Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
| Sign or symptom | Pathological basis |
|---|---|
| Sputum | |
|
Excess secretion from bronchial mucous glands (e.g. in asthma and chronic bronchitis) Inflammatory exudate from respiratory tract infection Ulceration of airways or damage to pulmonary vasculature (e.g. lung tumours, pulmonary infarcts, bronchiectasis, aspergilloma) |
| Cough | Physiological reflex response to presence of mucus, exudate, tumour or foreign material |
| Wheezing | |
|
Narrowing of larynx, trachea or proximal bronchi (e.g. by tumour) Distal bronchial narrowing (e.g. asthma) |
| Dyspnoea | Decreased oxygen in the blood from impaired alveolar gas exchange, left heart failure or anaemia |
| Cyanosis | Increased nonoxygenated (circulatory bypassing of lungs in congenital heart diseases or impaired alveolar gas exchange) |
| Pleuritic pain | Irritation of the pleura due to pulmonary inflammation, infarction or tumour |
| Pleural effusion | |
|
Cardiac failure. Hypoalbuminaemia (e.g. cirrhosis, nephrotic syndrome) Pleural inflammation or tumour |
| Finger clubbing | Often accompanies carcinoma of lung, bronchiectasis and pulmonary fibrosis, as well as, less commonly, cirrhosis and chronic inflammatory bowel disease |
| Weight loss | Protein catabolic state induced by chronic inflammatory disease (e.g. tuberculosis) or tumours |
| Auscultation signs | |
|
Sudden inspirational opening of small airways resisted by fluid or fibrosis Generalised or localised airway narrowing Pleural surface roughened by exudate |
| Percussion signs | |
|
Consolidation of lung by exudate (pneumonia) pleural effusion Increased gas content of thorax due to pneumothorax or emphysema |
Global estimates suggest that in the early 21st century respiratory diseases account for around 16% of all deaths worldwide. Acute respiratory infections account for around 4 million of which around 1.3 million are in children under 5 years (18% of childhood mortality). In 2011 there were 8.7 million new cases of tuberculosis (TB) and 1.6 million deaths. Up to 13% of TB cases were associated with HIV infection. Smoking-related conditions also account for many deaths. Lung cancer has an annual mortality of around 1.4 million (around 18% of all cancer deaths) and 2.5 million deaths occur from chronic obstructive pulmonary disease (COPD). There is also considerable morbidity due to respiratory disease: it is estimated that, in the UK, about 40% of absence from work is the result of respiratory disease, approximately 85% of which are transient infections of the upper respiratory tract ( Table 14.1 ).
| Aetiological factor | Disease |
|---|---|
| Genetic | Cystic fibrosis Alpha-1 antitrypsin deficiency Some asthma |
| Environmental | |
| Infection | Influenza Measles Bacterial pneumonias Tuberculosis |
| Smoking | Lung cancer Chronic bronchitis and emphysema Susceptibility to infection |
| Air pollution | Chronic bronchitis Susceptibility to infection |
| Occupation | Pneumoconiosis Asbestosis, mesothelioma and lung cancer |
The respiratory system extends from the nasal orifices to the periphery of the lung and includes the surrounding pleural cavity ( Fig. 14.1 ).
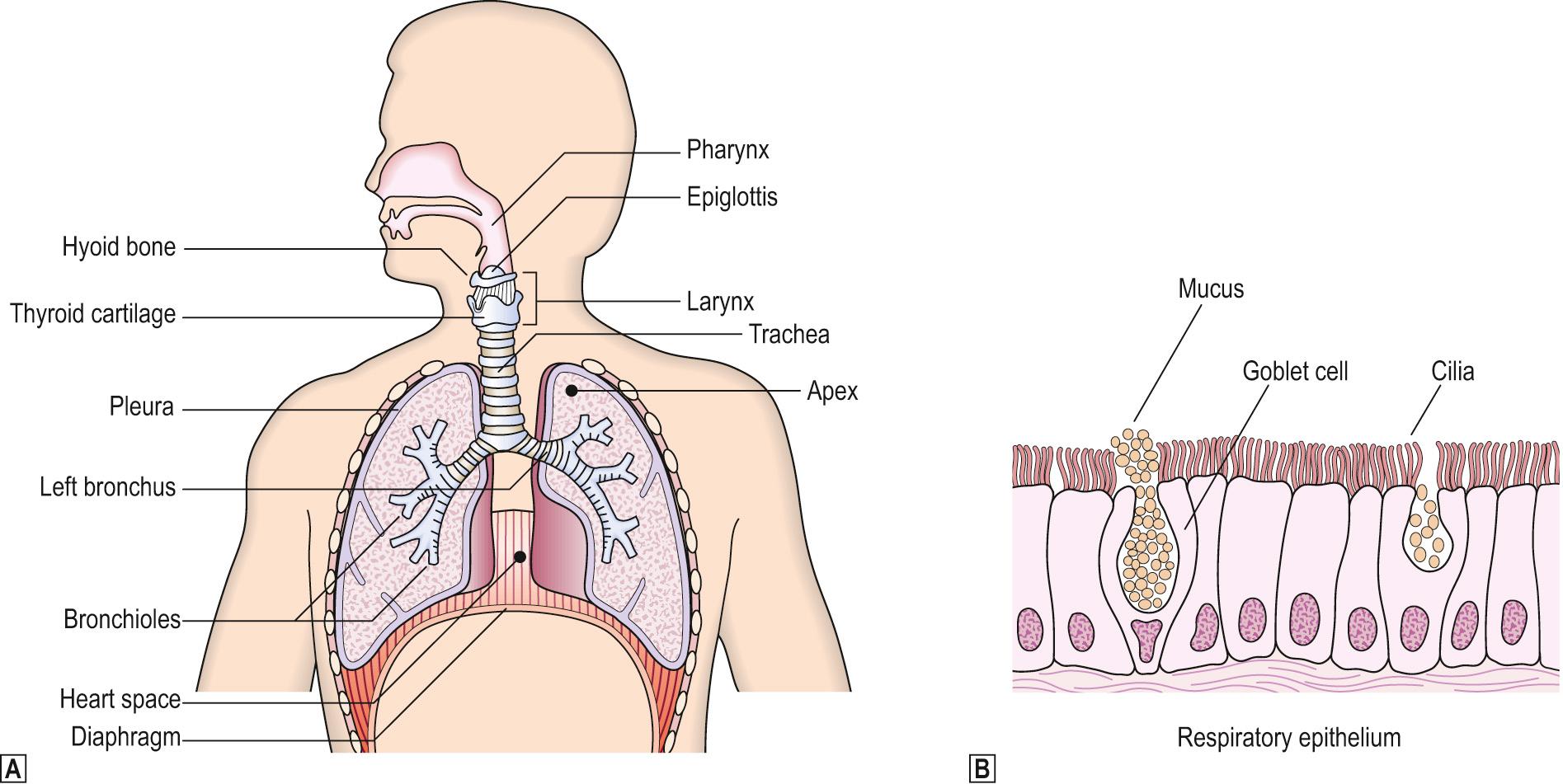
These constitute the upper respiratory tract. The nasal passages and sinuses are in continuity and are lined by pseudostratified columnar epithelial cells with admixed goblet cells (respiratory mucosa). The hairs in the nose trap large particles of foreign material, thereby filtering the air. The air is also warmed and humidified as it passes through the nasal cavity. The middle ear, also lined with respiratory epithelium, connects with the nasal cavity via the Eustachian tube.
The larynx connects the trachea to the pharynx. Consisting of a complicated system of cartilages and muscles, it allows air into the trachea, with the epiglottis preventing the passage of food into the lungs, and also produces sound for speaking. Part of the larynx, including the vocal cords and epiglottis, is covered with nonkeratinising squamous epithelium similar to that lining the oral cavity, pharynx and oesophagus.
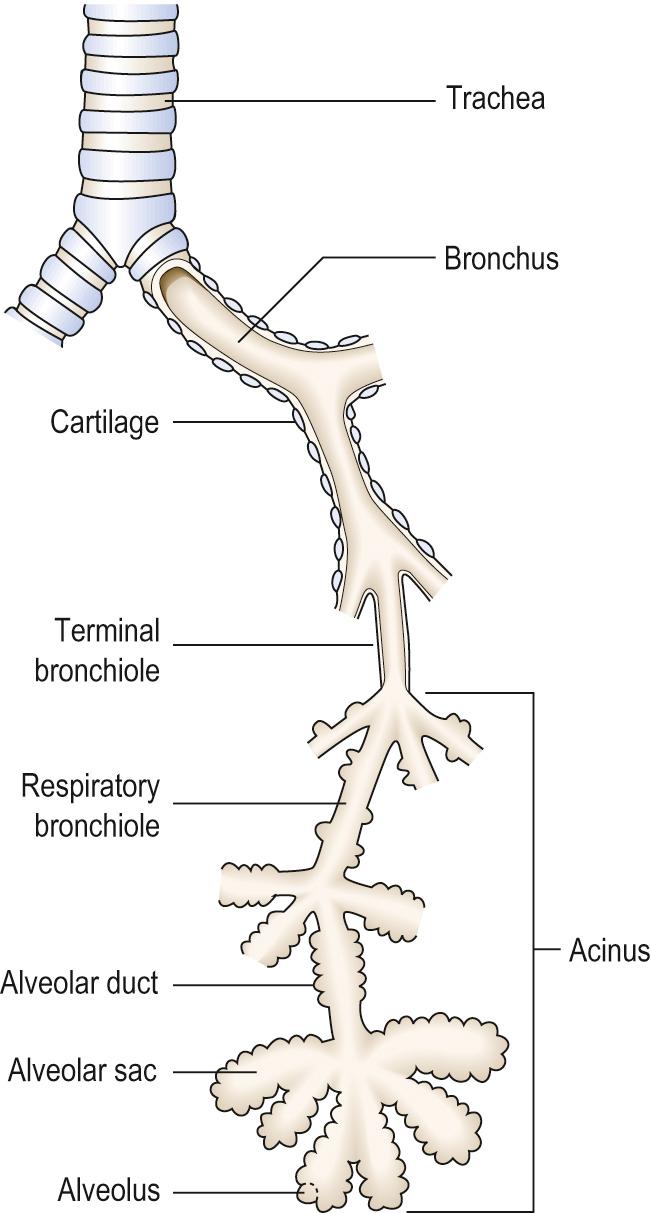
The lower respiratory tract consists of the trachea, bronchi, bronchioles, alveolar ducts and alveoli ( Fig. 14.2 ) that develop from an outpouching of the foregut at around the fifth week of development. The structure of the airway at each level differs ( Table 14.2 ).
| Part of respiratory tract | Structure |
|---|---|
| Trachea | Anterior C-shaped plates of cartilage with posterior smooth muscle. Mucous glands |
| Bronchi | Discontinuous foci of cartilage with smooth muscle. Mucous glands |
| Bronchioles | No cartilage or submucosal mucous glands. Clara cells secreting proteinaceous fluid. Ciliated epithelium |
| Alveolar duct | Flat epithelium. No glands. No cilia |
| Alveoli | Type I and II pneumocytes |
The lungs are divided into lobes : the right lung has three lobes (upper, middle, lower); the left lung has only two lobes (upper and lower). Each lung is formed of anatomically defined bronchopulmonary segments, 10 on the right and 8 or 9 on the left. Each segment is supplied by segmental branches of the pulmonary artery and bronchus (the bronchovascular bundle). The veins draining adjacent segments often anastomose before they reach the hilum and run principally in the fibrous septae of the lungs.
The airways (trachea, bronchi and bronchioles) are lined by respiratory epithelium and branch until they form terminal bronchioles less than 2 mm in diameter. The respiratory system distal to the terminal bronchiole is called the acinus or terminal respiratory unit , and comprises respiratory bronchioles and alveoli where gas exchange occurs. A group of three to five acini is called a lobule.
The alveoli are lined by flattened type I pneumocytes with occasional type II pneumocytes; the latter are rounded cells with surface microvilli. Type II cells secrete surfactant, replicate quickly after injury to alveolar walls and are believed to be the stem cell population of the alveolus. Beneath the alveolar cells lies a basement membrane which is shared by the alveolar capillary endothelial cells, thus permitting rapid and efficient gas exchange by diffusion.
The lung is encased by the visceral pleura , which is a thin layer of fibroconnective tissue and elastin with overlying mesothelial cells. The lungs sit within the chest cavity surrounded by the parietal pleura, diaphragm, ribs and intercostal muscles, mediastinal structures, vertebral column and sternum.
The lungs have a dual arterial blood supply . The trunk of the pulmonary artery arises from the right ventricle, splits into right and left main pulmonary arteries and then follows the airways, forming the bronchovascular bundles. The bronchial arteries arise from the descending thoracic aorta and supply oxygenated blood to lung parenchyma. Pulmonary veins run in the interlobular septae, taking all the blood from the lungs back to the left atrium.
Pulmonary lymphatic channels in the septae and pleura drain into the thoracic duct.
Respiration is controlled by the respiratory centre in the medulla oblongata, and the carotid bodies situated at the carotid bifurcations. The medullary centre senses changes in CO 2 /H + concentration in the cerebrospinal fluid, and modifies respiration by nervous stimulation of respiratory muscles and the diaphragm. The partial pressure of O 2 in the blood is monitored by the carotid bodies , which can stimulate the respiratory centre through the glossopharyngeal nerves. Carotid bodies can become hyperplastic in response to chronic arterial hypoxaemia, such as occurs in high-altitude dwellers and in patients with long-standing COPD.
Gas exchange can only occur in alveoli that are both perfused and ventilated. Ventilation of nonperfused alveoli increases ‘dead space’, that proportion of inspired air not involved with gas exchange. Perfusion of nonventilated alveoli leads to shunting of nonoxygenated blood from the pulmonary to the systemic circulation..
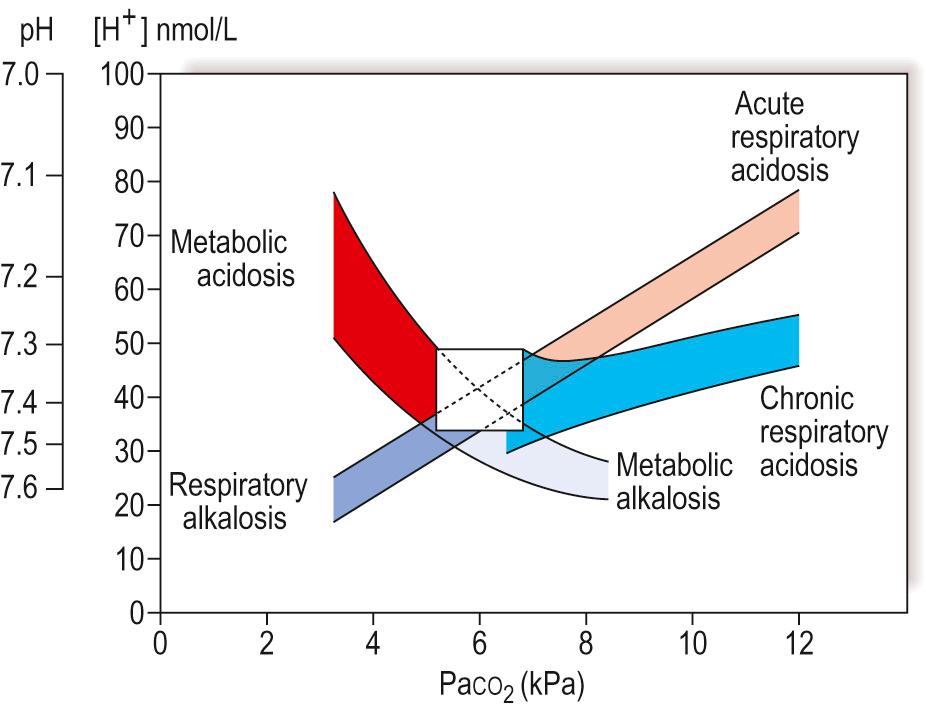
Normal acid-base balance in blood is dependent on efficient alveolar ventilation/perfusion, and adequate renal function. Metabolic and respiratory disease states can lead to disturbances in acid-base balance ( Fig. 14.3 ) with effects on respiration, for example, diabetic patients with ketoacidosis have a high [H] + (metabolic acidosis). This will result in an increased respiratory rate, reducing the blood concentrations of CO 2 (compensatory respiratory alkalosis) buffering the acidosis. If the disease becomes chronic, compensatory mechanisms by both the lungs and kidneys operate in an attempt to restore blood pH.
In normal quiet respiration, only a relatively small proportion of the total lung capacity (TLC) is inhaled and exhaled; this is the tidal volume (TV). TLC is made up of the amount of air totally exhaled after maximum inspiration (the vital capacity or VC) and the residual volume (RV). TLC, RV, TV and VC are all easily measured in the laboratory using helium dilution techniques.
In addition to calculating volume parameters, some techniques also assess actual pulmonary function. Spirometry measures the amount of exhaled air per second. The maximum volume of air blown from the lungs within the first second after a previous maximum inspiration is called the forced expiratory volume (FEV 1 ). This figure is a measure of small airway resistance and the predicted normal value is dependent on the patient's age, sex and size; for example, the small lungs of a child obviously cannot expel as much air as those of an adult. The ratio FEV 1 :VC compensates to a degree for the variability of lung size. It is possible to inhale more rapidly than exhale because, during inspiration, forces on the airways tend to open them further; during expiration, opposite forces tend to close the airways and thus restrict airflow. For a given lung volume, the expiratory flow rate reaches a peak (PEFR), which is again a measure of airways resistance.
An assessment of the ability of the lungs to exchange gas efficiently can be made by measuring the transfer factor for carbon monoxide (T CO ). Air containing a known concentration of carbon monoxide is inhaled; the breath is held for 15 seconds and then exhaled. The amount of carbon monoxide absorbed is a measure of pulmonary gas exchange. T CO is dependent on the concentration of blood haemoglobin, which has a strong affinity for carbon monoxide. Diseases that diffusely affect the alveolar capillary membrane (such as diffuse pulmonary fibrosis or emphysema where there is loss of alveolar surface area) will result in a low T CO .
There are two major patterns of abnormal pulmonary function tests: obstructive defects (e.g. asthma) and restrictive defects (e.g. pulmonary fibrosis) ( Table 14.3 ).
| Test | Diagnostic significance |
|---|---|
| Peak expiratory flow rate (PEFR) | Reduced with obstructed airways or muscle weakness |
| Forced expiratory volume in 1 second (FEV 1 ) | Reduced with obstructed airways, pulmonary fibrosis or oedema, or muscle weakness |
| Vital capacity (VC) | Reduced with reduction in effective lung volume (fibrosis or oedema), chest wall deformity (kyphoscoliosis), or muscle weakness Increased in emphysema |
| Forced expiratory ratio (FEV 1 :VC) | Low in obstructive defects Normal or high in restrictive defects |
| Carbon monoxide transfer (T CO ) | Reduced in pulmonary fibrosis, emphysema, oedema, embolism and anaemia |
In obstructive airways disease, RV and TLC are mildly increased due to hyperinflation of the lung while FEV 1 , VC and the FEV 1 :VC ratio is decreased. Clearly, in conditions such as asthma where there is variability in the degree of airway obstruction, the results of pulmonary function tests will depend on the clinical state of the patient and the presence of symptoms. Restrictive diseases are those that result in the lung becoming stiffer and are associated with reduced RV and TLC. The FEV 1 and VC may be reduced but their ratio remains normal. These tests are of most value in the follow-up of patients and can be used to monitor responses to therapy (e.g. asthma) and disease progression (e.g. pulmonary fibrosis).
Respiratory failure can occur as a result of:
impaired ventilation
neural problems, for example, due to narcotics, encephalitis, a cerebral space-occupying lesion, poliomyelitis, motor neurone disease, and so on
mechanical problems, for example, airway obstruction, trauma, kyphoscoliosis, muscle disease, pleural effusion, gross obesity (Pickwickian syndrome)
impaired perfusion, if diffuse or extensive, for example, cardiac failure or multiple pulmonary emboli
impaired gas exchange defects, if diffuse and severe, for example, emphysema or diffuse pulmonary fibrosis.
Type I respiratory failure is characterised by hypoxia and a low level of CO 2 in the blood secondary to hyperventilation. In type II respiratory failure, the hypoxia is associated with hypoventilation resulting in impaired clearance of CO 2 and hypercapnia. In acute type II respiratory failure, there is respiratory acidosis due to an increased [H] + . In chronic respiratory failure, this will be buffered by increased bicarbonate retention by the kidneys (compensatory metabolic alkalosis) (see Fig. 14.3 ).
Respiratory diseases of infancy and childhood are predominantly infectious (see Respiratory Infections , p. 292 ); such diseases, together with diarrhoea, are the primary cause of death in childhood in the developing world. Rarely, disease may arise as a result of either developmental abnormalities or immaturity.
Developmental abnormalities include:
tracheoesophageal fistula
congenital diaphragmatic hernia with pulmonary hypoplasia
congenital cystic adenomatoid malformations
bronchogenic/foregut cysts
pulmonary sequestration
congenital lobar emphysema.
Embryologically, the oesophagus and the trachea begin as a single tube; the trachea then buds off to form the pulmonary tree. A variety of anatomical abnormalities may be seen associated with fistulae, including oesophageal atresia.
This presents as neonatal respiratory distress due to herniation of the stomach and loops of bowel into the thorax. Usually, the left diaphragm is defective and surgical correction to restore normal thoracic and abdominal anatomy is essential at the earliest possible opportunity.
These are characterised by abnormalities in the development of small airways and the alveolar tissue of the lung. This results in the development of cysts within the lung which may be of varying size and can be localised to one lobe or be extensive and bilateral. The prognosis depends on the pattern of abnormality present and any other associated abnormalities.
These occur in the lung or mediastinum and may be lined either by bronchial elements such as cartilage, smooth muscle and ciliated respiratory epithelium (bronchogenic cysts), or by squamous or even gastric or pancreatic-type epithelium (foregut cysts). Usually, such cysts are asymptomatic.
A sequestered piece of lung is a mass of abnormal lung that does not communicate anatomically with the tracheobronchial tree, often being supplied by an anomalous artery, usually from the aorta. Sequestered segments of lung are found most often within the left lower lobe.
This condition is characterised by overdistension of a lobe due to intermittent bronchial obstruction, with the left upper lobe most frequently affected. The pathogenesis is thought to be related to abnormal bronchial cartilage allowing inspiration of air but restricting expiration.
Diseases due to immaturity include:
hyaline membrane disease (HMD) or idiopathic respiratory distress syndrome
bronchopulmonary dysplasia.
Complication of prematurity (less than 36 weeks' gestation)
Due to deficiency of pulmonary surfactant
Tachypnoea, dyspnoea, expiratory grunting, cyanosis
Diffuse alveolar damage with hyaline membranes
Increased risk associated with maternal diabetes, multiple pregnancy, Caesarean section, amniotic fluid aspiration
HMD is almost always seen in premature infants of birth weight less than 2.5 kg. Infants are usually of less than 36 weeks' gestation, and the incidence of HMD rises as the gestational age decreases. The risk of developing HMD may be decreased by giving mothers oral corticosteroids prior to delivery of the baby as this appears to stimulate surfactant production in the lungs.
After a few hours of relatively normal respiration, symptoms of tachypnoea and dyspnoea with expiratory grunting appear. Cyanosis quickly follows, with worsening respiratory distress with hypoxaemia refractory to high concentrations of inhaled oxygen.
The pathogenesis is thought to be due to a deficiency of surfactant. This is secreted by type II pneumocytes, and normally lines alveolar spaces, reducing surface tension, thereby allowing airway opening more easily during inspiration.
In fatal cases, the lungs are heavy, purple and solid, and sink in water. Histology shows alveoli with hyaline membranes. If the infant survives, resolution may occur within the next few days, although in some cases this will be associated with fibrosis and the development of bronchopulmonary dysplasia.
Bronchopulmonary dysplasia is the term used to describe the picture of lung organisation after HMD. Often, infants have been previously treated with high levels of oxygen, and it is not clear whether bronchopulmonary dysplasia is related to oxygen toxicity or merely a result of organisation after HMD. The features are of interstitial and peribronchial fibrosis. Patients may be left with very severe respiratory dysfunction requiring long-term oxygen therapy and even ventilation, depending on the severity.
Inflammatory diseases, for example, rhinitis, are very common
Nasal polyps are either inflammatory or allergic
Malignant tumours are rare
Rhinitis may be caused by many different viruses, especially rhinoviruses (the common cold virus), although respiratory syncytial virus (RSV), parainfluenza viruses, coronaviruses, Coxsackie viruses, echoviruses and bacteria, such as Haemophilus influenzae , may also be implicated. Rhinitis may also be caused by inhaled allergens as in ‘hay fever’ where the inflammatory reaction is mediated via type I and type III hypersensitivity reactions ( Chs. 8 and 9 ).
Nasal polyps most commonly arise due to chronic allergic inflammation. They consist of polypoid oedematous masses of mucosal tissue infiltrated with chronic inflammatory cells, especially plasma cells; eosinophils may be numerous.
Sinusitis is inflammation of the paranasal sinuses; it may be acute or chronic and can be infective or allergic. If the drainage orifice is blocked by inflamed swollen mucosa, an abscess may follow. Cranial osteomyelitis, meningitis or cerebral abscess may then result from sinusitis by direct extension.
Granulomatous angiitis (Wegener granulomatosis) , a granulomatous form of vasculitis (see Vascular Diseases , p. 299 ) may involve the nose and upper respiratory tract and present with septal perforation or collapse of the nasal cartilages.
Otitis media is infection of the middle ear, often viral, associated with generalised upper respiratory tract symptoms. The Eustachian tube may become swollen and blocked, leading to trapping of exudate in the middle ear. Eardrum perforation may ensue. In bacterial infections, more serious, but rare, complications include mastoiditis, meningitis and brain abscess.
Tumours of the nasal passages and sinuses are uncommon. They may be:
benign: squamous papilloma, juvenile angiofibroma
malignant: squamous cell carcinoma (SqCC), adenocarcinoma (AC), melanoma, lymphoma.
Squamous papillomata are benign lesions some of which are related to human papillomavirus infection.
Juvenile angiofibromas are rare and occur exclusively in males, usually during adolescence. They are extremely vascular, and surgical removal can be difficult. These tumours contain androgen receptors, explaining the male preponderance.
SqCC may be well differentiated, producing keratin, or very poorly differentiated. In the nasopharynx ( nasopharyngeal carcinoma ), these may contain many lymphocytes and have been misnamed ‘lymphoepitheliomas’. Such tumours are most common in South-East Asia where the Epstein–Barr virus is involved in the aetiology, although this association is less commonly found in Caucasian populations.
AC of the nasal passages and sinuses are rare and may be more common in those with occupational exposure to wood dust for example, furniture makers. These tumours may present clinically up to 40 years after initial exposure.
Primary mucosal melanomas of the nose and sinuses are rare but have a very poor prognosis.
Primary extranodal lymphomas are almost always of non-Hodgkin type.
Laryngitis may be infective, allergic or irritative
Polyps and papillomas are benign lesions
SqCC, typically in male smokers
Laryngitis may occur in association with viral or bacterial inflammation of trachea and bronchi; this is laryngotracheobronchitis. Diphtheria was once a common, and serious, bacterial cause of laryngitis, leading to the formation of a fibrinopurulent membrane that could cause airway obstruction. Chronic laryngitis may be irritative and due to cigarette smoke, chronic acid reflux or mechanical factors, for example, recent endotracheal intubation.
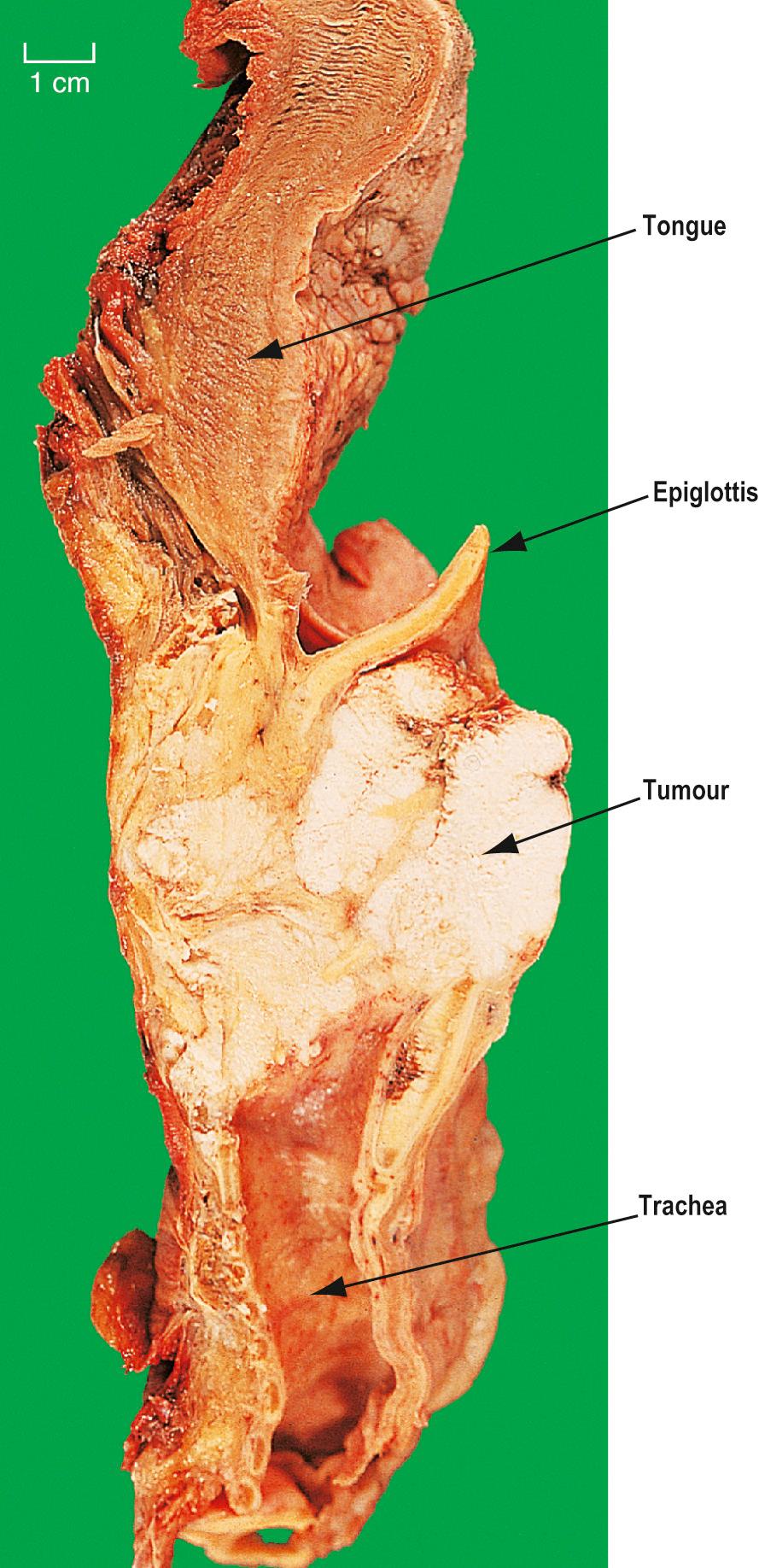
Epiglottitis is caused by capsulated forms of H. influenzae type B. The epiglottis becomes inflamed and greatly swollen, leading to airway obstruction ( Fig. 14.4 ). Treatment is by intubation, although, rarely, tracheostomy may be necessary; antibiotics are also given to treat the infection.
Laryngeal polyps often develop in singers and are thus sometimes referred to as ‘singer's nodes’. Even when only a few millimetres in diameter, they can alter the character of the voice.
Laryngeal tumours may be:
benign: squamous papilloma
malignant: SqCC.
Papillomas may be caused by types of human papillomavirus. Papillomas consist of squamous epithelium covering fibrovascular cores of stroma. They may be multiple and recurrent, especially in children, but are usually single in adults. Such papillomas can extend into the trachea and bronchi.
SqCC of the larynx typically affects males over 40 years of age and are associated with cigarette smoking. Tumours are often preceded by a phase of dysplasia. The dysplasia, especially if low grade, may be reversible with smoking cessation.
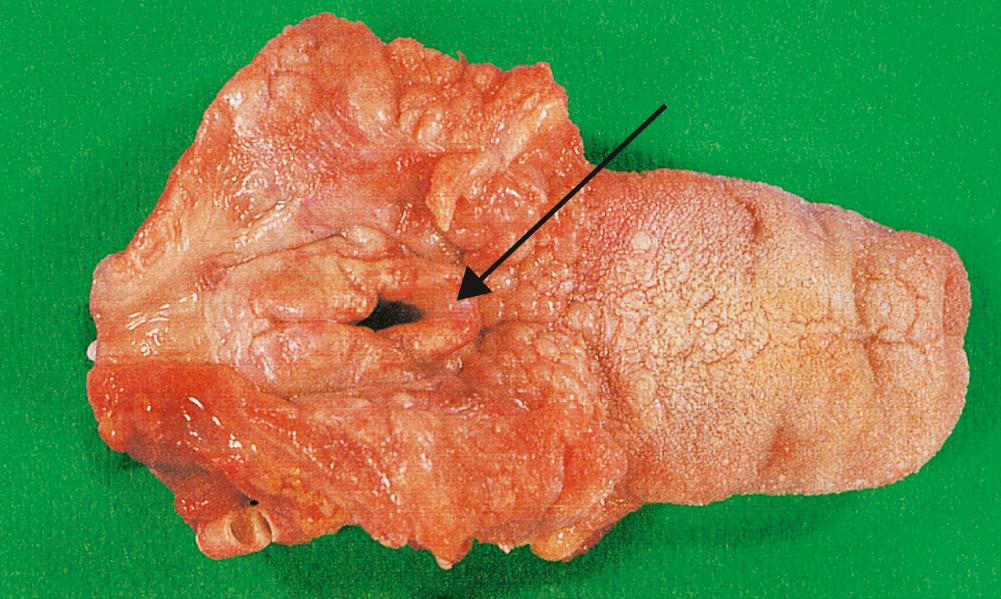
Most laryngeal carcinomas arise on the vocal cords ( Fig. 14.5 ), although they may arise above, in the pyriform fossa, or below, as upper tracheal carcinomas. Symptoms are hoarseness of voice and, later, pain, haemoptysis and dysphagia. The lesions ulcerate, fungate, invade locally and metastasise to regional lymph nodes in the neck. Treatment is by chemoradiotherapy and/or resection. These patients often have widespread mucosal abnormalities throughout the upper aerodigestive and respiratory tracts and are at high risk of developing further cancers, especially if they continue to smoke.
The lungs have an internal surface area of approximately 500 m 2 which is exposed to the external environment and potentially subjected to inhaled microbes with every breath. It is therefore not surprising that respiratory infections are relatively common, with the World Health Organization projecting such infections to continue as one of the global leading causes of death and disability. Countering the threat of pathogens are the defence mechanisms, any abnormality of which may predispose to infection:
loss or suppression of the cough reflex, for example, in coma, anaesthesia, neuromuscular disorders, or after surgery
ciliary defects, for example, in immotile cilia syndromes, or loss of ciliated cells with squamous metaplasia
mucus disorders, for example, excessive viscosity as in cystic fibrosis
acquired or congenital hypogammaglobulinaemia, for example, with decreased immunoglobulin A in the mucus
acquired or congenital immunosuppression, for example, thymic aplasia, neutropenia following chemotherapy, steroid therapy or HIV infection
decreased macrophage function, for example, in people who smoke or are hypoxic
the extremes of age and the presence of comorbid conditions.
Infections can be classified as primary , with no underlying predisposing condition in a healthy individual, or secondary , when local or systemic defences are weakened. The latter are by far the most common types of respiratory infection in developed countries.
Characterised by cough, dyspnoea, tachypnoea, sputum
Usually viral
In acute bronchitis, the trachea and larynx are involved as well as the bronchi, and the disease is often known as acute laryngotracheobronchitis (or ‘croup’). The disease is most severe in children. Viruses are usually the cause, especially RSV, although H. influenzae and Streptococcus pneumoniae are frequent bacterial causes. Acute bronchitis may be caused by direct chemical injury from air pollutants, such as smoke, sulphur dioxide and chlorine.
Chronic bronchitis is a clinical term defined as cough and sputum for 3 months in 2 consecutive years; it is discussed below under diffuse obstructive airways disease ( p. 302 ). Episodes of acute bronchitis are common in COPD, and cause a sudden deterioration in pulmonary function with cough and the production of purulent sputum.
Usually a primary viral infection in infants (RSV)
May be secondary to other inhaled irritants or part of a systemic disease process
Causes dyspnoea and tachypnoea
Acute bronchiolitis is a respiratory infection caused by viruses, especially RSV, in infants. Symptoms are of acute respiratory distress with dyspnoea and tachypnoea. Most cases resolve within a few days, although a minority may develop secondary pneumonia or complications such as obliterative bronchiolitis where the small airways are obliterated by fibrous tissue.
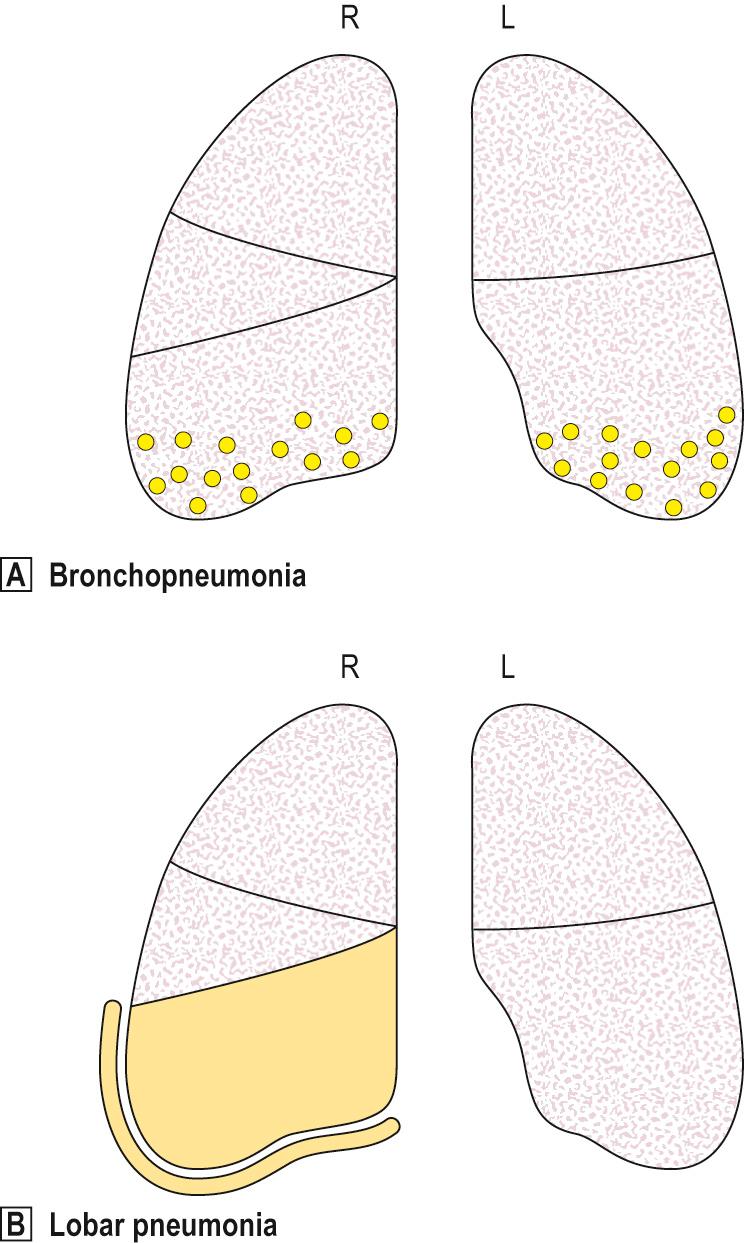
Pneumonia is usually due to infection affecting distal airways and alveoli, with the formation of an inflammatory exudate. It may be classified according to several criteria ( Table 14.4 ; Fig. 14.6 ).
| Criterion | Type | Example/comment |
|---|---|---|
| Anatomical pattern | Bronchopneumonia Lobar pneumonia | Most widely used classification before identifying aetiological agent |
| Clinical circumstances | Primary | In an otherwise healthy person |
| Secondary | With local or systemic defects in defence | |
| Aetiological agent | Bacterial | Streptococcus pneumoniae , Staphylococcus aureus , Mycobacterium tuberculosis , etc. |
| Viral | Influenza, measles, etc. | |
| Fungal | Cryptococcus , Candida , Aspergillus , etc. | |
| Other | Pneumocystis jiroveci , Mycoplasma , aspiration, lipid, eosinophilic | |
| Host reaction | Fibrinous Suppurative | According to dominant component of exudate |
Patchy consolidation — often several lobes or bilateral
Centred on bronchioles or bronchi
Usually in infancy or old age
Usually secondary to preexisting disease
Bronchopneumonia has a characteristic patchy distribution, centred on inflamed bronchioles and bronchi with subsequent spread to surrounding alveoli (see Fig. 14.6A ). It occurs most commonly in old age, in infancy and in patients with debilitating diseases, such as cancer, cardiac failure, chronic renal failure or cerebrovascular disease. Bronchopneumonia may also occur in patients with acute bronchitis, COPD or cystic fibrosis. Failure to clear respiratory secretions, such as is common in the postoperative period, also predisposes to the development of bronchopneumonia.
Typical organisms include staphylococci, streptococci and H. influenzae . Patients often become septicaemic and toxic, with fever and reduced consciousness.
Affected areas of the lung tend to be basal and bilateral, and appear focally grey or grey–red at postmortem with pus-filled bronchi ( Fig. 14.7 ). Histology shows typical acute inflammation with exudation in the bronchi and adjacent alveolar spaces. With antibiotics and physiotherapy, the inflammatory process may undergo resolution but healing by organisation or death may occur.

Affects anatomically delineated segment(s) or the entirety, of a lobe or lung
Relatively uncommon in infancy and old age
Affects males more than females
90% due to S. pneumoniae (pneumococcus)
Cough and fever with purulent or ‘rusty’ sputum
Pneumococcal pneumonia typically affects otherwise healthy adults between 20 and 50 years of age; however, lobar pneumonia caused by Klebsiella typically affects the elderly, diabetics or alcoholics. Symptoms include a cough, fever and production of sputum. The sputum appears purulent and may contain flecks of blood, so-called ‘rusty’ sputum. Fever can be very high (over 40°C), with rigors. Acute pleuritic chest pain on deep inspiration reflects inflammation of the pleura (pleurisy). As the lung becomes consolidated ( Fig. 14.8 ), the chest signs are dullness to percussion with bronchial breathing.

The pathology of lobar pneumonia is a classic example of acute inflammation, involving four stages.
Congestion . This first stage lasts for about 24 hours and represents the outpouring of a protein-rich exudate into the alveolar spaces. The lung is heavy, oedematous and red.
Red hepatisation . In this second stage, which lasts for a few days, there is massive accumulation in the alveolar spaces of polymorphs, together with some lymphocytes and macrophages. Many red cells are also extravasated from the distended capillaries. The overlying pleura bears a fibrinous exudate. The lung is red, solid and airless, with a consistency resembling fresh liver.
Grey hepatisation . This third stage also lasts a few days and represents further accumulation of fibrin, with destruction of white cells and red cells. The lung is now grey–brown and solid.
Resolution . This fourth stage occurs at about 8 to 10 days in untreated cases, and represents the resorption of exudate and enzymatic digestion of inflammatory debris, with preservation of the underlying alveolar wall architecture. Most cases of acute lobar pneumonia resolve in this way but infections with some more virulent bacterial organisms may lead to tissue damage and fibrosis or abscess formation (e.g. Staphylococcus aureus , Klebsiella pneumoniae ).
Pneumonias caused by organisms other than traditional bacteria are often referred to as ‘atypical pneumonias’. These may be subclassified into those occurring in nonimmunosuppressed hosts and those occurring in immunosuppressed hosts.
Pneumonia may be due to:
viruses, for example, influenza, RSV and adenovirus
Mycoplasma
Legionnaires disease.
The clinical course of viral pneumonia is varied depending on the extent and severity of the disease. In fatal cases, the lungs appear heavy, red and consolidated, as in adult respiratory distress syndrome (ARDS). Histology shows interstitial inflammation consisting of lymphocytes, macrophages and plasma cells. Hyaline membranes of fibrinous exudate are prominent. The alveoli may be relatively free of cellular exudate. Secondary bacterial infection is, however, common and may be severe, for example staphylococcal pneumonia complicating flu.
Mycoplasma pneumonia tends to cause a more low-grade pneumonia, with interstitial inflammation and less exudation.
Since the first well-described outbreak in 1976, this disease has become increasingly recognised. It is caused by a bacillus, Legionella pneumophila , transmitted in water droplets from contaminated air humidifiers and water cisterns. Patients may be previously well, although a proportion have an underlying chronic illness, such as heart failure or carcinoma. Symptoms include cough, dyspnoea and chest pain, together with more systemic features, such as myalgia, headache, confusion, nausea, vomiting and diarrhoea. About 5% to 20% of cases are fatal depending on the age of the population affected. At autopsy, the lungs are very heavy and consolidated.
Immunosuppression may be relative, as occurs in patients at the extremes of age, diabetics or those who are malnourished as well as those on high-dose steroid therapy, undergoing chemotherapy for malignancy, immunosuppression for transplantation or those with HIV/AIDS infection.
Most lung infections in these patients are with organisms similar to those seen in the general population. Patients with severe immunosuppression are, however, prone to infection with unusual organisms that are usually nonpathogenic in other individuals. These are known as ‘opportunistic’ infections. In any immunosuppressed patient, the onset of fever, shortness of breath and cough, together with pulmonary infiltrates, is an ominous event.
Common ‘opportunistic’ agents include:
Pneumocystis jiroveci
fungi, for example, Candida, Aspergillus
viruses, for example, cytomegalovirus (CMV), herpes simplex virus, varicella-zoster.
Alveoli are filled with a bubbly pink exudate. Round or crescent-shaped organisms are seen using a silver impregnation stain. There may also be diffuse alveolar damage.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here