Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Although the incidence of rheumatic heart diseases has decreased, mitral stenosis (MS) remains prevalent in developed countries. It is common and underdiagnosed in developing countries.
Calcific MS is the consequence of extensive mitral annular calcification, the prevalence of which increases markedly with age.
Clinical assessment is paramount to detect MS in asymptomatic patients and to evaluate symptoms.
Planimetry using bidimensional echocardiography is the reference measurement for the mitral valve area (MVA) in patients with rheumatic MS.
Intervention is needed in symptomatic patients who have rheumatic MS with an MVA smaller than 1.5 cm 2 .
Balloon mitral commissurotomy (BMC) can be considered for selected asymptomatic patients who have rheumatic MS with an MVA of less than 1.5 cm 2 , particularly those who have a high risk of thromboembolism.
The choice between BMC and surgery should be individualized and based on valve anatomy and other clinical and echocardiographic characteristics.
Decision making for interventions is difficult for calcific MS because of the technical difficulties of surgery and the frequently high-risk profile of patients. Transcatheter mitral valve replacement may be an alternative for selected patients, but it carries significant early morbidity and mortality, and long-term results are lacking.
Mitral stenosis (MS) remains prevalent despite the decreased incidence of rheumatic heart disease. The main purpose of investigation of rheumatic MS is to determine the optimal timing of intervention and the most appropriate treatment: balloon mitral commissurotomy (BMC) or surgery. Large series reporting long-term follow-up after BMC have improved the level of evidence for interventional decision making, as attested by contemporary guidelines.
In patients with calcific mitral stenosis, decision making must also consider the technical difficulties of surgery and the frequently high-risk profile of elderly patients. Transcatheter mitral valve replacement offers an alternative for selected patients, but it carries significant early morbidity and mortality, and long-term results are lacking.
MS is the least common left-sided native valve disease in developed countries, accounting for 9% of single, moderate or severe native valve diseases in Europe in 2001. The overall prevalence of MS, without assessment of cause, was estimated at 0.1% in the only large population-based study on valvular diseases comprising systematic echocardiographic examinations. Unlike other valvular diseases, the most frequent cause of MS remains rheumatic heart disease, which is now rare in developed countries.
Calcific MS is the consequence of mitral annular calcification (MAC) extending to the leaflets. MAC is diagnosed by cardiac computed tomography (CT) in approximately 10% of unselected patients. Its prevalence increases with age and is greater than 25% after the age of 75 years (MESA study). In the Euro Heart Survey, the percentage of calcific causes increased progressively with age. MAC is favored by cardiovascular risk factors and reduced renal function. , Although MAC is common, it seldom causes significant hemodynamic impairment. Mitral regurgitation (MR) is more common than MS, which is encountered in less than 10% of patients with MAC. ,
In developing countries, the estimated prevalence of rheumatic heart disease is between 1 and 10 cases per 1000 of school-age children according to clinical screening and between 20 and 30 cases per 1000 of school-age children by systematic echocardiographic screening. Most valvular disease is of rheumatic origin and involves mainly young adults (mean age, 30–40 years). , Pure MS accounts for 5% to 10% of valvular disease in patients between 20 and 50 years of age, and MS with MR accounts for 20% to 30%.
Intermediate patterns are observed in emerging countries. In a 2009 Turkish survey, rheumatic heart disease accounted for 46% of all valve diseases, followed by calcific causes in 29%.
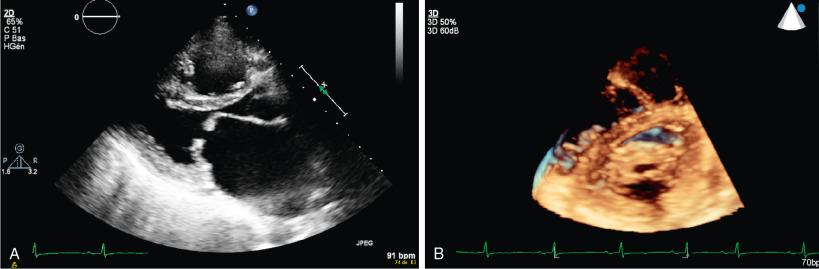
The main mechanism of rheumatic MS is commissural fusion ( Fig. 16.1 ). Posterior leaflet thickening and restriction are almost constant features. Thickening and rigidity of the anterior leaflet or subvalvular apparatus can also contribute to stenosis. Commissural fusion explains why the area of the mitral orifice is relatively constant in severe MS, whereas it may vary according to flow conditions after the commissures have been opened by BMC.
Degenerative MAC results from an active remodeling process favored by cardiovascular risk factors, increased mitral valve stress, and disorders of calcium-phosphorus metabolism. , It is frequently associated with atherosclerosis and calcific aortic stenosis. , The main mechanism of calcific MS is reduced anterior leaflet mobility due to rigidity without commissural fusion. ,
Other causes are rare. Congenital MS is mainly the consequence of abnormalities of the subvalvular apparatus. Inflammatory diseases (e.g., systemic lupus), infiltrative diseases, carcinoid heart disease, and drug-induced valve diseases are characterized by a predominance of leaflet thickening and restriction, but commissures are seldom fused.
The increase in diastolic mitral pressure gradient depends on the mitral valve area (MVA) and on other factors such as transvalvular flow and heart rate. Severe MS may therefore be associated with a low gradient in patients with low cardiac output, particularly those who have chronic atrial fibrillation (AF).
Chronic left atrial (LA) pressure overload due to mitral gradient leads to enlargement of the LA, with important interpatient variations. LA enlargement and wall fibrosis favor the occurrence of AF.
The severity of blood stasis can be assessed with Doppler echocardiography from the intensity of LA spontaneous contrast and the decrease of flow velocities in the LA appendage in patients in sinus rhythm. Blood stasis and LA appendage flow velocities are considerably impaired when AF occurs. The LA appendage is the most frequent location of LA thrombus.
Postcapillary pulmonary hypertension is the passive consequence of increased LA pressure. There may also be a component of precapillary pulmonary hypertension due to an increase in pulmonary vascular resistance, which determines a gradient of 7 mmHg or greater between diastolic pulmonary artery pressure (PAP) and pulmonary artery wedge pressure.
Increased pulmonary vascular resistance involves endothelium-dependent vasoconstriction, which is reversible under inhaled nitric oxide, and structural changes of the pulmonary arterial wall. Structural changes initially consist of intimal and medial thickening in muscular arteries and arterioles, which may be reversible with a decrease in PAP. More severe lesions include fibrinoid necrosis and arteritis, loss of smooth muscle cell nuclei, fibrin deposition in the arterial wall, and inflammatory cells. Plexiform lesion is the hallmark of end-stage, irreversible pulmonary hypertension and accounts for persistently elevated PAP after intervention for MS. There is a wide range in PAP for any degree of MS because PAP depends on MVA and gradient and on left ventricular (LV) end-diastolic pressure, chronic pulmonary disease, and net atrioventricular compliance. ,
Chronic pulmonary hypertension leads to right ventricular (RV) hypertrophy, dilation, and then reduced ejection fraction. This process may be exacerbated by significant tricuspid regurgitation from rheumatic involvement of the tricuspid valve or annular dilation due to RV enlargement. Although pulmonary hypertension presumably is the cause of right heart dysfunction, there is a poor correlation between pulmonary pressures and RV failure in patients with MS.
LV size is usually normal or moderately reduced in MS. The main consequence of MS on the LV is a prolongation of early diastolic filling and an increased contribution of LA contraction. AF further alters diastolic filling. LV filling may also be impaired by RV pressure or volume overload determining abnormal septal motion.
Although LV contractility typically is normal in isolated MS, forward stroke volume may be reduced due to low filling volumes across the stenotic mitral valve. LV ejection fraction is impaired in 5% to 10% of patients in the absence of other valve or coronary artery disease. This does not seem to be explained by abnormal loading conditions because LV dysfunction typically persists after the relief of MS.
Hemodynamic changes during exercise provide additional insights into the many factors interacting with the severity of the stenosis to determine its repercussions. The increase in transmitral gradient during exercise is the consequence of shortening of the diastolic filling period, and it determines an upstream increase in PAP. However, changes in mitral gradient and PAP vary greatly for a given degree of stenosis. This heterogeneity may be explained by differences in the evolution of stroke volume during exercise and by differences in atrioventricular compliance, which depends mostly on LA compliance. , Besides valvular function, lung function, chronotropic incompetence, stroke volume reserve, and peripheral factors contribute to impaired exercise tolerance.
Increased stroke volume during exercise is associated with an increase in MVA during exercise, which is observed in patients who have a moderate impairment of valve anatomy. In patients with severe impairment of valve anatomy, stroke volume does not increase or may even decrease during exercise. Besides valvular function, net atrioventricular compliance is a strong determinant of LA pressure and PAP at rest and during exercise. , ,
Dyspnea is the most frequent symptom of MS, and it has a prognostic value. It may be difficult to assess given the progressive course of the disease and in elderly patients with calcific MS. Paroxysmal dyspnea, cough, or hemoptysis should be looked for.
Patients sometimes complain more about fatigue than dyspnea, particularly elderly patients and those who have advanced heart disease with chronic AF. Asthenia and abdominal pain are suspicious for right heart failure.
Complications such as AF or embolic events may reveal MS in previously asymptomatic patients. Pregnancy is a common cause of decompensation of previously well-tolerated MS, because the increase in cardiac output and tachycardia causes a sharp increase in the mitral gradient and PAP during the second trimester. The search for comorbidity is important in older patients, who account for a growing portion of patients with rheumatic or calcific MS in developed countries. , ,
Auscultation reveals a loud first heart sound and an opening snap in early diastole just after the second heart sound, followed by a holodiastolic rumbling murmur that decreases in intensity with time and increases in end-diastole in patients in sinus rhythm ( Fig. 16.2 ). Careful auscultation is needed because the murmur is often difficult to identify.
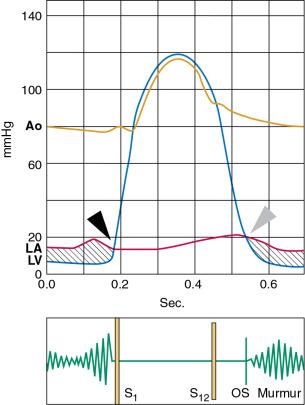
A loud murmur with a thrill suggests severe stenosis. However, a low-intensity murmur does not exclude severe stenosis in a patient with low cardiac output. The duration of the interval between the second aortic sound and the opening snap is shortened in severe stenosis. The intensity of the first sound and of the opening snap may be diminished in cases of extensive calcification that limits leaflet motion.
Auscultation should search for a holosystolic murmur at the apex, which suggests combined MR and MS. The holosystolic murmur of tricuspid regurgitation is usually located at the xiphoid or near the apex and increases with inspiration. It is important to pay attention even to a low-intensity mid-systolic murmur attesting to associated aortic stenosis, the severity of which tends to be underestimated when combined with MS. A diastolic murmur at the left sternal border is more likely to be the consequence of aortic than pulmonic regurgitation. The second pulmonary sound is louder in cases of pulmonary hypertension. Auscultation is also the first means of detecting arrhythmias, which should be confirmed by electrocardiography.
Clinical signs of left-sided heart failure are found in patients with severe symptoms. Signs of right heart failure are observed in patients with severe and often long-standing disease. Hepatomegaly may be expansive in cases of severe tricuspid regurgitation.
LA enlargement is characterized by LA double density and prominence of the LA appendage on chest radiograms. The pulmonary artery trunk and branches are often dilated. Heart size is initially normal but is enlarged in severe chronic MS with RV and right atrial enlargement. Interstitial edema is often seen even in patients without clinical signs of heart failure. Alveolar edema is a sign of acute hemodynamic decompensation. Transverse chest radiography is useful to detect RV enlargement, mild pleural effusion, and MAC.
LA enlargement is the only electrocardiographic abnormality at an early stage. RA and RV enlargement with right axis deviation and right bundle branch block are observed in more advanced disease. Electrocardiography plays a major role in the detection of atrial arrhythmias including frequent atrial premature beats, AF, and less frequently, atrial flutter or atrial tachycardia.
Echocardiography is the cornerstone for confirming the diagnosis of MS, evaluating its cause, determining the severity and consequences of valve lesions, and assessing valve anatomy and associated diseases.
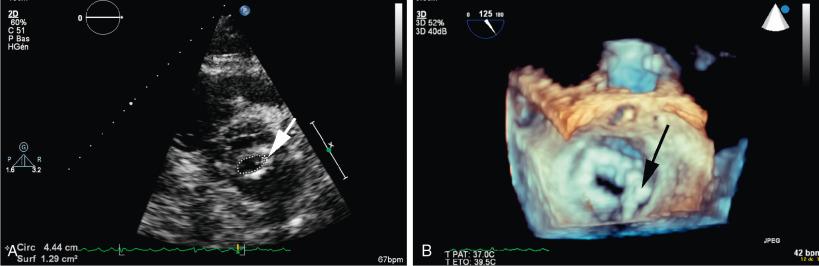
Planimetry using the parasternal short-axis view is the reference measurement of MVA because it directly measures the valve area independent of loading conditions and associated heart diseases. Technical expertise is needed to scan the mitral valve apparatus to position the measurement plane on the leaflet tip. This may be facilitated with the use of three-dimensional (3D) echocardiography, which improves accuracy and reproducibility. , Planimetry is also useful during BMC to monitor the procedure and immediately after BMC, for which it is the most reliable technique.
Planimetry may be difficult or not feasible in cases of irregular orifice or severe calcification and in patients with poor echogenicity. Mitral orifice planimetry is particularly difficult to perform and lacks reliability in patients with degenerative MS due to the extent of calcification and the deformation of the mitral orifice. Limited data suggest that planimetry using 3D echocardiography has good concordance with the results obtained from use of the continuity equation.
The parasternal short-axis view also assesses commissural fusion; accuracy is higher with 3D rather than two-dimensional (2D) echocardiography. This is important for differentiating rheumatic from calcific MS and for determining the feasibility of BMC. Assessment of the commissural opening provides an additional indication of the efficacy of BMC during and after the procedure and during late follow-up.
The pressure half-time method is easier to perform and is therefore widely used, but it may be misleading in cases of aortic regurgitation, abnormal compliance of cardiac chambers, and immediately after BMC. The validity of the pressure half-time method is questionable for patients with calcific MS because LV compliance is frequently impaired due to patient age and hypertension.
Use of the continuity equation is not valid in cases of associated significant MR or aortic regurgitation. Its accuracy and reproducibility are limited due to the number of measurements involved.
Assessment of the proximal isovelocity surface area is technically demanding.
Mean mitral gradient, as assessed by pulsed or continuous-wave Doppler, depends greatly on flow conditions: cardiac output, heart rate, and associated MR. Its value should be consistent with the MVA, and it has prognostic value after BMC. Despite its flow dependence, the mean gradient is useful in patients with calcific MS because of limitations of the methods used to assess valve area. Severe MS is likely if the mean gradient is greater than 10 mmHg.
The consistency of results obtained by planimetry, the pressure half-time method, and mitral gradient should always be checked, keeping in mind the limitations of the various measurements. , The continuity equation and proximal isovelocity surface area methods are not used routinely in rheumatic MS but may be useful when other methods lead to uncertain or discordant findings ( Table 16.1 ). Given the limitations of planimetry and the pressure half-time method, the continuity equation is useful for assessment of calcific MS.
| Measurement | Method | Advantages | Disadvantages | Alternative Methods |
|---|---|---|---|---|
| Valve area (cm 2 ) | Planimetry on 2D/3D parasternal short-axis view | Direct measurement, independent of flow conditions; reference method for rheumatic MS | Experience required; not feasible if there is severe valve deformity or a poor acoustic window | MSCT, CMR, Gorlin formula |
| Pressure half-time using CW Doppler | Easy to obtain | Dependence on other factors (regurgitations, chamber compliance, diastolic function) | — | |
| Continuity equation | Independent of flow conditions; recommended for calcific MS | Errors of measurement (multiple variables); not valid in cases of significant regurgitation | — | |
| Proximal isovelocity surface | Independent of flow conditions | Technically difficult | — | |
| Mean mitral gradient (mmHg) | CW Doppler on mitral flow | Easy to obtain | Depends on heart rate and flow conditions | Right + left catheterization |
| Pulmonary artery pressure (mmHg) | CW Doppler on tricuspid regurgitant flow | Easy to obtain in cases of tricuspid regurgitation | Arbitrary estimation of right atrial pressure; no estimation of pulmonary vascular resistance | Right catheterization (reference measurement) |
| Mean gradient and pulmonary artery pressure at exercise (mmHg) | CW Doppler of mitral and tricuspid regurgitant flow | Objective assessment of exercise tolerance | Lack of validation for decision making | — |
When the MVA is greater than 1.5 cm 2 , the hemodynamics are not affected at rest. Interventions for MS are considered when the MVA is smaller than 1.5 cm 2 . , , Mitral valve resistance has been proposed as a marker of severity but has no additional value compared with MVA.
Analysis of the morphology of the valve leaflets, mitral annulus, and subvalvular apparatus using 2D echocardiography is a key feature in the diagnosis of MS and its mechanism. It also has implications for the choice of the most appropriate intervention.
Rheumatic MS is characterized by commissural fusion, restriction of posterior leaflet motion, and impairment of the subvalvular apparatus. Valve calcification may involve both leaflets but seldom affects the mitral annulus. Degenerative MS is characterized by extensive calcification of the mitral annulus, which appears as a dense band located between the posterior leaflet and the posterior wall with acoustic shadowing. Calcification often extends to the base of the leaflets, but there is no commissural fusion, and the leaflet tips are less frequently involved. Thickening and restriction of the motion of both leaflets is frequently observed when MAC causes severe MS. ,
In rheumatic MS, echocardiographic evaluation assesses leaflet thickening (significant if ≥5 mm), leaflet mobility in the long-axis parasternal view, and calcification, which is best confirmed by fluoroscopic examination. The parasternal short-axis view is paramount for planimetry and for evaluating the homogeneity of the impairment of the mitral orifice, focusing on commissural areas ( Fig. 16.3 ). The long-axis parasternal and apical views enable assessment of the subvalvular apparatus (i.e., thickening and/or shortening of chordae), although impairment tends to be underestimated compared with anatomic findings.
The severity of valvular and subvalvular involvement usually is described by a combined score in rheumatic MS. The Wilkins echocardiographic score grades each of the following components of the mitral apparatus from 1 to 4: leaflet mobility, thickness, calcification, and impairment of the subvalvular apparatus ( Table 16.2 ). Total scores range from 4 to 16. An alternative approach is to assess the whole mitral valve anatomy according to the best surgical alternative; three classifications are identified based on echocardiography and fluoroscopy ( Table 16.3 ).
| Grade a | Mobility | Thickening | Calcification | Subvalvular Thickening |
|---|---|---|---|---|
| 1 | Highly mobile valve with only leaflet tips restricted | Leaflets near normal in thickness (4–5 mm) | A single area of increased echocardiographic brightness | Minimal thickening just below the mitral leaflets |
| 2 | Leaflet middle and base portions have normal mobility | Mid-leaflets normal, considerable thickening of margins (5–8 mm) | Scattered areas of brightness confined to leaflet margins | Thickening of chordal structures extending to one of the chordal length |
| 3 | Valve continues to move forward in diastole, mainly from the base | Thickening extending through the entire leaflet (5–8 mm) | Brightness extending into the midportions of the leaflets | Thickening extended to distal third of the chords |
| 4 | No or minimal forward movement of the leaflets in diastole | Considerable thickening of all leaflet tissue (>8–10 mm) | Extensive brightness throughout much of the leaflet tissue | Extensive thickening and shortening of all chordal structures extending down to the papillary muscles |
a Each component is graded separately, and the total score is the sum of the four items, ranging between 4 and 16.
| Echocardiographic Group | Mitral Valve Anatomy |
|---|---|
| Group 1 | Pliable noncalcified anterior mitral leaflet and mild subvalvular disease (i.e., thin chordae ≥ 10 mm long) |
| Group 2 | Pliable noncalcified anterior mitral leaflet and severe subvalvular disease (i.e., thickened chordae ≤ 10 mm long) |
| Group 3 | Calcification of mitral valve of any extent as assessed by fluoroscopy, whatever the state of the subvalvular apparatus |
These two scores share limitations related to the lack of a detailed location of calcification and leaflet thickening, particularly in relation to commissural areas, which are likely to influence the results of BMC. They tend to underestimate the weight of subvalvular apparatus impairment. Other scoring systems involve a more detailed approach, including quantitative approaches and analysis of commissural areas. , , Good prediction of the results of BMC has been shown for small numbers of patients, but validation in large series using multivariate analyses including other predictors is lacking. No comparative evaluation of scoring systems enables a particular one to be recommended. It is unlikely that a single scoring system could combine reproducibility and accurate prediction of the results of BMC. Echocardiographers use a method with which they are familiar and that includes the assessment of valve morphology among other clinical and echocardiographic findings.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here