Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Male reproductive functions can be divided into three major subdivisions: (1) formation of sperm—spermatogenesis; (2) performance of the male sexual act; and (3) regulation of male reproductive functions by the various hormones. Associated with these reproductive functions are the effects of the male sex hormones on the accessory sexual organs, cellular metabolism, growth, and other functions of the body.
Figure 81-1A shows various portions of the male reproductive system, and Figure 81-1B gives a more detailed structure of the testis and epididymis. The testis is composed of up to 900 coiled seminiferous tubules, each averaging more than one-half meter long, in which the sperm are formed. The sperm then empty into the epididymis, which is another coiled tube about 6 meters long. The epididymis leads into the vas deferens, which enlarges into the ampulla of the vas deferens immediately before the vas enters the body of the prostate gland.
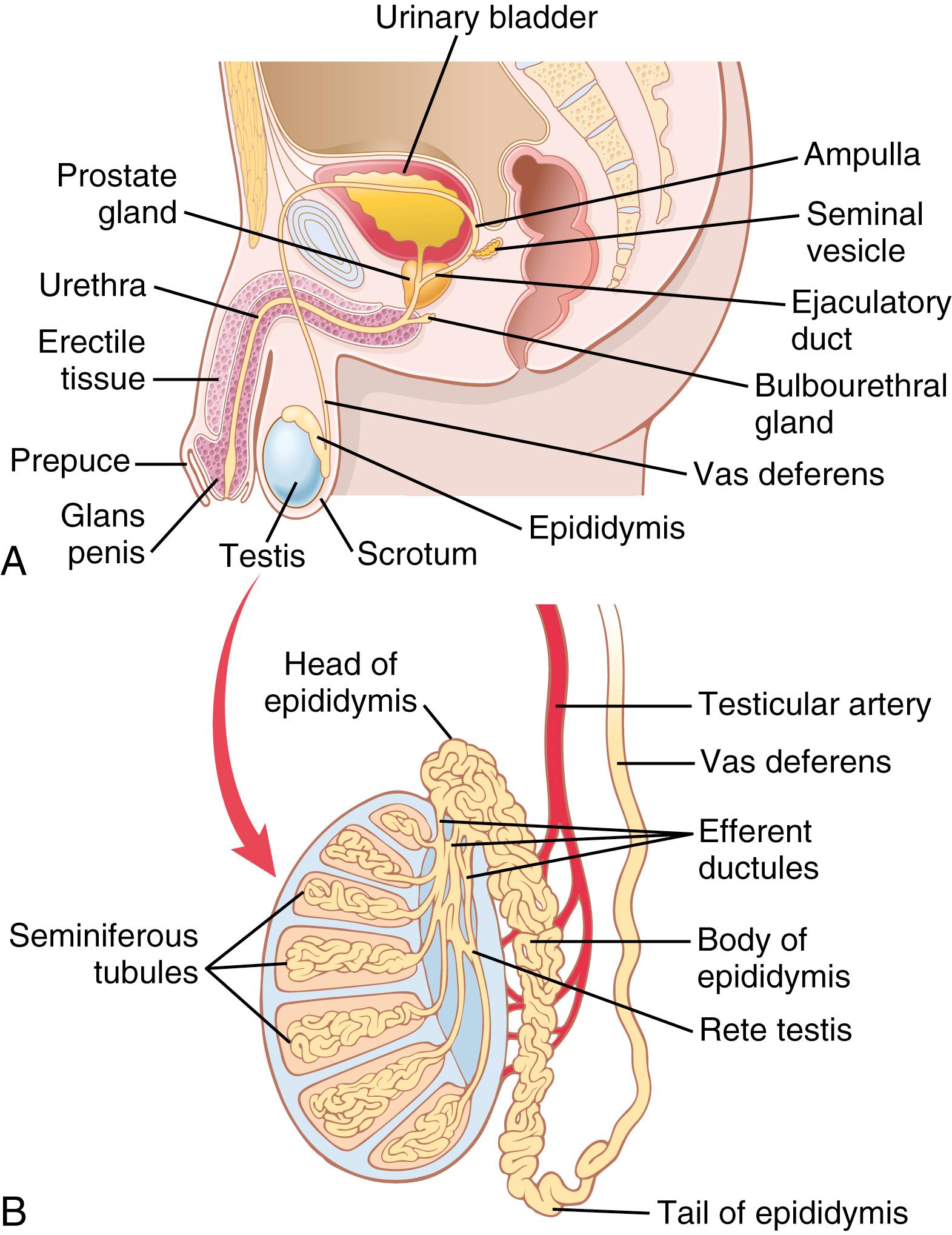
Two seminal vesicles, one located on each side of the prostate, empty into the prostatic end of the ampulla, and the contents from both the ampulla and the seminal vesicles pass into an ejaculatory duct leading through the body of the prostate gland and then emptying into the internal urethra. Prostatic ducts also empty from the prostate gland into the ejaculatory duct and from there into the prostatic urethra.
Finally, the urethra is the last connecting link from the testis to the exterior. The urethra is supplied with mucus derived from a large number of minute urethral glands located along its entire extent and even more so from bilateral bulbourethral glands ( Cowper glands ) located near the origin of the urethra.
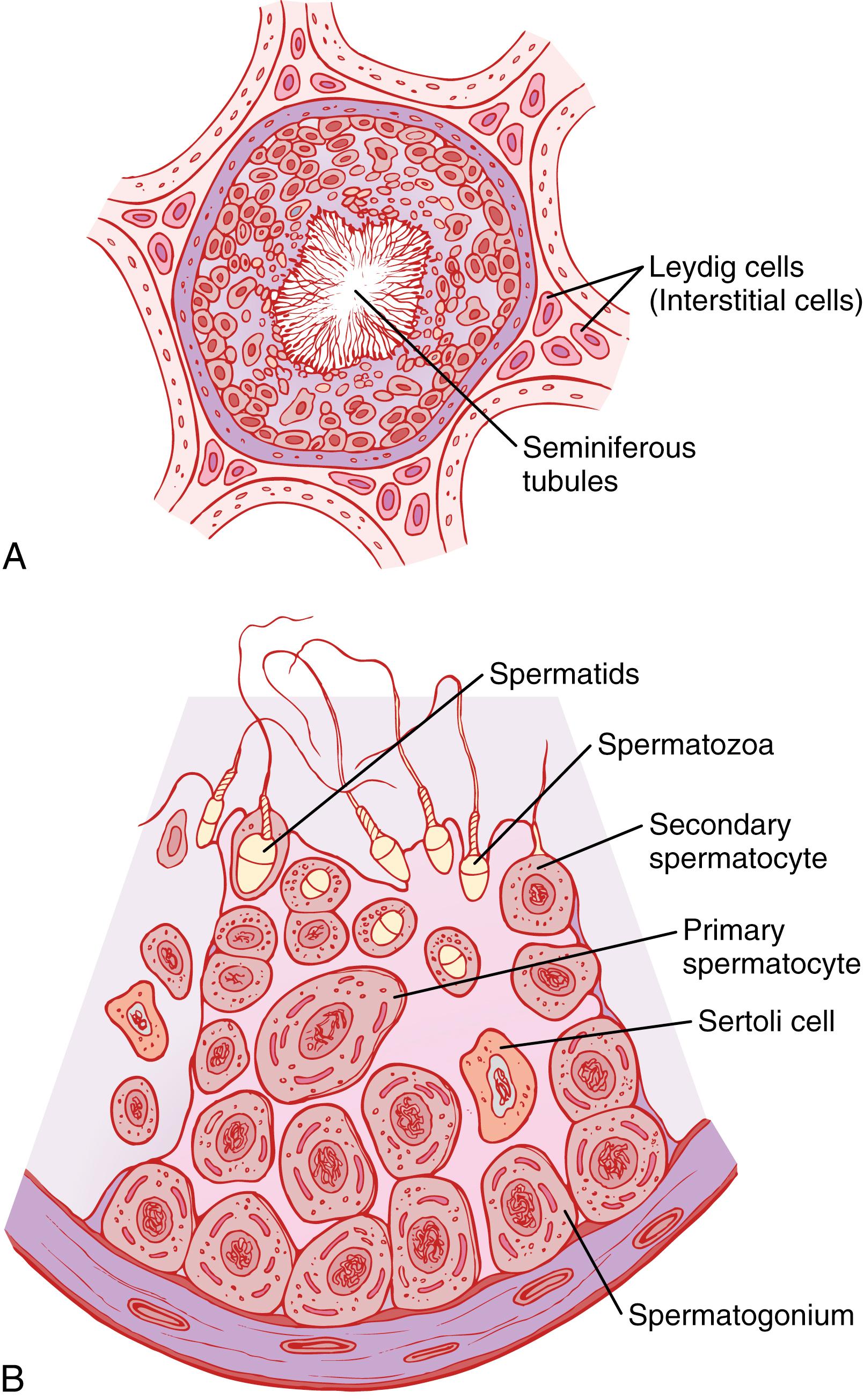
During formation of the embryo, the primordial germ cells migrate into the testes and become immature germ cells called spermatogonia, which lie in two or three layers of the inner surfaces of the seminiferous tubules (a cross section of a tubule is shown in Figure 81-2A ). At puberty the spermatogonia begin to undergo mitotic division and continually proliferate and differentiate through definite stages of development to form sperm, as shown in Figure 81-2B .
Spermatogenesis occurs in the seminiferous tubules during active sexual life as the result of stimulation by anterior pituitary gonadotropic hormones. Spermatogenesis begins in the male at an average age of 13 years and continues throughout most of the remainder of life but decreases markedly in old age.
In the first stage of spermatogenesis, the spermatogonia migrate among Sertoli cells toward the central lumen of the seminiferous tubule. The Sertoli cells are large, with overflowing cytoplasmic envelopes that surround the developing spermatogonia all the way to the central lumen of the tubule.
Spermatogonia that cross the barrier into the Sertoli cell layer become progressively modified and enlarged to form large primary spermatocytes ( Figure 81-3 ) . Each of these primary spermatocytes, in turn, undergoes meiotic division to form two secondary spermatocytes. After another few days, these secondary spermatocytes also divide to form spermatids that are eventually modified to become spermatozoa (sperm).
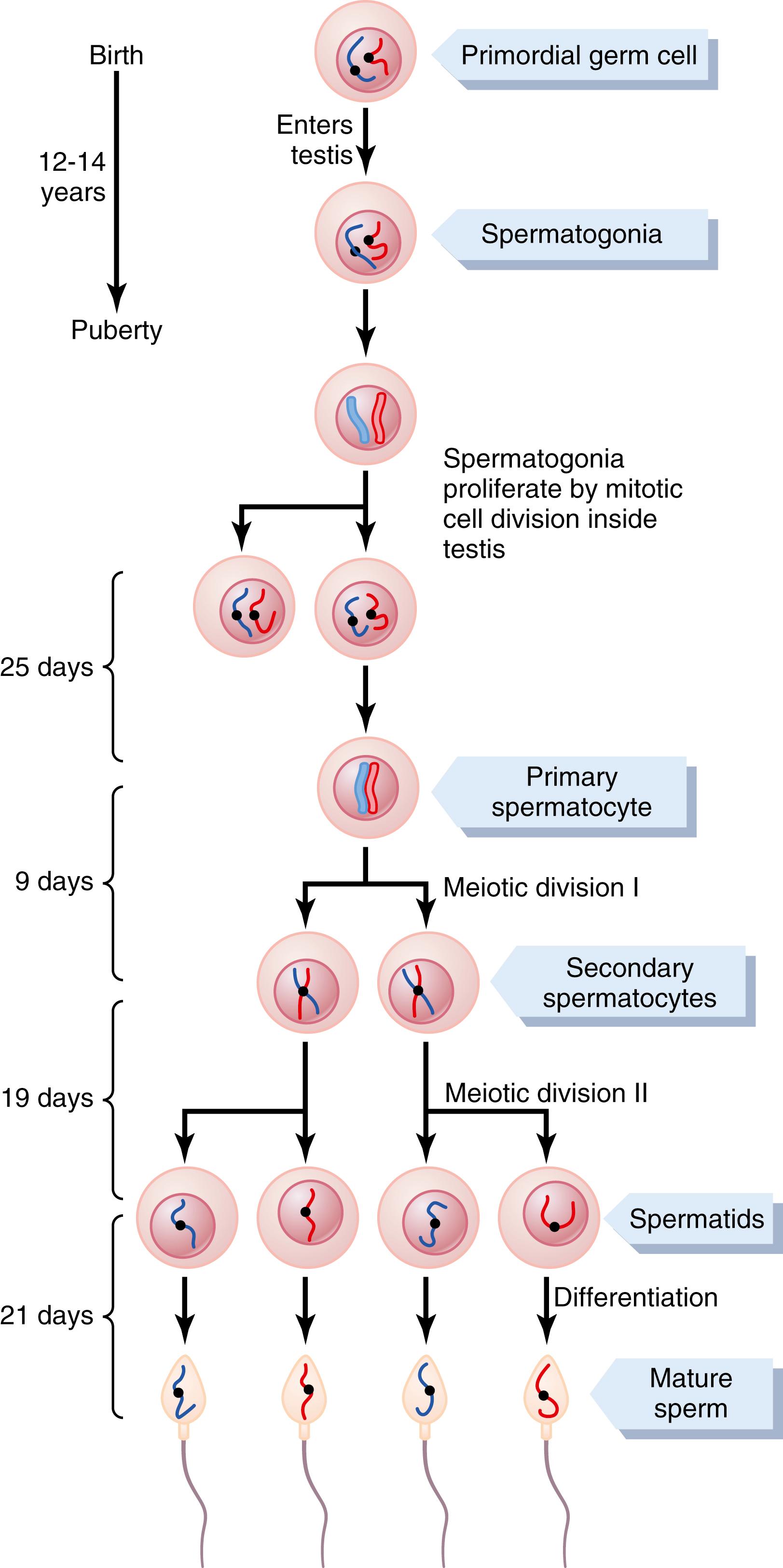
During the change from the spermatocyte stage to the spermatid stage, the 46 chromosomes (23 pairs of chromosomes) of the spermatocyte are divided, and thus 23 chromosomes go to one spermatid and the other 23 go to the second spermatid. The chromosomal genes are also divided so that only one-half of the genetic characteristics of the eventual fetus are provided by the father, with the other half being derived from the oocyte provided by the mother.
The entire period of spermatogenesis, from spermatogonia to spermatozoa, takes about 74 days.
In each spermatogonium, one of the 23 pairs of chromosomes carries the genetic information that determines the sex of each eventual offspring. This pair is composed of one X chromosome, which is called the female chromosome, and one Y chromosome, the male chromosome. During meiotic division, the male Y chromosome goes to one spermatid that then becomes a male sperm, and the female X chromosome goes to another spermatid that becomes a female sperm. The sex of the eventual offspring is determined by which of these two types of sperm fertilizes the ovum. This process is discussed further in Chapter 83 .
When the spermatids are first formed, they still have the usual characteristics of epithelioid cells, but soon they begin to differentiate and elongate into spermatozoa. As shown in Figure 81-4 , each spermatozoon is composed of a head and a tail . The head comprises the condensed nucleus of the cell, with only a thin cytoplasmic and cell membrane layer around its surface. On the outside of the anterior two-thirds of the head is a thick cap called the acrosome that is formed mainly from the Golgi apparatus. The acrosome contains several enzymes similar to those found in lysosomes of the typical cell, including hyaluronidase (which can digest proteoglycan filaments of tissues) and powerful proteolytic enzymes (which can digest proteins). These enzymes play important roles in allowing the sperm to enter the ovum and fertilize it.
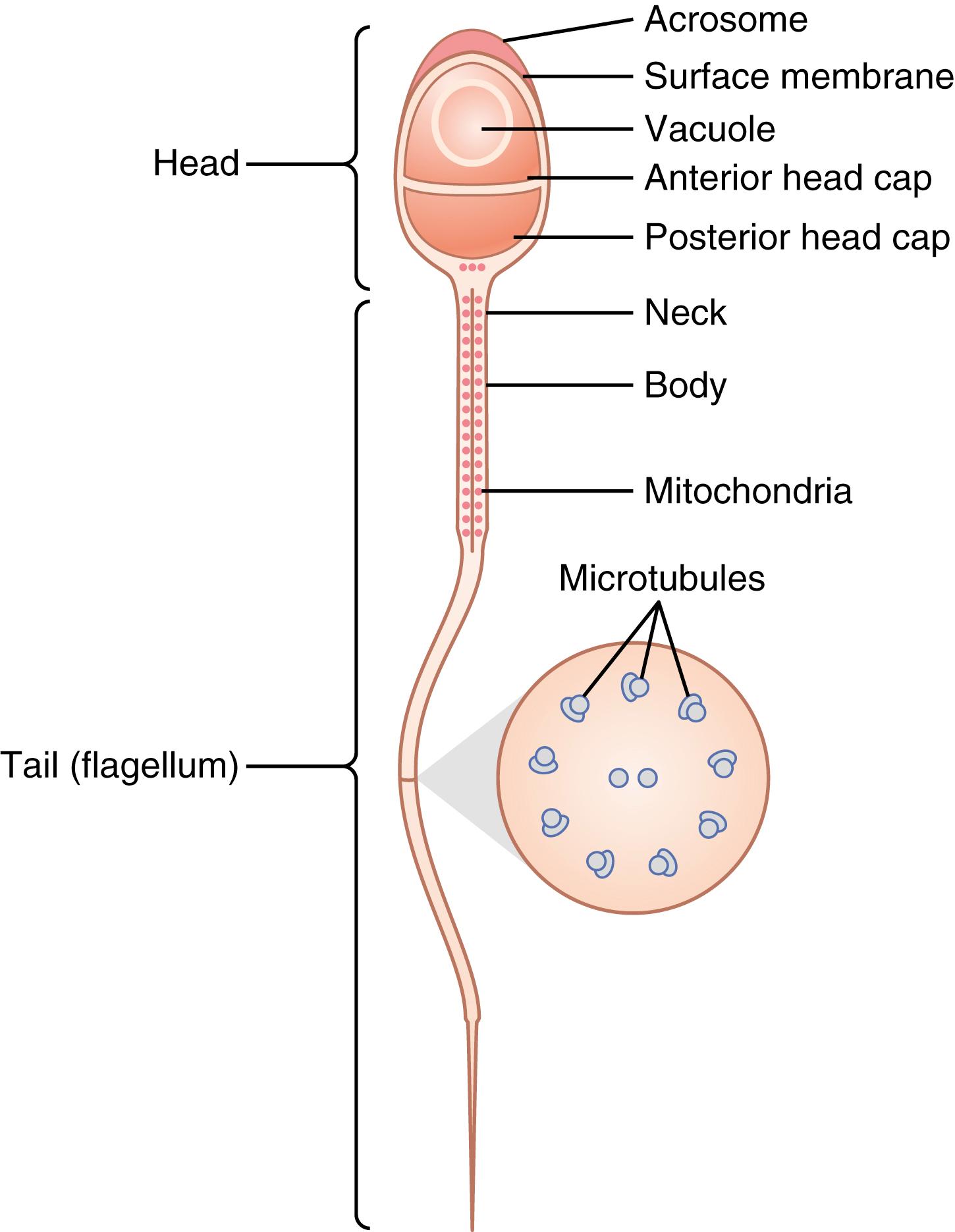
The tail of the sperm, called the flagellum, has three major components: (1) a central skeleton constructed of 11 microtubules, collectively called the axoneme ; the structure of the axoneme is similar to that of cilia found on the surfaces of other types of cells described in Chapter 2 ; (2) a thin cell membrane covering the axoneme; and (3) a collection of mitochondria surrounding the axoneme in the proximal portion of the tail, called the body of the tail .
Back-and-forth movement of the tail (flagellar movement) provides motility for the sperm. This movement results from a rhythmic longitudinal sliding motion between the anterior and posterior tubules that make up the axoneme. The energy for this process is supplied in the form of adenosine triphosphate, which is synthesized by the mitochondria in the body of the tail.
Normal sperm move in a fluid medium at a velocity of 1 to 4 mm/min, which allows them to move through the female genital tract in quest of the ovum.
The role of hormones in reproduction is discussed later in detail; for now, note that several hormones play essential roles in spermatogenesis. Some of these roles are as follows:
Testosterone, secreted by the Leydig cells located in the interstitium of the testis (see Figure 81-2 ), is essential for growth and division of the testicular germinal cells, which is the first stage in forming sperm.
Luteinizing hormone, secreted by the anterior pituitary gland, stimulates the Leydig cells to secrete testosterone.
Follicle-stimulating hormone, also secreted by the anterior pituitary gland, stimulates the Sertoli cells; without this stimulation, conversion of the spermatids to sperm (the process of spermiogenesis) will not occur.
Estrogens, formed from testosterone by the Sertoli cells when they are stimulated by follicle-stimulating hormone, are probably also essential for spermiogenesis.
Growth hormone (as well as most of the other body hormones) is necessary for controlling background metabolic functions of the testes. Growth hormone specifically promotes early division of the spermatogonia; in its absence, as in pituitary dwarfs, spermatogenesis is severely deficient or absent, thus causing infertility.
After formation in the seminiferous tubules, the sperm require several days to pass through the 6-meter-long tubule of the epididymis. Sperm removed from the seminiferous tubules and from the early portions of the epididymis are nonmotile and cannot fertilize an ovum. However, after the sperm have been in the epididymis for 18 to 24 hours, they develop the capability of motility, even though several inhibitory proteins in the epididymal fluid still prevent final motility until after ejaculation.
The two testes of the human adult form up to 120 million sperm each day. Most of these sperm are stored in the epididymis, although a small quantity is stored in the vas deferens. They can remain stored, while maintaining their fertility, for at least a month. During this time, they are kept in a deeply suppressed, inactive state by multiple inhibitory substances in the secretions of the ducts. Conversely, with a high level of sexual activity and ejaculations, they may be stored no longer than a few days.
After ejaculation, the sperm become motile and capable of fertilizing the ovum, a process called maturation. The Sertoli cells and the epithelium of the epididymis secrete a special nutrient fluid that is ejaculated along with the sperm. This fluid contains hormones (including both testosterone and estrogens), enzymes, and special nutrients that are essential for sperm maturation.
The normal motile, fertile sperm are capable of flagellated movement through the fluid medium at velocities of 1 to 4 mm/min. The activity of sperm is greatly enhanced in a neutral and slightly alkaline medium, as exists in the ejaculated semen, but it is greatly depressed in a mildly acidic medium. A strong acidic medium can cause the rapid death of sperm.
The activity of sperm increases markedly with increasing temperature, but so does the rate of metabolism, causing the life of the sperm to be considerably shortened. Although sperm can live for many weeks in the suppressed state in the genital ducts of the testes, the life expectancy of ejaculated sperm in the female genital tract is only 1 to 2 days.
Each seminal vesicle is a tortuous, loculated tube lined with a secretory epithelium that secretes a mucoid material containing an abundance of fructose, citric acid, and other nutrient substances, as well as large quantities of prostaglandins and fibrinogen. During the process of emission and ejaculation, each seminal vesicle empties its contents into the ejaculatory duct shortly after the vas deferens empties the sperm. This action adds greatly to the bulk of the ejaculated semen, and the fructose and other substances in the seminal fluid are of considerable nutrient value for the ejaculated sperm until one of the sperm fertilizes the ovum.
Prostaglandins are believed to aid fertilization in two ways: (1) by reacting with the female cervical mucus to make it more receptive to sperm movement and (2) by possibly causing backward, reverse peristaltic contractions in the uterus and fallopian tubes to move the ejaculated sperm toward the ovaries (a few sperm reach the upper ends of the fallopian tubes within 5 minutes).
The prostate gland secretes a thin, milky fluid that contains calcium, citrate ion, phosphate ion, a clotting enzyme, and a profibrinolysin. During emission, the capsule of the prostate gland contracts simultaneously with the contractions of the vas deferens so that the thin, milky fluid of the prostate gland adds further to the bulk of the semen. A slightly alkaline characteristic of the prostatic fluid may be quite important for successful fertilization of the ovum because the fluid of the vas deferens is relatively acidic owing to the presence of citric acid and metabolic end products of the sperm and, consequently, helps inhibit sperm fertility. Also, the vaginal secretions of the female are acidic (with a pH of 3.5–4.0). Sperm do not become optimally motile until the pH of the surrounding fluids rises to about 6.0 to 6.5. Consequently, it is probable that the slightly alkaline prostatic fluid helps neutralize the acidity of the other seminal fluids during ejaculation and thus enhances the motility and fertility of the sperm.
Semen, which is ejaculated during the male sexual act, is composed of the fluid and sperm from the vas deferens (≈10% of the total), fluid from the seminal vesicles (almost 60%), fluid from the prostate gland (≈30%), and small amounts from the mucous glands, especially the bulbourethral glands. Thus, the bulk of the semen is seminal vesicle fluid, which is the last to be ejaculated and serves to wash the sperm through the ejaculatory duct and urethra.
The average pH of the combined semen is about 7.5, with the alkaline prostatic fluid having more than neutralized the mild acidity of the other portions of the semen. The prostatic fluid gives the semen a milky appearance, and fluid from the seminal vesicles and mucous glands gives the semen a mucoid consistency. Also, a clotting enzyme from the prostatic fluid causes the fibrinogen of the seminal vesicle fluid to form a weak fibrin coagulum that holds the semen in the deeper regions of the vagina where the uterine cervix lies. The coagulum then dissolves during the next 15 to 30 minutes because of lysis by fibrinolysin formed from the prostatic profibrinolysin. In the early minutes after ejaculation, the sperm remain relatively immobile, possibly because of the viscosity of the coagulum. As the coagulum dissolves, the sperm simultaneously become highly motile.
Although sperm can live for many weeks in the male genital ducts, once they are ejaculated in the semen, their maximal life span is only 24 to 48 hours at body temperature. At lowered temperatures, however, semen can be stored for several weeks, and when frozen at temperatures below −100°C, sperm have been preserved for years.
Although spermatozoa are said to be “mature” when they leave the epididymis, their activity is held in check by multiple inhibitory factors secreted by the genital duct epithelia. Therefore, when they are first expelled in the semen, they are unable to fertilize the ovum. However, on coming in contact with the fluids of the female genital tract, multiple changes occur that activate the sperm for the final processes of fertilization. These collective changes are called capacitation of the spermatozoa, which normally requires from 1 to 10 hours. The following changes are believed to occur:
The uterine and fallopian tube fluids wash away the various inhibitory factors that suppress sperm activity in the male genital ducts.
While the spermatozoa remain in the fluid of the male genital ducts, they are continually exposed to many floating vesicles from the seminiferous tubules containing large amounts of cholesterol. This cholesterol is continually added to the cellular membrane covering the sperm acrosome, toughening this membrane and preventing release of its enzymes. After ejaculation, the sperm deposited in the vagina swim away from the cholesterol vesicles upward into the uterine cavity, and they gradually lose much of their other excess cholesterol during the next few hours. In so doing, the membrane at the head of the sperm (the acrosome) becomes much weaker.
The membrane of the sperm also becomes much more permeable to calcium ions, so calcium now enters the sperm in abundance and changes the activity of the flagellum, giving it a powerful whiplash motion in contrast to its previously weak undulating motion. In addition, the calcium ions cause changes in the cellular membrane that cover the leading edge of the acrosome, making it possible for the acrosome to release its enzymes rapidly and easily as the sperm penetrates the granulosa cell mass surrounding the ovum, and even more so as it attempts to penetrate the zona pellucida of the ovum.
Thus, multiple changes occur during the process of capacitation. Without these changes, the sperm cannot make its way to the interior of the ovum to cause fertilization.
Stored in the acrosome of the sperm are large quantities of hyaluronidase and proteolytic enzymes. Hyaluronidase depolymerizes the hyaluronic acid polymers in the intercellular cement that holds the ovarian granulosa cells together. The proteolytic enzymes digest proteins in the structural elements of tissue cells that still adhere to the ovum.
When the ovum is expelled from the ovarian follicle into the fallopian tube, it still carries with it multiple layers of granulosa cells. Before a sperm can fertilize the ovum, it must dissolute these granulosa cell layers, and then it must penetrate through the zona pellucida , the thick covering of the ovum . To achieve this penetration, the stored enzymes in the acrosome begin to be released. The hyaluronidase among these enzymes is especially important in opening pathways between the granulosa cells so that the sperm can reach the ovum.
When the sperm reaches the zona pellucida of the ovum, the anterior membrane of the sperm binds specifically with receptor proteins in the zona pellucida. Next, the entire acrosome rapidly dissolves, and all the acrosomal enzymes are released. Within minutes, these enzymes open a penetrating pathway for passage of the sperm head through the zona pellucida to the inside of the ovum. Within another 30 minutes, the cell membranes of the sperm head and of the oocyte fuse with each other to form a single cell. At the same time, the genetic material of the sperm and the oocyte combine to form a completely new cell genome, containing equal numbers of chromosomes and genes from mother and father. This is the process of fertilization; the embryo then begins to develop, as discussed in Chapter 83 .
With as many sperm as there are, why does only one enter the oocyte? The reason is not entirely known, but within a few minutes after the first sperm penetrates the zona pellucida of the ovum, calcium ions diffuse inward through the oocyte membrane and cause multiple cortical granules to be released by exocytosis from the oocyte into the perivitelline space. These granules contain substances that permeate all portions of the zona pellucida and prevent binding of additional sperm, and they even cause any sperm that have already begun to bind to fall off. Thus, almost never does more than one sperm enter the oocyte during fertilization.
The seminiferous tubular epithelium can be destroyed by several diseases. For example, bilateral orchitis (inflammation) of the testes resulting from mumps causes sterility in some affected males. Also, some male infants are born with degenerate tubular epithelia as a result of strictures in the genital ducts or other abnormalities. Finally, another cause of sterility, usually temporary, is excessive temperature of the testes.
Increasing the temperature of the testes can prevent spermatogenesis by causing degeneration of most cells of the seminiferous tubules besides the spermatogonia. It has often been stated that the reason the testes are located in the dangling scrotum is to maintain the temperature of these glands below the internal temperature of the body, although usually only about 2°C below the internal temperature. On cold days, scrotal reflexes cause the musculature of the scrotum to contract, pulling the testes close to the body to maintain this 2°C differential. Thus, the scrotum acts as a cooling mechanism for the testes (but a controlled cooling), without which spermatogenesis might be deficient during hot weather.
Cryptorchidism means failure of a testis to descend from the abdomen into the scrotum at or near the time of birth of a fetus. During development of the male fetus, the testes are derived from the genital ridges in the abdomen. However, at about 3 weeks to 1 month before birth of the baby, the testes normally descend through the inguinal canals into the scrotum. Occasionally this descent does not occur or occurs incompletely, and as a result one or both testes remain in the abdomen, in the inguinal canal, or elsewhere along the route of descent.
A testis that remains in the abdominal cavity throughout life is incapable of forming sperm. The tubular epithelium becomes degenerate, leaving only the interstitial structures of the testis. It has been claimed that even the few degrees higher temperature in the abdomen than in the scrotum is sufficient to cause this degeneration of the tubular epithelium and, consequently, to cause sterility, although this effect is not certain. Nevertheless, for this reason, operations to relocate the cryptorchid testes from the abdominal cavity into the scrotum before the beginning of adult sexual life can be performed on boys who have undescended testes.
Testosterone secretion by the fetal testes is the normal stimulus that causes the testes to descend into the scrotum from the abdomen. Therefore, many, if not most, cases of cryptorchidism are caused by abnormally formed testes that are unable to secrete enough testosterone. The surgical operation for cryptorchidism in these patients is unlikely to be successful.
The usual quantity of semen ejaculated during each coitus averages about 3.5 milliliters, and each milliliter of semen contains an average of about 120 million sperm, although even in “normal” males this quantity can vary from 35 million to 200 million. This means an average total of about 400 million sperm are usually present in the several milliliters of each ejaculate. When the number of sperm in each milliliter falls below about 20 million, the person is likely to be infertile. Thus, even though only a single sperm is necessary to fertilize the ovum, for reasons that are not understood, the ejaculate usually must contain a tremendous number of sperm for only one sperm to fertilize the ovum.
Occasionally, a man has a normal number of sperm but is still infertile. When this situation occurs, sometimes as many as one-half of the sperm are found to be abnormal physically, having two heads, abnormally shaped heads, or abnormal tails, as shown in Figure 81-5 . At other times, the sperm appear to be structurally normal, but for reasons not understood, they are either entirely nonmotile or relatively nonmotile. Whenever most of the sperm are morphologically abnormal or are nonmotile, the person is likely to be infertile, even though the remainder of the sperm appear to be normal.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here