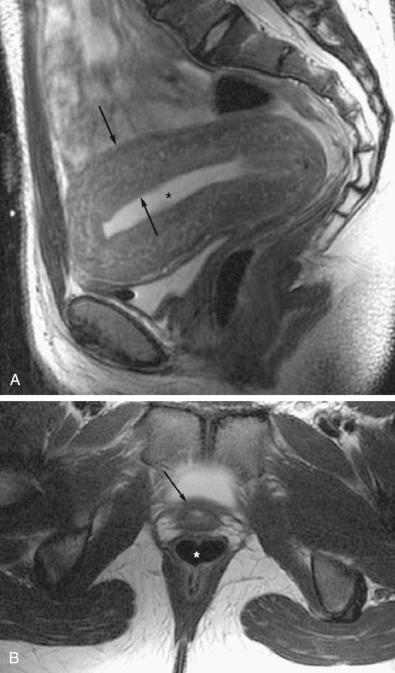
The lower third of the vagina originates from the urogenital sinus rather than the müllerian ducts and is developmentally distinct. Absence of the distal or lower third of the vagina or the presence of a transverse membrane (mimicking an imperforate hymen) results from failure of urogenital sinus development. In both eventualities, the vaginal obstruction causes the vagina and uterus to distend with fluid, referred to as hematometrocolpos when blood products are identified. The upper vagina demonstrates very thin walls, whereas the uterus may have either thin or thick myometrium ( Fig. 36-10 ). Hematometrocolpos is characterized as a heterogeneous collection with high T1- and intermediate or low T2-weighted signal intensity.
The ovaries arise from primitive germ cells that migrate to the embryonic gonadal ridge and subsequently descend into the pelvis. Congenital anomalies of the ovaries are typically associated with chromosomal disorders and include gonadal dysgenesis, commonly occurring with Turner syndrome (45,X karyotype) and Turner syndrome mosaicism (45,X/46XX karyotype). The ovaries of patients with gonadal dysgenesis are absent or seen as fibrous streaks. Fat-suppressed T2-weighted and gadolinium-enhanced T1-weighted sequences are most helpful in the identification of the ovaries.
Leiomyomas are benign tumors arising from uterine smooth muscle cells and occur in more than 80% of African-American women and in approximately 70% of Caucasian women by age 50 years. African-American women are diagnosed with leiomyomas at earlier ages, are more likely to be symptomatic, and are more likely to undergo myomectomies and hysterectomies compared to Caucasian women. Leiomyomas have a significant impact on public health, accounting for at least one third of the 600,000 hysterectomies performed each year in the United States.
Most patients with leiomyomas are asymptomatic. Clinical symptoms associated with leiomyomas include dysfunctional uterine bleeding, pelvic pressure, and pelvic pain. In addition, there is an association with impaired reproductive function, which may be related to impaired implantation, tubal obstruction, and an increased rate of miscarriage as well as preterm labor. Approximately 90% of leiomyomas occur in the uterus, whereas 5% to 10% are cervical in location. Leiomyomas can enlarge during pregnancy, and cervical leiomyomas may cause dystocia. A minority of leiomyomas occur in the round and broad ligaments ( Fig. 36-11 ) or adnexa.
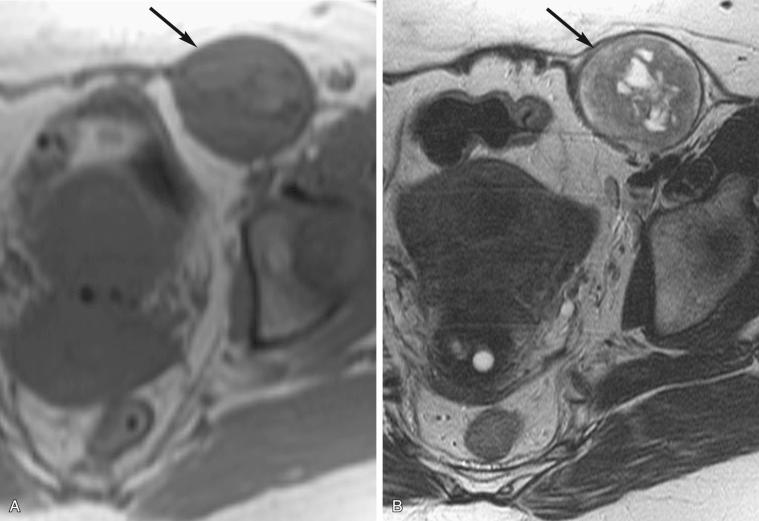
Location of the leiomyoma often predicates the symptoms. Uterine leiomyomas are classified as submucosal, intramural, or subserosal ( Fig. 36-12 ). Approximately 5% of leiomyomas are submucosal in location ( Fig. 36-13 ). Submucosal leiomyomas typically present with menometrorrhagia. In addition, a submucosal leiomyoma is more likely to be associated with infertility, dysfunctional uterine bleeding, dysmenorrhea, and anemia. Submucosal leiomyomas are often effectively treated with hysteroscopic resection, depending upon size and intracavitary extent of the mass. Submucosal leiomyomas are distinguished from large intramural leiomyomas based on identification of the lesion's epicenter within the endometrial cavity rather than within the myometrium, and less than 180-degree encirclement by surrounding myometrium.
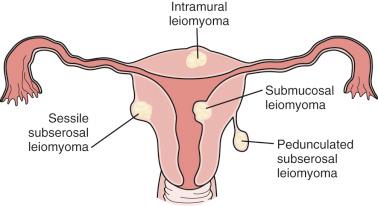

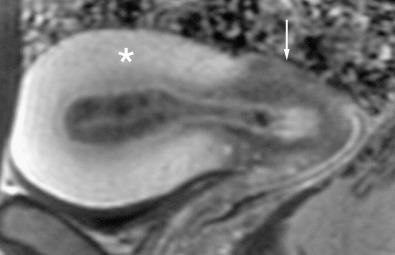
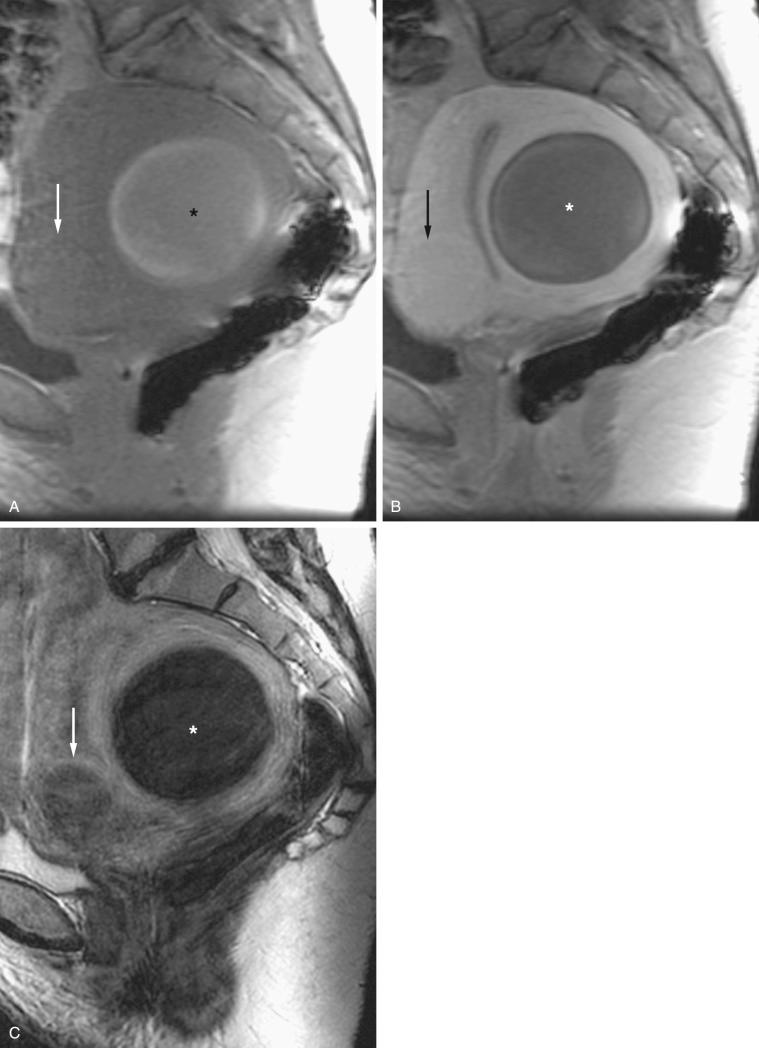
Subserosal leiomyomas account for approximately 10% to 20% of uterine leiomyomas, are located just under the uterine serosa, and may be pedunculated or sessile ( Figs. 36-13 and 36-14 ). Symptoms are associated with large size owing to mass effect or torsion of a pedunculated lesion. The bridging vascular sign (vessels originating from the uterus and feeding a pelvic mass) is seen in approximately 77% of exophytic leiomyomas and is helpful in differentiating these tumors from solid adnexal masses. Conversely, an ovarian vascular pedicle (identified by the presence of a gonadal vein) may be helpful in establishing that a mass is ovarian in origin. A pedicle is seen in 92% of ovarian masses and 13% of pedunculated subserosal leiomyomas.
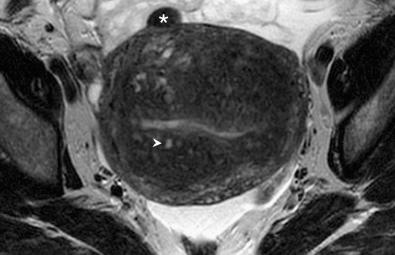
The pathophysiology of leiomyomas is unknown; however, genetic predisposition and hormonal status are involved in tumor development and growth. Responsiveness of leiomyomas to hormonal stimulation frequently results in enlargement during pregnancy and involution following menopause. Various types of benign degeneration are common, particularly in large leiomyomas, and include hyaline (most common and present in at least 60% of leiomyomas), cystic, myxoid, fatty, and hemorrhagic degeneration ( Fig. 36-15 ). Imaging-based differentiation between the types of degeneration is usually not possible; however, certain features may favor one or another type. Degeneration within a leiomyoma may make the sonographic diagnosis difficult as a degenerated leiomyoma may have cystic components and, thus, may mimic the sonographic appearance of a complex ovarian mass. In such cases, MRI may be used for diagnosis.
Knowledge of atypical locations and presentations, such as benign metastasizing leiomyomas, intravenous leiomyomas, diffuse leiomyomatosis, and peritoneal disseminated leiomyomatosis, is important. Although these uncommon presentations may suggest a malignant process, they are essentially a variation in the growth pattern of this benign lesion. Uterine leiomyosarcomas have been reported to occur in association with leiomyomas. However, genetic studies suggest that these are two different entities arising from separate pathways. Malignant degeneration of a benign leiomyoma into a leiomyosarcoma is considered by most pathologists to be extremely rare, if it occurs at all. Sometimes, the distinction between a leiomyoma and a leiomyosarcoma cannot be reliably made based on MRI characteristics of the primary lesion; however, rapid growth, irregular borders, evidence of extrauterine extension, lymphadenopathy, and metastases are, to different degrees, suggestive of malignancy ( Fig. 36-16 ).
The preferred treatment for leiomyomas depends upon their size and location, as well as clinical presentation. The most common therapeutic options are hysterectomy, myomectomy (transabdominal, laparoscopic, or hysteroscopic), myolysis, and uterine artery embolization (UAE). Hysterectomy is usually performed in women who have completed childbearing and do not wish to preserve the uterus. Myomectomy is often the choice for those patients who wish to preserve the uterus. In these cases, an abdominal approach is used for multiple large leiomyomas; the laparoscopic approach is appropriate for resection of subserosal and pedunculated lesions, whereas the hysteroscopic technique is preferred for patients with submucosal lesions that are greater than 50% intracavitary. UAE is a newer, safe, and effective technique with the potential to become the treatment of choice for symptomatic uterine leiomyomas. Contraindications to UAE include active pelvic infection, renal insufficiency, and contrast agent allergy. The reported principal advantage of UAE in appropriate candidates is lower morbidity compared to more invasive surgical techniques.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here