Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter deals with two final options to preserve some effective function of the extremity. Other revision replacement options are discussed in Chapter 106, Chapter 107, Chapter 108 . We continue to use reinsertion into the cement host; strut grafting for deficiency and fracture and impaction grafting. However, when none of these strategies is viable ( Fig. 109.1 ), there are two remaining options to restore function: total humeral replacement and allograft prosthetic replacement (APC). Bulk allograft replacements are still used to reconstruct deficiencies after tumor resection. Total allograft replacement has been abandoned due to the eventual development of neurotrophic resorption and dysfunction.

In the early years of joint replacement salvage options, usually for infection, were resection or fusion. Allograft composite revision was considered unreliable. Extensive bone loss made fusion difficult at best, and the resection was dysfunctionally unstable (see Chapter 5 ). Adopting techniques from hip revision and tumor surgery we attempted allograft prosthetic reconstruction for massive bone loss in the 1990s. However, a review of 13 procedures revealed a complication rate of 55% and a success rate of only 60%, and we therefore placed a moratorium on this strategy. Still the relentless stream of what appeared as near hopeless salvage pathologies, along with the recognition of the effectiveness of strut graft augmentation, prompted reconsideration of the proposition. We abandoned the step-cut transverse-type interface and the need for plate and screw stabilization in favor of linear strut contact and monofilament wire cerclage stabilization.
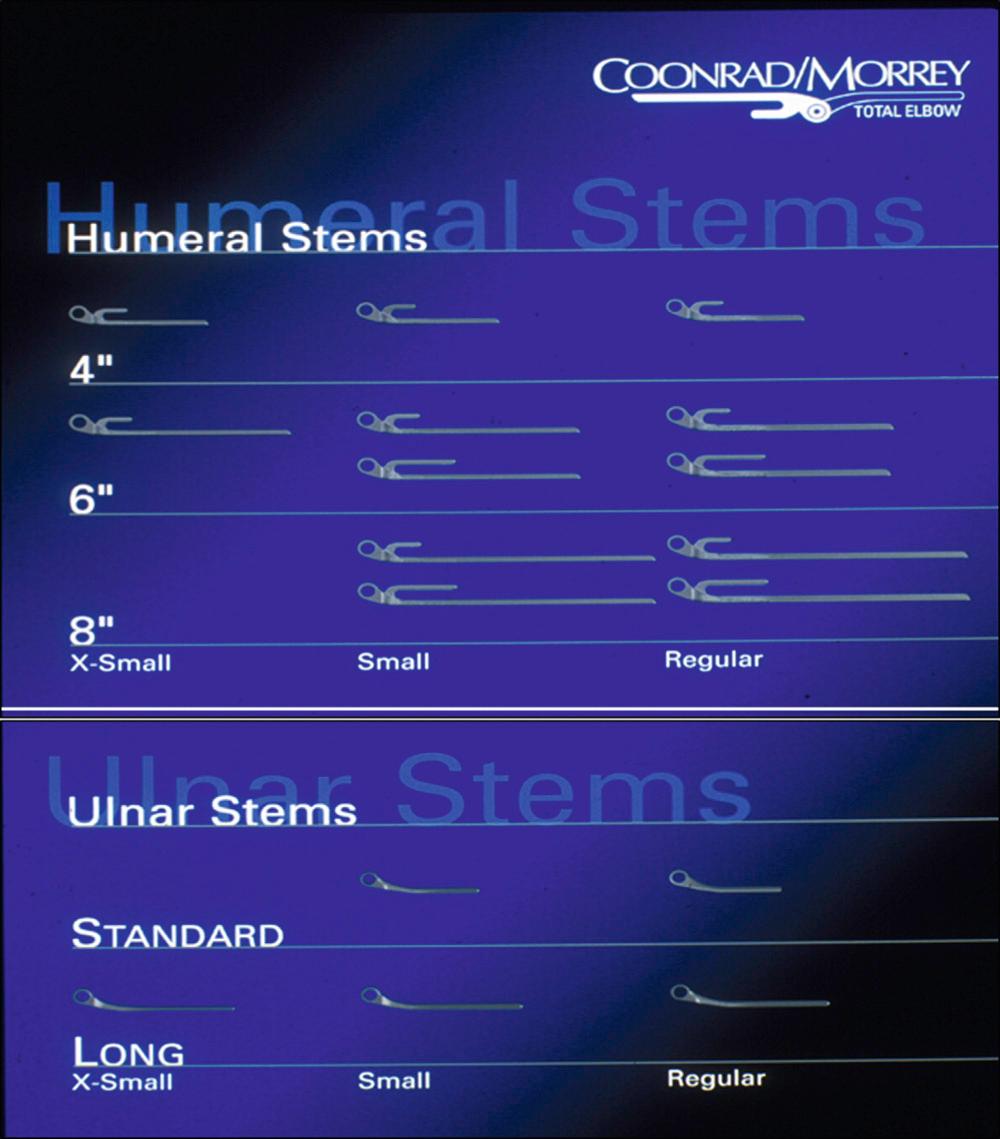
As with any revision option, having a spectrum of off-the-shelf implant options is critical and obviates the need for expensive and ineffective custom devices ( Fig. 109.2 ). We feel a linked implant is essential for a reliable outcome.
Septic loss of bone is a near-hopeless revision circumstance. Improved methods to document the potential for residual infection and recognizing the value of staged reimplantation are additional developments, which further prompted the used of the APC.
Bulk allografts are known to resorb around the hip, especially the acetabulum. There has been documentation of more bulk graft resorption about the elbow than at the shoulder. However, the justification of this concept resides in the absence of any other viable option to restore function, at least at this time.
The technical difficulty and the clinical inadequacy of achieving precise step-cuts prompted the concept of a side-to-side graft/host bone construct. There are three essential concepts to be realized ( Fig. 109.3 ):
The component is fixed in a circumferentially intact graft.
Incorporation is enhanced by extensive contact at the graft/host interface.
Stabilization is by cerclage wire, making it independent of compromised host bone holding a screw.
The APC is used when strut augmentation is considered inadequate.

The classification is based on experience with three distinct types of osseous deficiencies ( Fig. 109.4 ).

Expanded cortex
Osteolysis
Length deficiency usually not an issue
The implant is secured to a circumferential graft that is then fashioned and “intussipated” into the host bone ( Fig. 109.5 ). Ideally the stem will be long enough to be cemented into the host bone.
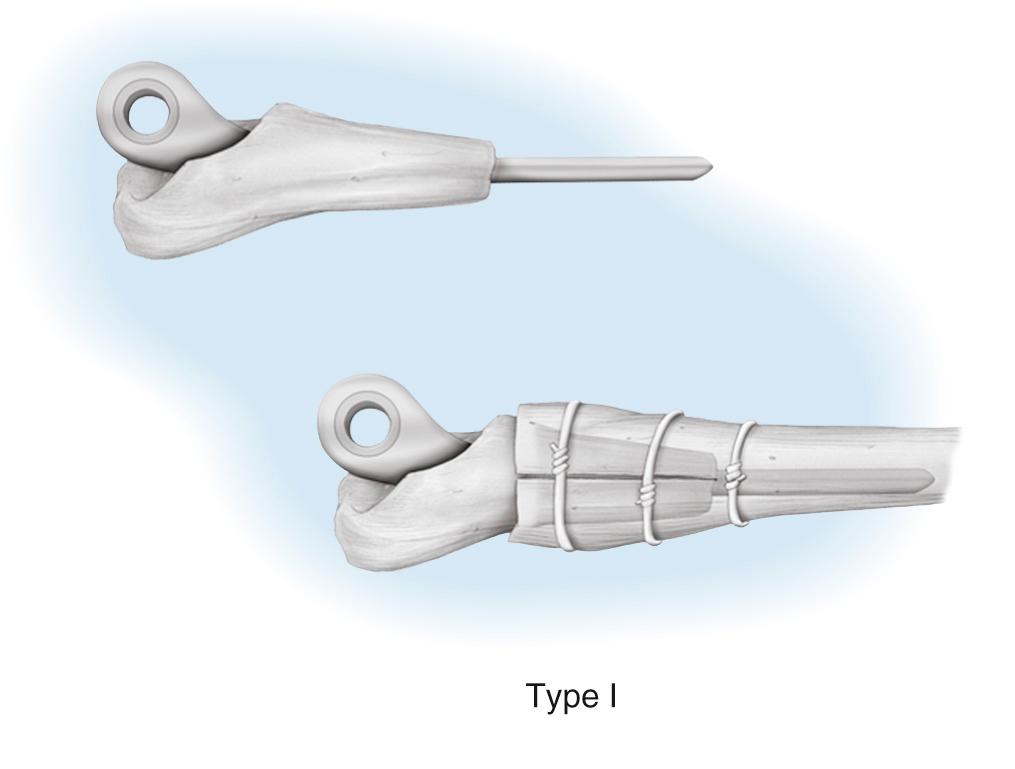
Rarely the graft will be placed over the host bone.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here