Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The labia majora are homologous to the scrotum in the man. The labia minora are homologous to the penile urethra and a portion of the skin of the penis in men.
The clitoris complex is composed of both erectile and nonerectile tissue and includes the glans, prepuce, body, crura, bulbs, suspensory ligament, and the root.
The clitoral complex is the female homologue of the penis in the man and is a critical organ responsible for sexual arousal, function, and sexual health.
The female urethra measures 3.5 to 5 cm long. The mucosa of the proximal two-thirds of the urethra is composed of stratified transitional epithelium, and the distal one-third is stratified squamous epithelium.
When a woman is standing, the axis of the upper portion of the vagina lies close to the horizontal plane, with the upper portion of the vagina curving toward the hollow of the sacrum.
The vaginal length increases with weight and height, and it decreases with age.
The lower third of the vagina is in close anatomic relationship with the urogenital and pelvic diaphragms.
The middle third of the vagina is supported by the levator ani muscles and the lower portion of the cardinal ligaments.
The primary lymphatic drainage of the upper third of the vagina is to the external iliac nodes, the middle third of the vagina drains to the common and internal iliac nodes, and the lower third has a wide lymphatic distribution, including the common iliac, superficial inguinal, and perirectal nodes.
Descriptive terms for pelvic organs are derived from the Latin root, whereas terms relating to surgical procedures are derived from the Greek root.
The length and width of the endocervical canal vary. The width of the canal varies with the parity of the woman and changing hormonal levels. It is usually 2.5 to 3 cm long and 7 to 8 mm at its widest point.
The fibromuscular cervical stroma is composed primarily of collagenous connective tissue and ground substance. The connective tissue contains approximately 15% smooth muscle cells and a small amount of elastic tissue.
The major arterial supply to the cervix is located in the lateral cervical walls at the 3 and 9 o’clock positions.
The pain fibers from the cervix accompany the parasympathetic fibers to the second, third, and fourth sacral segments.
The transformation zone of the cervix encompasses the border of the squamous epithelium and columnar epithelium. The location of the transformation zone changes on the cervix depending on a woman’s hormonal status.
The uterus of a nulliparous woman is approximately 8 cm long, 5 cm wide, and 2.5 cm thick and weighs 40 to 50 g. In contrast, in a multiparous woman each measurement is approximately 1.2 cm larger and normal uterine weight is 20 to 30 g heavier. The maximal weight of a normal uterus is 110 g.
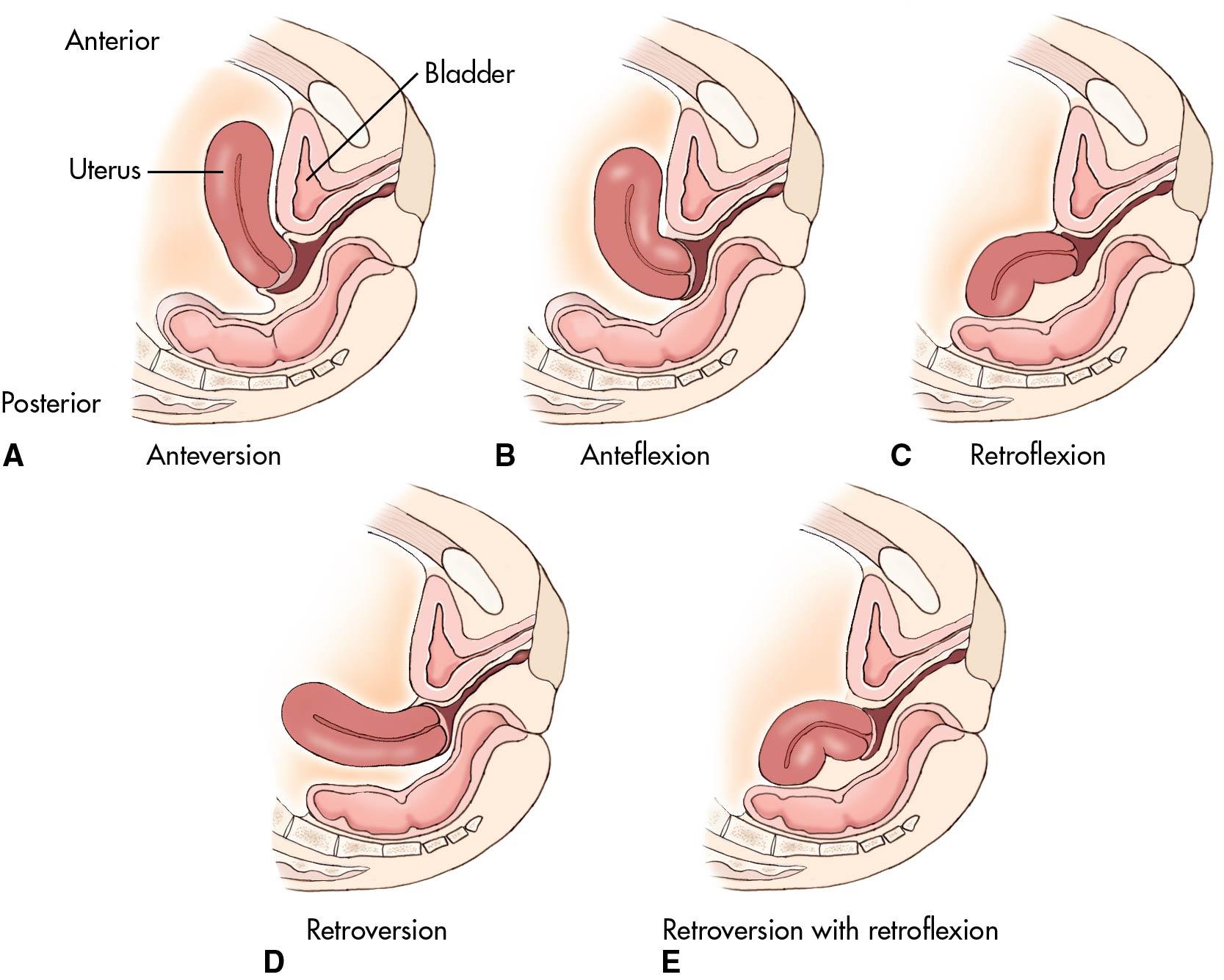
In the majority of women the long axis of the uterus is both anteverted in respect to the long axis of the vagina and anteflexed in relation to the long axis of the cervix. However, a retroflexed uterus is a normal variant found in approximately 25% of women.
The uterine and ovarian arteries provide the arterial blood supply of the uterus. The uterine arteries are large branches of the anterior division of the hypogastric arteries, whereas the ovarian arteries originate directly from the aorta.
Afferent nerve fibers from the uterus enter the spinal cord at the eleventh and twelfth thoracic segments.
The fallopian tubes are 10 to 14 cm long and are composed of four anatomic sections. Closest to the uterine cavity is the interstitial segment, followed by the narrow isthmic segment, then the wider ampullary segment, and distally the trumpet-shaped infundibular segment.
The right fallopian tube and appendix are often anatomically adjacent. Clinically it may be difficult to differentiate inflammation of the upper portion of the genital tract and acute appendicitis.
During the reproductive years, the ovaries measure approximately 1.5 cm × 2.5 cm × 4 cm.
The ovary in nulliparous women rests in a depression of peritoneum named the fossa ovarica. Immediately adjacent to the ovarian fossa are the external iliac vessels, the ureter, and the obturator vessels and nerves.
Three prominent ligaments determine the anatomic mobility of the ovary: the mesovarian, the ovarian ligament, and the infundibulopelvic ligament.
The arterial supply of the pelvis is paired, bilateral, and has multiple collaterals and numerous anastomoses.
The extent of collateral circulation after hypogastric artery ligation depends on the site of ligation and may be divided into three groups: branches from the aorta, branches from the external iliac arteries, and branches from the femoral arteries.
The internal iliac nodes are found in an anatomic triangle whose sides are composed of the external iliac artery, the hypogastric artery, and the pelvic sidewall. This rich collection of nodes receives channels from every internal pelvic organ and the vulva, including the clitoris and urethra.
The femoral triangle is the anatomic space lying immediately distal to the fold of the groin. The boundaries of the femoral triangle are the sartorius and adductor longus muscles and the inguinal ligament.
The pudendal nerve and its branches supply the majority of both motor and sensory fibers to the muscles and skin of the vulvar region.
The femoral nerve may be compromised by pressure on the psoas muscle during abdominal surgery and by hyperflexion of the leg during vaginal surgery.
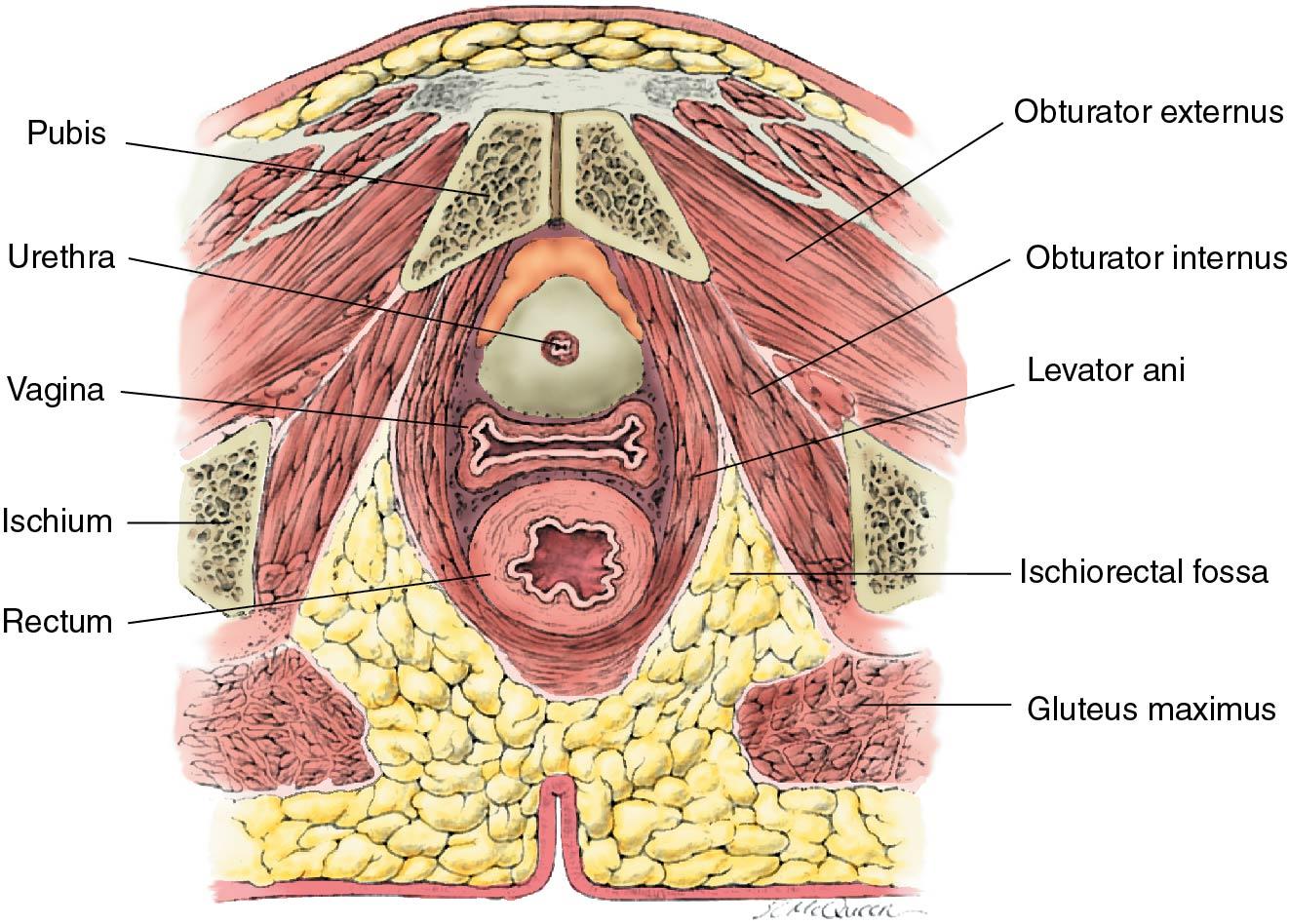
The pelvic diaphragm is important in supporting both abdominal and pelvic viscera and facilitates equal distribution of intraabdominal pressure during activities such as coughing. The levator ani muscles constitute the greatest bulk of the pelvic diaphragm.
The major function of the urogenital diaphragm is to support the urethra and maintain the urethrovesical junction.
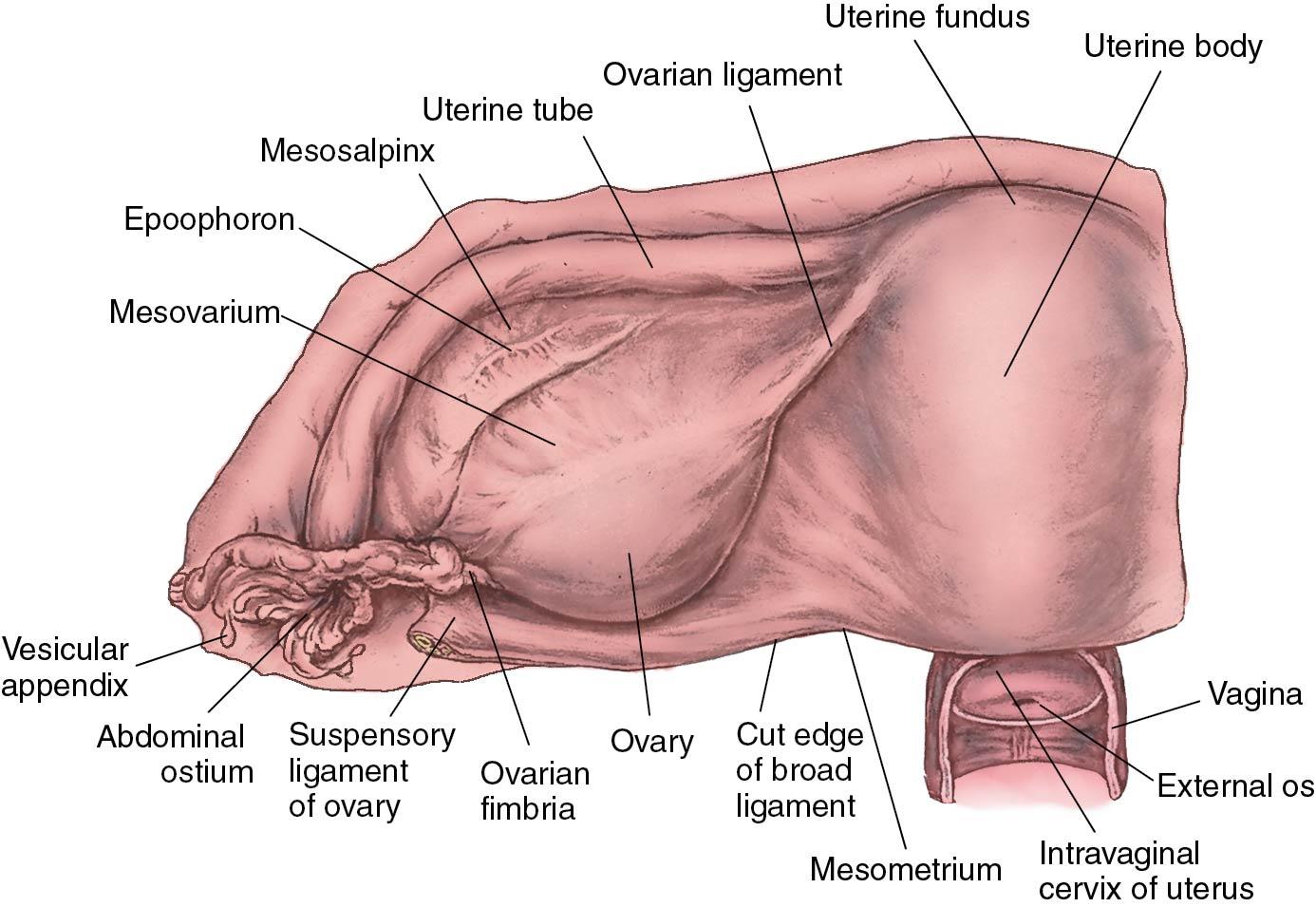
Contained within the broad ligaments are the following structures: oviducts, ovarian and round ligaments, ureters, ovarian and uterine arteries and veins, parametrial tissue, embryonic remnants of the mesonephric duct and Wolffian body, and two secondary ligaments.
The cardinal ligaments provide the major support to the uterus.
A congenital anomaly of a double, or bifid, ureter occurs in 1% to 4% of women.
When the urinary bladder is empty, the ureteral orifices are approximately 2.5 cm apart. This distance increases to 5 cm when the bladder is distended.
The distal ureter enters into the cardinal ligament. In this location the ureter is approximately 1 to 2 cm lateral to the uterine cervix and is surrounded by a plexus of veins. In approximately 12% of women, the cervix will be less than 0.5 cm from the cervix.
Two ways of distinguishing the ureter from pelvic vessels are (1) identification of peristalsis after stimulation with a surgical instrument and (2) identification of Auerbach plexuses.
Surgical compromise of the ureters may occur during clamping or ligating of the infundibulopelvic vessels, clamping or ligating of the cardinal ligaments, or wide suturing in the endopelvic fascia during an anterior repair.
The following three important axioms should be in the forefront of decision making during difficult gynecologic surgery: (1) Do not assume that the anatomy of the left and right side of the pelvis are invariably identical mirror images; (2) during difficult operations with multiple adhesions, operate from known anatomic areas into the unknown; and (3) from the sage advice of a distinguished Canadian gynecologist, Dr. Henry McDuff: “If the disease be rampant and the anatomy obscure, and the plans of dissection not pristine and pure, do not be afraid, nor faint of heart, try the retroperitoneum, it’s a great place to start.”
Accompanying videos for this chapter are available on ExpertConsult.com .
The organs of the female reproductive tract are classically divided into the external and the internal genitalia. The external genital organs are present in the perineal area and include the mons pubis, clitoris, urinary meatus, labia majora, labia minora, vestibule, Bartholin glands, and periurethral glands. The internal genital organs are located in the true pelvis and include the vagina, uterus, cervix, oviducts, ovaries, and surrounding supporting structures. This chapter integrates the basic anatomy of the female pelvis with clinical situations.
Embryologically, the urinary, reproductive, and gastrointestinal tracts develop in close proximity. This relationship continues throughout a woman’s life span. In adults the reproductive organs are in intimate contact with the lower urinary tract and large intestines. Because of the anatomic proximity of the genital and urinary systems, altered pathophysiology in one organ often produces symptoms in an adjacent organ. The gynecologic surgeon should master the intricacy of these anatomic relationships to avoid surgical complications. The clinician must also appreciate that wide individual differences in anatomic detail exist among patients. Understanding these variations is one of the greatest challenges of clinical medicine.
This chapter focuses on the norms of human anatomy; it does not duplicate the completeness of an anatomic text or surgical atlas.
The vulva, or pudendum, is a collective term for the external genital organs that are visible in the perineal area. The vulva consists of the following: the mons pubis, labia majora, labia minora, hymen, clitoris, vestibule, urethra, Skene glands, Bartholin glands, and vestibular bulbs ( Fig. 3.1 ).
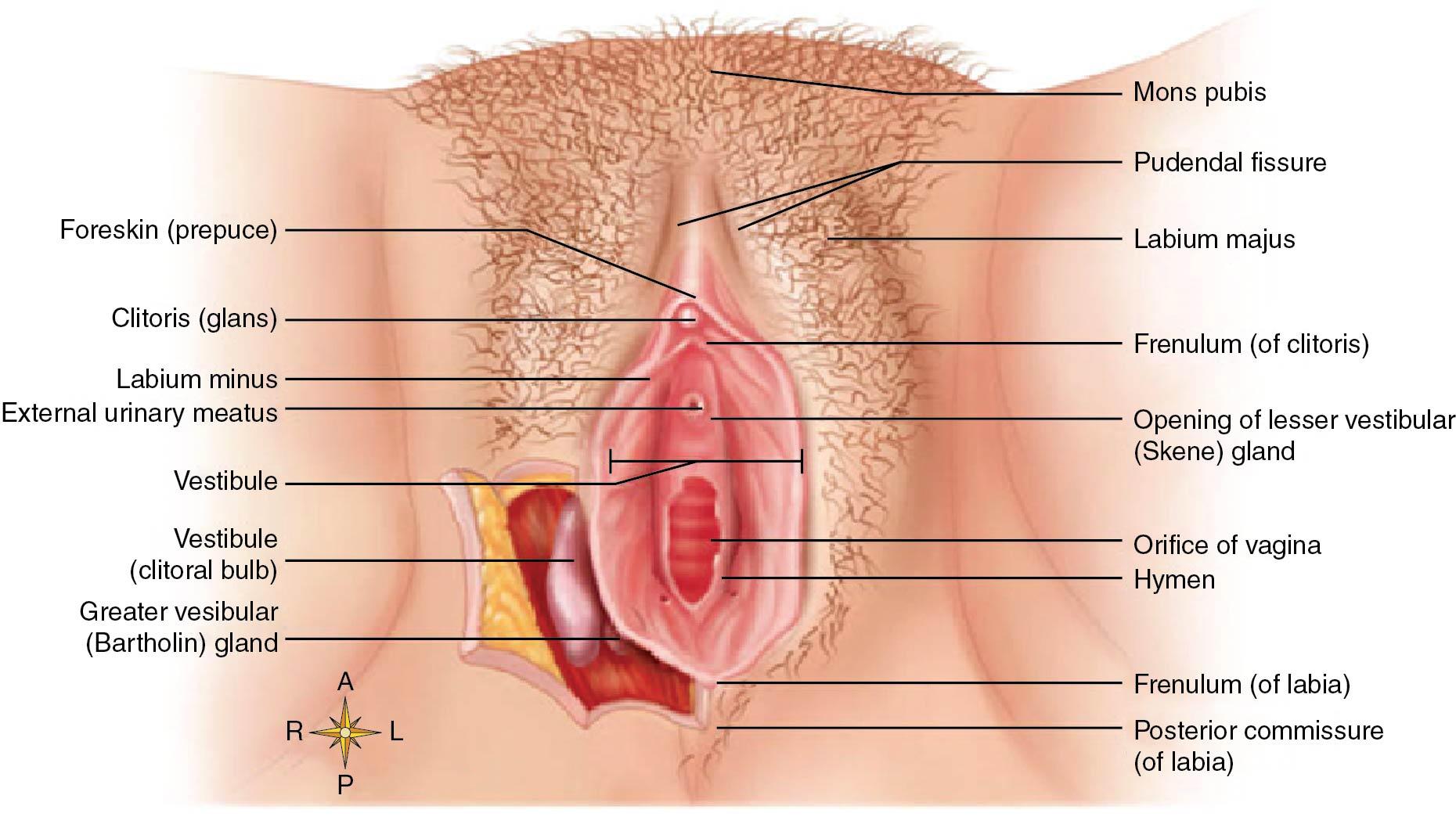
The boundaries of the vulva extend from the mons pubis anteriorly to the rectum posteriorly and from one lateral genitocrural fold to the other. The entire vulvar area is covered by keratinized , stratified squamous epithelium. The skin becomes thicker, more pigmented, and more keratinized as the distance from the vagina increases.
The mons pubis is a fatty, rounded eminence that develops hair after puberty. It is directly anterior and superior to the symphysis pubis. The hair pattern, or escutcheon , of most women is triangular. Genetic and racial differences produce a variety of normal hair patterns, with approximately one in four women having a modified escutcheon that has a diamond (male-like) pattern.
The labia majora are two large, longitudinal, cutaneous folds of adipose and fibrous tissue. Each labium majus is approximately 7 to 8 cm long and 2 to 3 cm wide. The labia majora are homologous to the scrotum in the man. The labia extend from the mons pubis anteriorly to become lost in the skin between the vagina and the anus in the area of the posterior fourchette. The skin of the outer convex surface of the labia majora is pigmented and covered with hair follicles. The thin skin of the inner surface does not have hair follicles but has many sebaceous glands, making this area at risk for sebaceous cysts. Histologically the labia majora have both sweat and sebaceous glands ( Fig. 3.2 ). Abundant apocrine glands are present in the vulvar area and secrete sweat directly into the hair follicles before the follicle opens onto the skin surface in a similar fashion to those of the breast and axillary areas. The size and contour of the labia are related to fat content. During menopause the labia atrophies as a result of a lack of estrogen, which is no longer produced by the ovary.

The clinical significance of the hair-bearing areas of the vulva is that conditions that involve the skin, such as vulvar intraepithelial neoplasia (VIN), may be found as deep as 3 mm below the surface because they can involve the skin down into the hair shafts. That is not the case in the non–hair-bearing areas, such as the labia minora, where the full thickness of the epidermis is usually no more than 1 mm. Hence, treatment of the non–hair-bearing areas does not have to be any deeper than 1 mm to be effective, whereas treatment of the hair-bearing areas must to be at least 3 mm in depth to cover the potentially deeper skin down the hair shafts.
The labia minora, or nymphae, are two small, red cutaneous folds situated between the labia majora and the vaginal orifice. They are more delicate, shorter, and thinner than the labia majora. Anteriorly they divide at the clitoris to form superiorly the prepuce and inferiorly the frenulum of the clitoris. Histologically they are composed of dense connective tissue with erectile tissue and elastic fibers, rather than adipose tissue. The skin of the labia minora is less cornified and has many sebaceous glands but no hair follicles or sweat glands. The labia minora and the breasts are the only areas of the body rich in sebaceous glands but without hair follicles. Among women of reproductive age, there is considerable variation in the size of the labia minora, and they are relatively more prominent in children and postmenopausal women. The labia minora are homologous to the penile urethra and part of the skin of the penis in men.
The hymen is a thin, usually perforated membrane at the entrance of the vagina. There are many anatomic variations in the structure and shape of the hymen that require surgical resection. Please refer to Chapter 12 for examples of hymenal variants. The hymen histologically is covered by stratified squamous epithelium on both sides and consists of fibrous tissue with a few small blood vessels and lacks innervation. In newborns the hymen is annular in shape and vascular as a result of circulating maternal estrogen. In prepubertal girls the lack of estrogen results in atrophy of the hymen and it becomes friable until puberty, at which point the hormonal influences lead to increased elasticity. During pregnancy this tissue becomes thickened with glycogen. Small tags, or what appear to be nodules of firm fibrous material, termed carunculae myrtiformes, are the remnants of the hymen identified in adult women. The postmenopausal hymen is pale pink and thin from a lack of estrogen.
The clitoris, better known now as the clitoral complex, is a multiplanar structure that contains both erectile and nonerectile tissue ( Fig. 3.3 ).
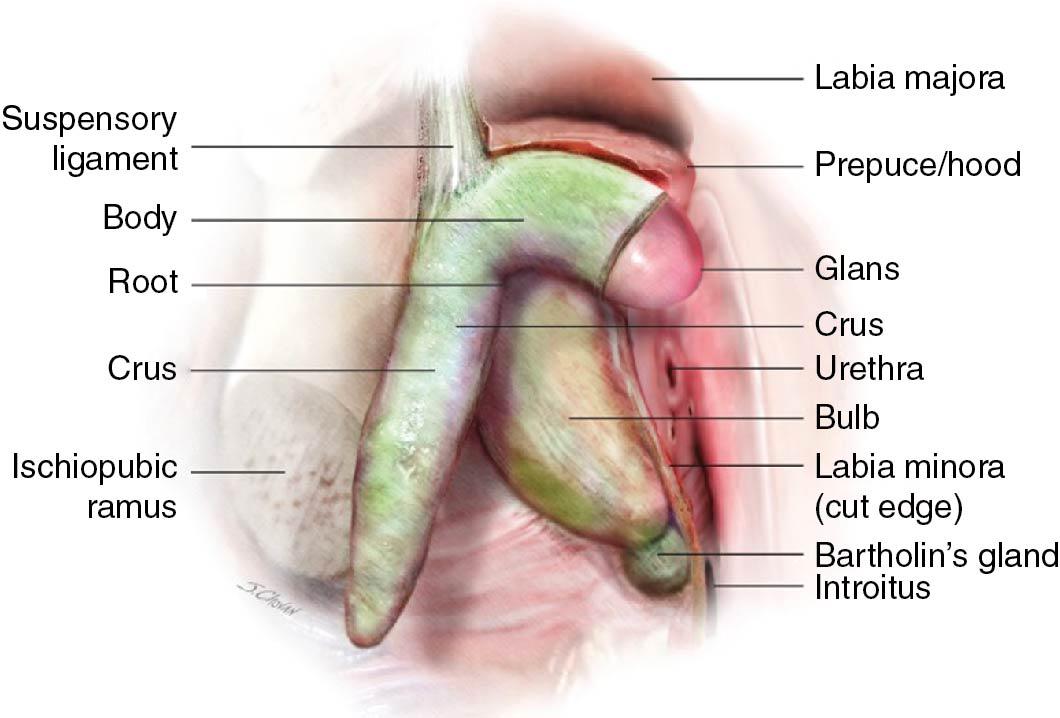
It is located deep to the superficial structures of the vulva and attaches to the pubic arch with supporting tissue at the mons pubic and labia. The complex consists of the glans, prepuce, body, crura, bulbs, suspensory ligament, and root. The visible external portion of the clitoris is composed of nonerectile tissue, known as the glans, and its skin covering, called the prepuce. The average dimensions of the glans are 3.4 mm by 5.1 mm by 16 mm. Parity has been associated with larger glans length and width. However, age, weight, and oral contraceptive use do not change the anatomic dimensions. The erectile portion of the clitoris is composed of paired bulbs, the crura and the body. The bulbs are 4 cm long when flaccid and can engorge up to 7 cm when erect.
The body of the clitoris (1 to 2 cm long) has two cylindrical corpora cavernosa composed of thin-walled tissue, which diverge to form the crura. The bilateral crura attaches to the periosteum of the symphysis pubis and surrounds the urethra. The root is the center of sexual arousal and stimulates the engorgement of the glans. It is in close proximity to the skin surface and the urethral opening and unifies all the erectile tissue essential to sexual function. The clitoral complex is innervated by the dorsal nerve of the clitoris, the pudendal nerve, and the cavernous nerves. The clitoral complex is the female homologue of the penis in the man.
The vestibule is the lowest portion of the embryonic urogenital sinus. It is the cleft distal to the vagina between the labia minora that is visualized when the labia are held apart. The vestibule extends from the clitoris to the posterior fourchette. The orifices of the urethra and vagina and the ducts from the Bartholin glands open into the vestibule. Within the area of the vestibule are the remnants of the hymen and numerous small mucinous glands.
The urethra is a membranous conduit for urine from the urinary bladder to the vestibule. The female urethra measures 3.5 to 5 cm long. The mucosa of the proximal two-thirds of the urethra is composed of stratified transitional epithelium, whereas the distal one-third is stratified squamous epithelium. The distal orifice is 4 to 6 mm in diameter, and the mucosal edges grossly appear everted.
Skene glands, or paraurethral glands, are branched, tubular glands that are adjacent to the distal urethra. Usually Skene ducts run parallel to the long axis of the urethra for approximately 1 cm before opening into the distal urethra, but sometimes the ducts open into the area just outside the urethral orifice. Skene glands are the largest of the paraurethral glands; however, many smaller glands empty into the urethra. Skene glands are homologous to the prostate in the man, and the glands may be involved in sexual stimulation and lubrication for sexual intercourse.
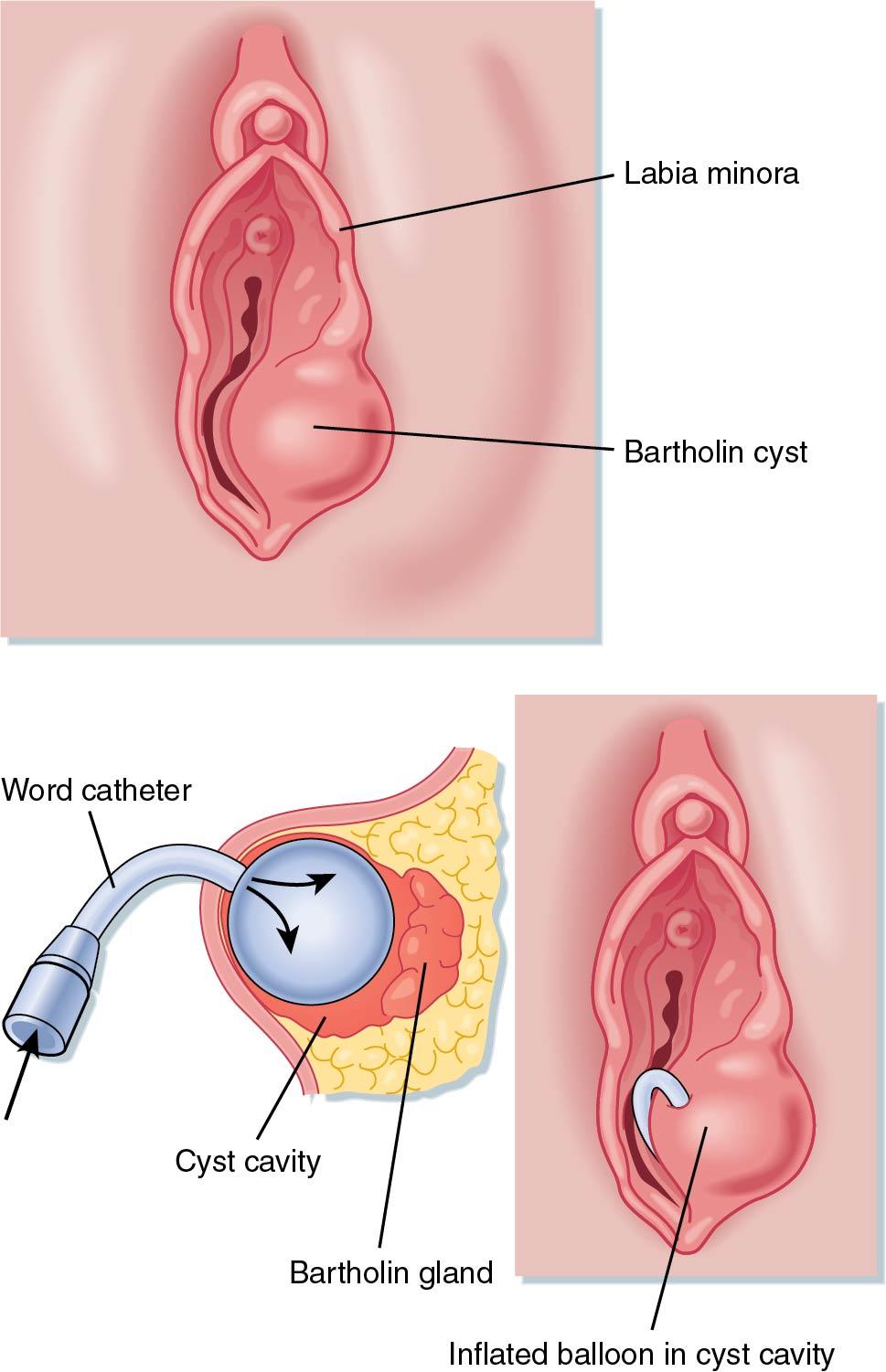
Bartholin glands are vulvovaginal glands located immediately beneath the fascia at about 4 and 8 o’clock, respectively, on the posterolateral aspect of the vaginal orifice. Each lobulated, racemose gland is about the size of a pea. Histologically the gland is composed of cuboidal epithelium. The duct from each gland is lined by transitional epithelium and is approximately 2 cm long. Bartholin ducts open into a groove between the hymen and the labia minora. Bartholin glands are homologous to Cowper glands in the man ( Fig. 3.4 ).

The vestibular bulbs are two elongated masses of erectile tissue situated on either side of the vaginal orifice. Each bulb is immediately below the bulbocavernosus muscle. The distal ends of the vestibular bulbs are adjacent to Bartholin glands. They are homologous to the bulb of the penis in the man.
The skin of the vulvar region is subject to both local and general dermatologic conditions. The intertriginous areas of the vulva remain moist, and obese women are particularly susceptible to chronic infection. The vulvar skin of a postmenopausal woman is sensitive to topical cortisone and testosterone but insensitive to topical estrogen. The most common large cystic structure of the vulva is a Bartholin duct cyst ( Fig. 3.5 ). This condition may become painful if the cyst develops into an acute abscess. The management of Bartholin cysts includes sitz baths, incision and drainage, placement of a Word catheter, antibiotics, and possible marsupialization for chronic infections.
Chronic infections of the periurethral glands may result in one or more urethral diverticula. The most common symptoms of a urethral diverticulum are similar to the symptoms of a lower urinary tract infection: urinary frequency, urgency, and dysuria.
Vulvar trauma such as a straddle injury often results in large hematomas or profuse external hemorrhage. The richness of the vascular supply and the absence of valves in vulvar veins contribute to this complication. The abundant vascularity of the region promotes rapid healing, with an associated low incidence of wound infection in episiotomies or obstetric tears of the vulva. The subcutaneous fatty tissue of the labia majora and mons pubis are in continuity with the fatty tissue of the anterior abdominal wall. When infections such as cellulitis and necrotizing fasciitis occur in this space, they are poorly contained and may rapidly extend in a cephalad direction.
The vagina is a thin-walled, distensible, fibromuscular tube that extends from the vestibule of the vulva to the uterus. The potential space of the vagina is larger in the middle and upper thirds. The walls of the vagina are normally in apposition and flattened in the anteroposterior diameter. Thus the vagina has the appearance of the letter H in cross section ( Fig. 3.6 ).
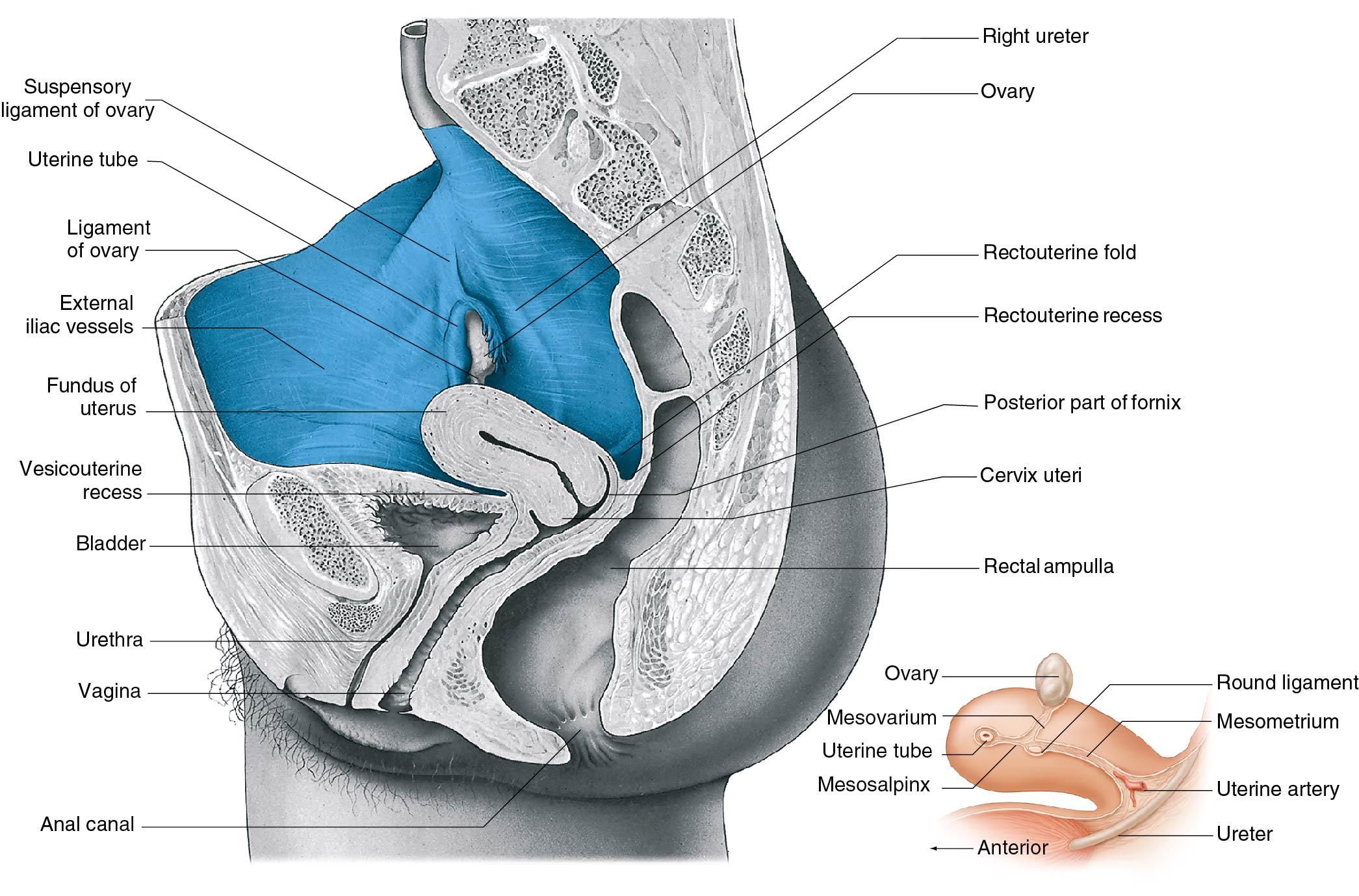
The axis of the upper portion of the vagina lies fairly close to the horizontal plane when a woman is standing, with the upper portion of the vagina curving toward the hollow of the sacrum. In most women an angle of at least 90 degrees is formed between the axis of the vagina and the axis of the uterus ( Fig. 3.7 ). The vagina is held in position by the surrounding endopelvic fascia and ligaments.
The lower third of the vagina is in close relationship with the urogenital and pelvic diaphragms. The middle third of the vagina is suspended by the lower portion of the cardinal ligaments and supported by the levator ani muscles. The upper third is suspended by the upper portions of the cardinal ligaments and the parametria. The vagina of reproductive-age women has numerous transverse folds, vaginal rugae. They help provide accordion-like distensibility and are more prominent in the lower third of the vagina. The cervix extends into the upper part of the vagina. The spaces between the cervix and attachment of the vagina are called fornices. The posterior fornix is considerably larger than the anterior fornix; thus the anterior vaginal length is approximately 6 to 9 cm compared with a posterior vaginal length of 8 to 12 cm. Vaginal length is increased slightly by a woman’s weight and height. Age, conversely, leads to a shortening of the vagina. A study by Tan and colleagues noted a decrease of 0.08 cm per 10 years ( ). The lack of estrogen during menopause also leads to loss of vaginal elasticity.
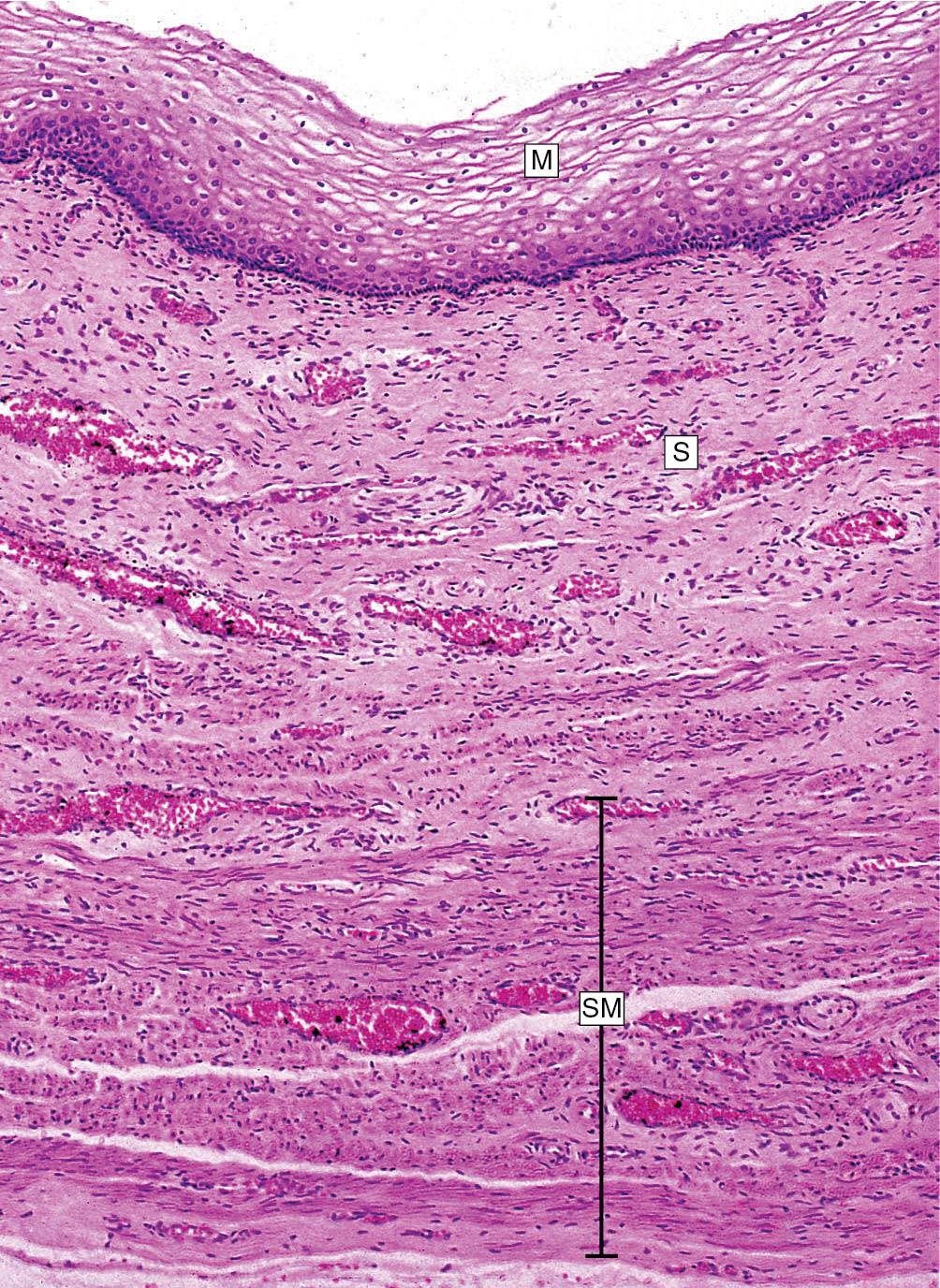
Histologically the vagina is composed of four distinct layers. The mucosa consists of a stratified, nonkeratinized squamous epithelium ( Fig. 3.8 ). If the environment of the vaginal mucosa is modified, as in uterine prolapse, then the epithelium may become keratinized. The squamous epithelium is similar microscopically to the exocervix, although the vagina has larger and more frequent papillae that extend into the connective tissue. The normal vagina does not have glands. The next layer is the lamina propria, or tunica. It is composed of fibrous connective tissue. Throughout this layer of collagen and elastic tissue is a rich supply of vascular and lymphatic channels. The density of the connective tissue in the endopelvic fascia varies throughout the longitudinal axis of the vagina. The muscular layer has many interlacing fibers; however, an inner circular layer and an outer longitudinal layer can be identified. The fourth layer consists of cellular areolar connective tissue containing a large plexus of blood vessels.
The vascular system of the vagina is generously supplied with an extensive anastomotic network throughout its length. The vaginal artery originates either directly from the uterine artery or as a branch of the internal iliac artery arising posterior to the origin of the uterine and inferior vesical arteries. Multiple vaginal arteries may be present on each side of the pelvis. There is an anastomosis with the cervical branch of the uterine artery to form the azygos arteries. Branches of the internal pudendal, inferior vesical, and middle hemorrhoidal arteries also contribute to the interconnecting network and the longitudinal azygos arteries.
The venous drainage is complex and accompanies the arterial system. Below the pelvic floor, the principal venous drainage occurs via the pudendal veins. The vaginal, uterine, and vesical veins, as well as those around the rectosigmoid, all provide venous drainage of the venous plexuses surrounding the middle and upper vagina.
The nerve supply of the vagina comes from the autonomic nervous system’s vaginal plexus, and sensory fibers come from the pudendal nerve. Pain fibers enter the spinal cord in sacral segments two to four. There is a paucity of free nerve endings in the upper two-thirds of the vagina.
The lymphatic drainage is characterized by its wide distribution and frequent crossovers between the right and left sides of the pelvis. In general the primary lymphatic drainage of the upper third of the vagina is to the external iliac nodes; the middle third of the vagina drains to the common and internal iliac nodes; and the lower third has a complex and variable distribution, including the common iliac, superficial inguinal, and perirectal nodes.
In clinical practice, anatomic descriptions of pelvic organs are derived from Latin roots, such as the word vagina, which is derived from the Latin word for “sheath.” In contrast, the names for surgical procedures of pelvic organs are derived from Greek roots. For instance, colpectomy, colporrhaphy, and colposcopy are derived from kolpos (“fold”), the Greek word for the vagina ; another example is hysterectomy (Greek) versus uterus (Latin).
Clinicians should consider the H shape of the vagina when they insert a speculum and inspect the walls of the vagina. The posterior fornix is an important surgical landmark because it provides direct access to the cul-de-sac of Douglas. The distal course of the ureter is an essential consideration in vaginal surgery. Ureteral injury can result from vaginally placed sutures used to obtain hemostasis in patients with vaginal lacerations. The anatomic proximity and interrelationships of the vascular and lymphatic networks of the bladder and vagina are such that inflammation of one organ can produce symptoms in the other. For example, vaginitis sometimes produces urinary tract symptoms such as frequency and dysuria.
A Gartner duct cyst is a congenital abnormality caused by incomplete regression of the wolffian (mesonephric) duct ( Fig. 3.9 A). It is usually present on the lateral wall of the vagina. However, if encountered in the lower third of the vagina, these cysts are located anteriorly and may be difficult to distinguish from a large urethral diverticulum. Often these cysts remain small and require no treatment, but they may be excised surgically if they produce symptoms or interfere with sexual function. Before excision, magnetic resonance imaging (MRI) is often obtained to confirm the diagnosis ( Fig. 3.9 B).
An interesting phenomenon is the source of vaginal lubrication during intercourse. For years there was speculation on how an organ without glands is able to “secrete” fluid. Vaginal lubrication occurs from a transudate produced by engorgement of the vascular plexuses that encircle the vagina. This richness of vascularization allows many drugs to readily enter the systemic circulation when placed in the vagina. Medications that are absorbed vaginally go directly into the systemic circulation, bypassing the liver and its metabolism on the first round through the circulation.
The anatomic relationship between the long axis of the vagina and other pelvic organs may be altered by pelvic relaxation resulting primarily from the trauma of childbirth. Atrophy or weakness of the endopelvic fascia and muscles surrounding the vagina may result in the development of a cystocele, rectocele, or enterocele, all possibly contributing to a vaginal vault prolapse. One of many popular operations for vaginal vault prolapse is fixation of the vaginal apex to the sacrospinous ligament. A rare complication of this operation is massive hemorrhage, usually from the arterial or venous branches of the inferior gluteal or pudendal vasculature.
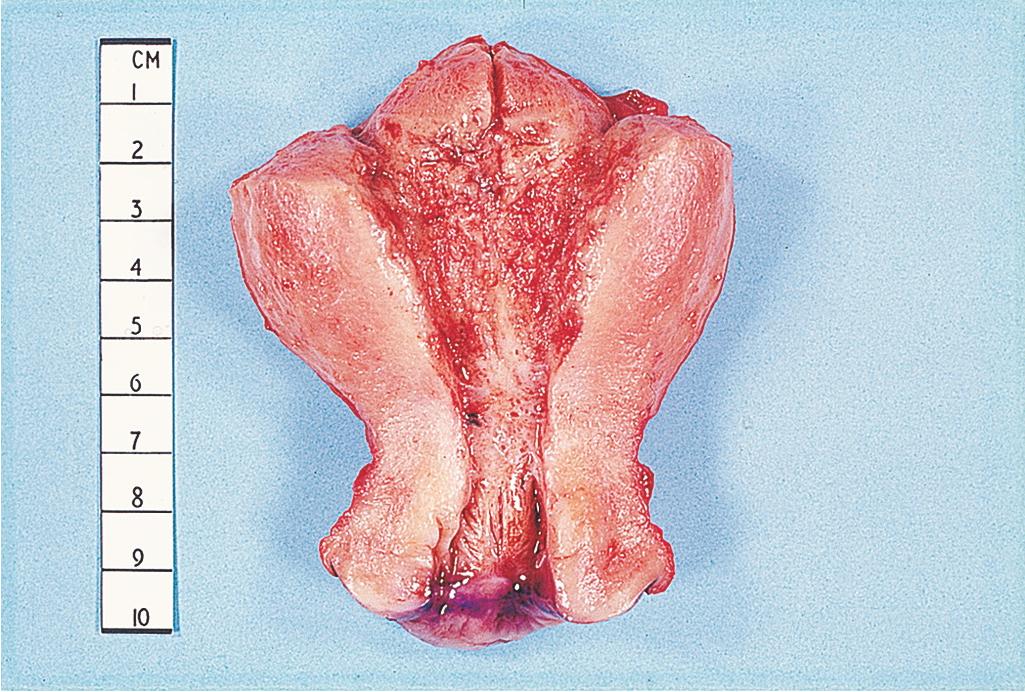
The lower, narrow portion of the uterus is the cervix. The word cervix originates from the Latin word for neck. The Greek word for neck is trachelos, and when the cervix is removed, the surgical procedure is termed a trachelectomy. The cervix may vary in shape from cylindric to conical. It consists of predominantly fibrous tissue, in contrast to the primarily muscular corpus of the uterus.
The vagina is attached obliquely around the middle of the cervix; this attachment divides the cervix into an upper, supravaginal portion and a lower segment in the vagina called the portio vaginalis ( Fig. 3.10 ). The supravaginal segment is covered by peritoneum posteriorly and is surrounded by loose, fatty connective tissue— the parametrium —anteriorly and laterally.
The canal of the cervix is fusiform, with the widest diameter in the middle. The length and width of the endocervical canal varies; it is usually 2.5 to 3 cm long and 7 to 8 mm at its widest point. The width of the canal varies with the parity of the woman and with changing hormonal levels. The cervical length increases in pregnancy, reaching maximal length in the second trimester. The cervical canal opens into the vagina at the external os of the cervix. In the majority of women the external os is in contact with the posterior vaginal wall. The external os is small and round in nulliparous women but is wider and gaping after vaginal delivery. Often, lateral or stellate scars, which are residual marks of previous cervical lacerations, are present.
The mucous lining of the endocervical canal of nulliparous women is arranged in longitudinal folds, called plicae palmatae, with secondary branching folds called the arbor vitae. These folds, which form a herringbone pattern, often disappear after vaginal delivery.
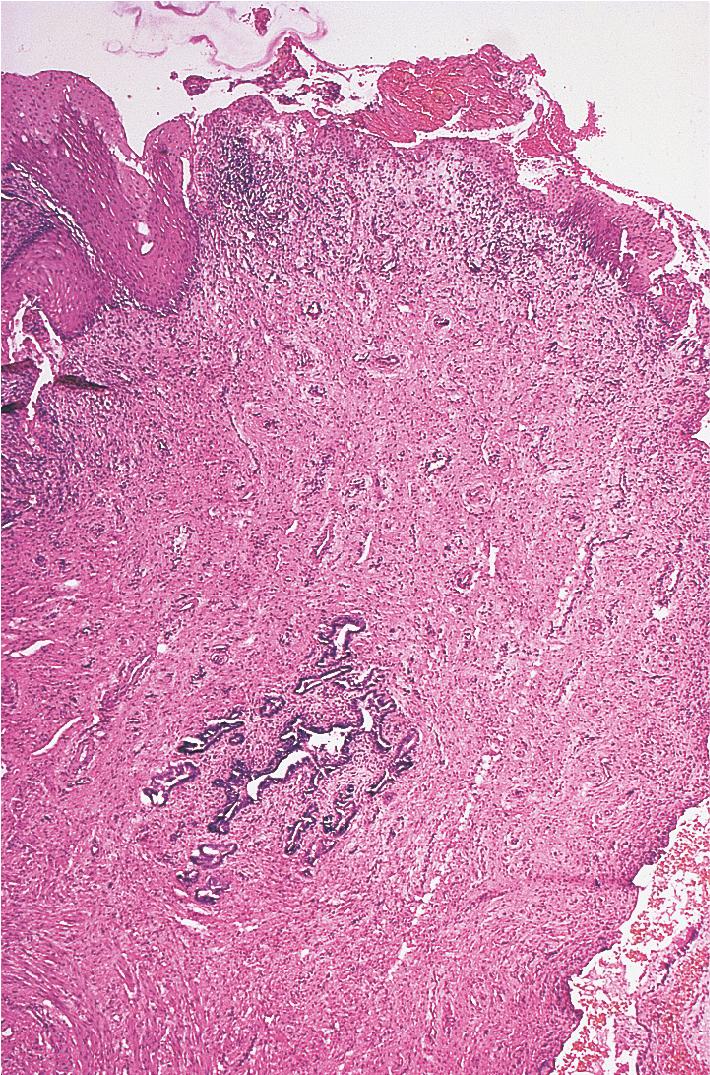
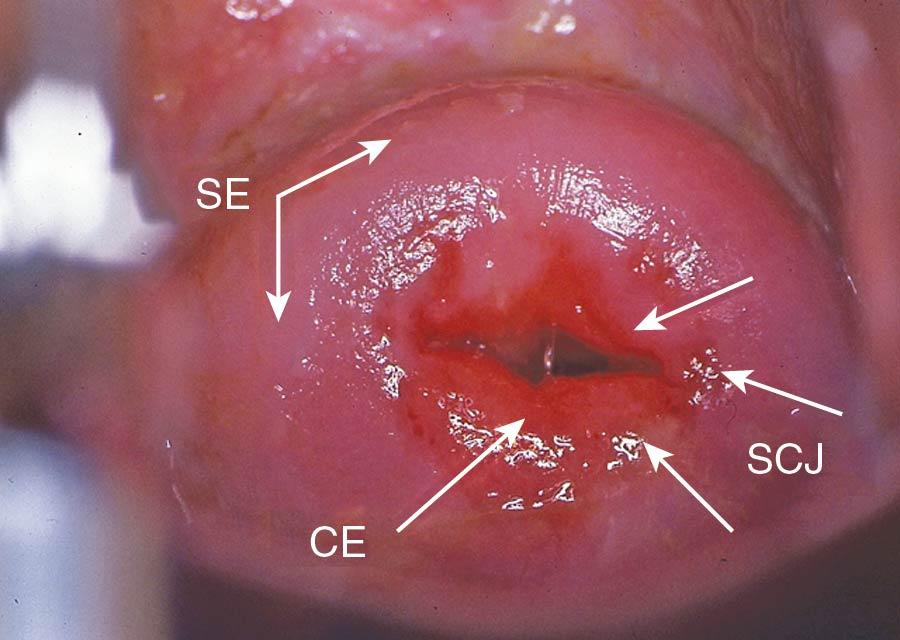
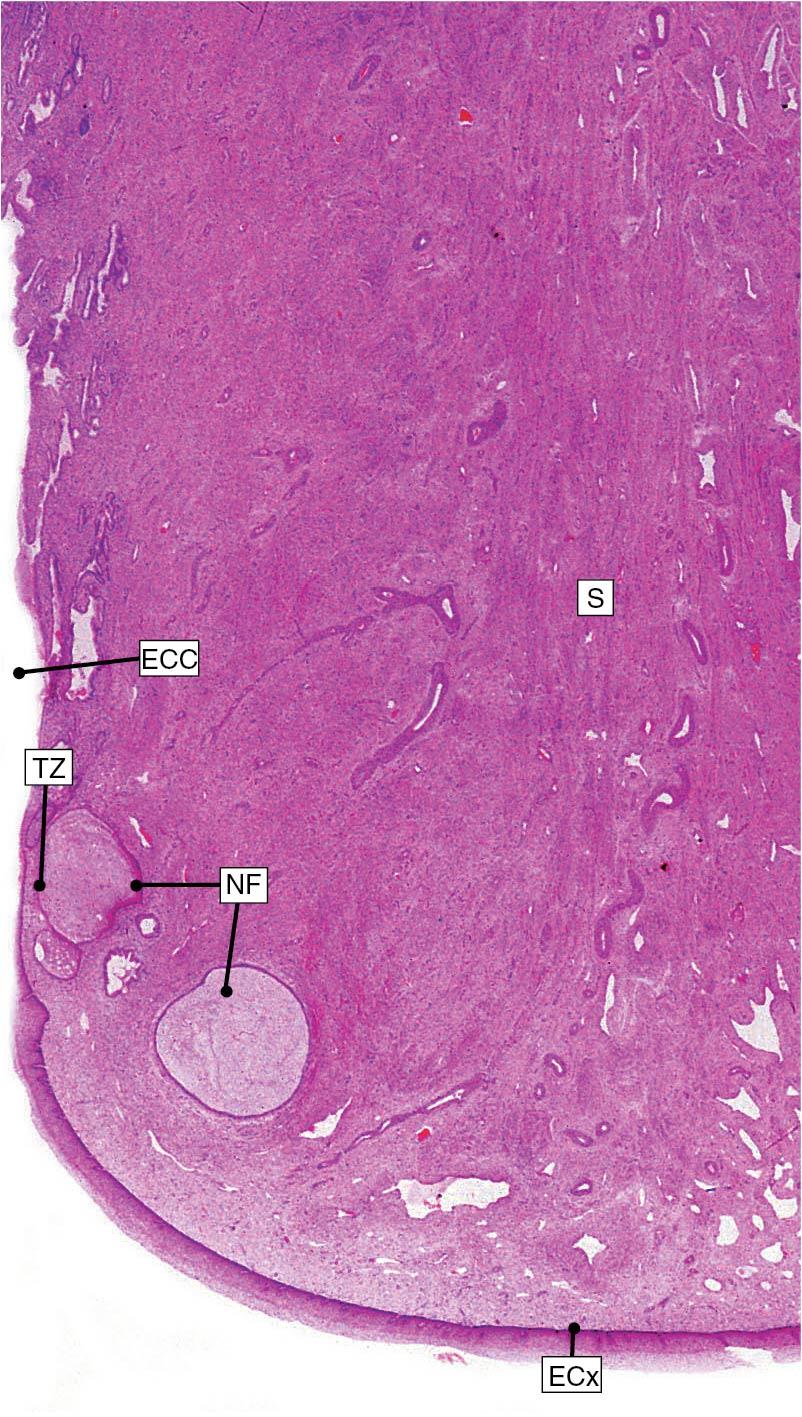
A single layer of columnar epithelium lines the endocervical canal and the underlying glandular structures. This specialized epithelium secretes mucus, which facilitates sperm transport. An abrupt transformation usually is seen at the junction of the columnar epithelium of the endocervix and the nonkeratinized stratified squamous epithelium of the portio vaginalis ( Figs. 3.11 and 3.12 ). The stratified squamous epithelium of the exocervix is identical to the lining of the vagina.

The dense, fibromuscular cervical stroma is composed primarily of collagenous connective tissue and mucopolysaccharide ground substance. The collagen framework and ground substance are sensitive to hormonal effects. The connective tissue contains approximately 15% smooth muscle cells and a small amount of elastic tissue ( Fig. 3.13 ). However, there are few muscle fibers in the distal portions of the cervix.
It is not surprising that the cervical and uterine vascular supplies are interrelated. The arterial supply of the cervix arises from the descending branch of the uterine artery. The cervical arteries run on the lateral side of the cervix and form the coronary artery, which encircles the cervix. The azygos arteries run longitudinally in the middle of the anterior and posterior aspects of the cervix and the vagina. There are numerous anastomoses between these vessels and the vaginal and middle hemorrhoidal arteries. The venous drainage accompanies these arteries. The lymphatic drainage of the cervix is complex, involving multiple chains of nodes. The principal regional lymph nodes are the obturator, common iliac, internal iliac, external iliac, and visceral nodes of the parametria. Other possible lymphatic drainage includes the following chains of nodes: superior and inferior gluteal, sacral, rectal, lumbar, aortic, and visceral nodes over the posterior surface of the urinary bladder. The stroma of the endocervix is rich in free nerve endings . Pain fibers accompany the parasympathetic fibers to the second, third, and fourth sacral segments.
The major arterial supply to the cervix is located on the lateral cervical walls at the 3 and 9 o’clock positions, respectively. Therefore a deep figure-of-eight suture through the vaginal mucosa and cervical stroma at 3 and 9 o’clock helps to reduce blood loss during procedures such as cone biopsy. If the gynecologist is overzealous in placing such a hemostatic suture high in the vaginal fornix, it is possible to compromise the course of the distal ureter just before it enters the bladder.
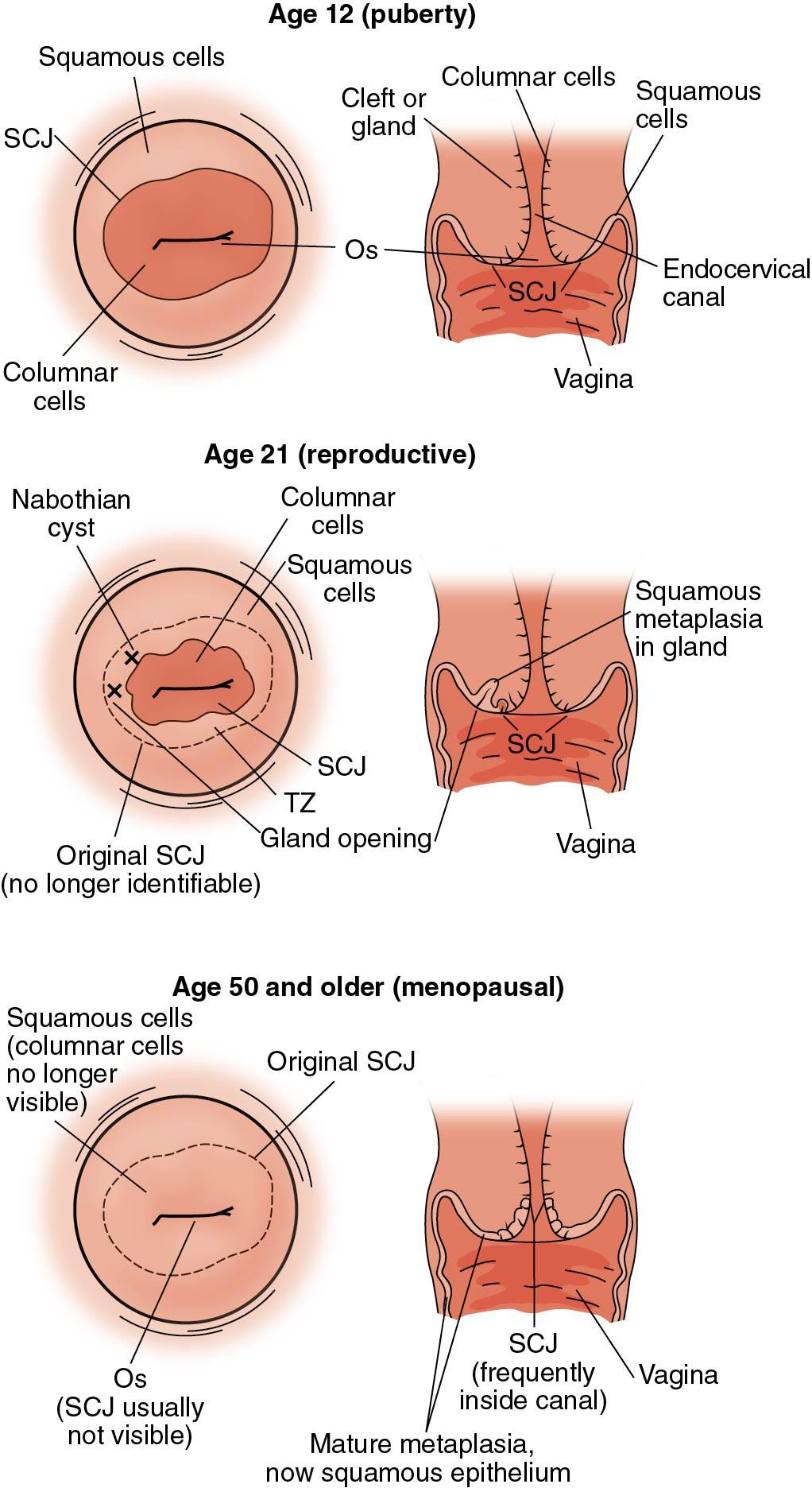
The transformation zone, also known as the squamocolumnar junction (SCJ), of the cervix is an important anatomic landmark for clinicians. This area encompasses the transition from stratified squamous epithelium to columnar epithelium. Most cases of cervical dysplasia develop within this transformation zone and are due to human papillomavirus (HPV) infections.
The position of a woman’s transformation zone, in relation to the long axis of the cervix, depends on her age and hormonal status. When the woman is young, the transformation zone is located further out on the cervical portio. This is called an ectropion and is a normal finding, especially during pregnancy. As a woman ages, the transformation zone migrates higher up the endocervical canal ( Fig. 3.14 ).
The endocervix is rich in free nerve endings. Occasionally, women experience a vasovagal response during transcervical instrumentation of the uterine cavity. Serial cardiac monitoring during insertion of intrauterine devices demonstrates a reflex bradycardia in some women. The sensory innervation of the exocervix is not as concentrated or sophisticated as that of the endocervix or external skin. Therefore usually the exocervix may be cauterized by either cold or heat without major discomfort to the patient.
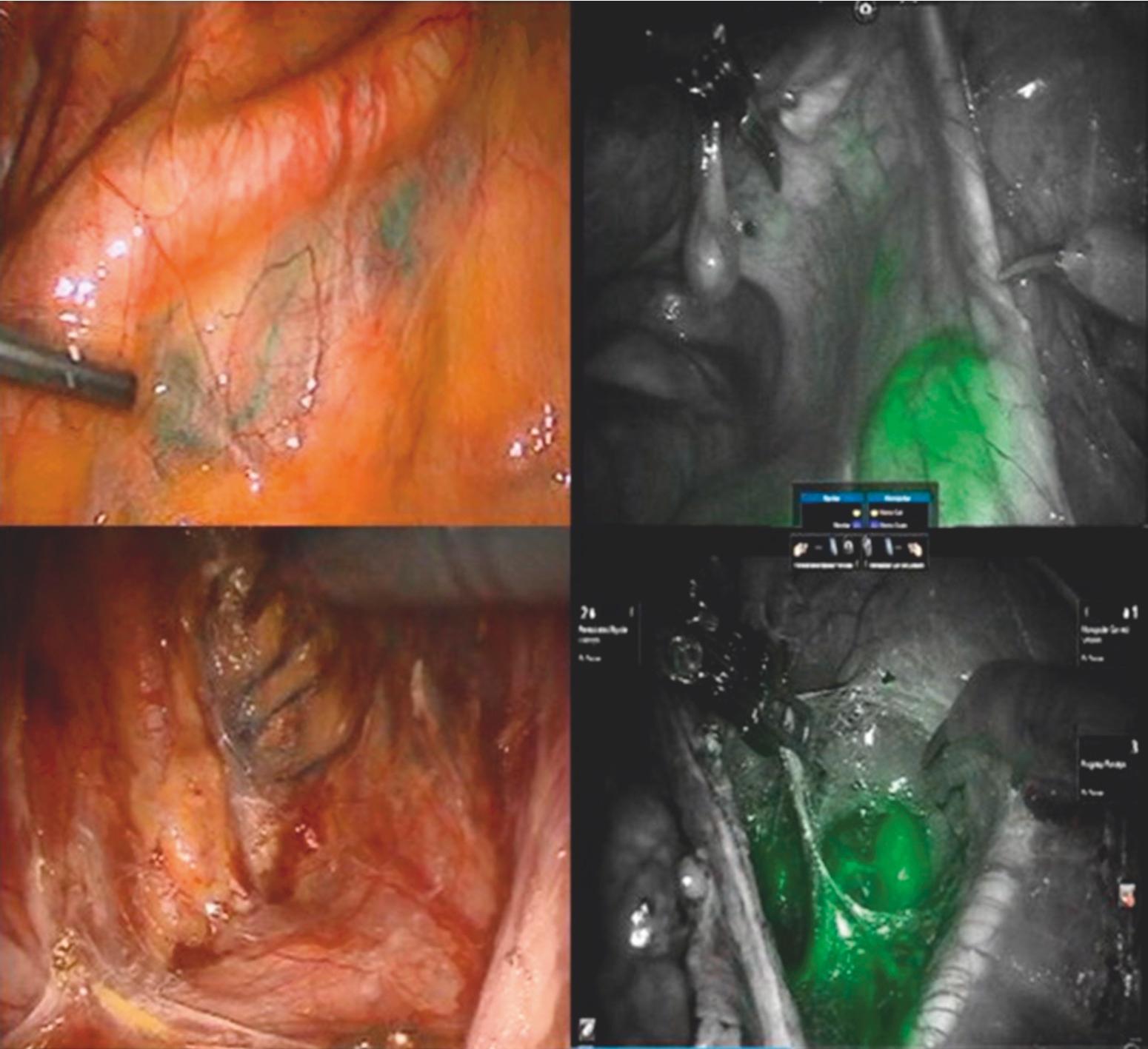
The lymphatic drainage of the cervix is fairly organized, as described earlier. Similar to other disease sites, sentinel lymph node (SLN) mapping and biopsy for cervical cancer are replacing the more traditional full lymphadenectomies in favor of fewer complications, specifically lymphedema. Sentinel lymph node mapping in cervical cancer was first described in 1999 by Echt and coworkers when they injected 13 patients who had early-stage cervical cancer with a blue dye, lymphazurin, and identified SLNs in 15% ( ). This technique has been refined over the years and is now performed using near-infrared fluorescence imaging and indocyanine green (ICG) and achieves detection of SLNs in 85% to 90% of cases.
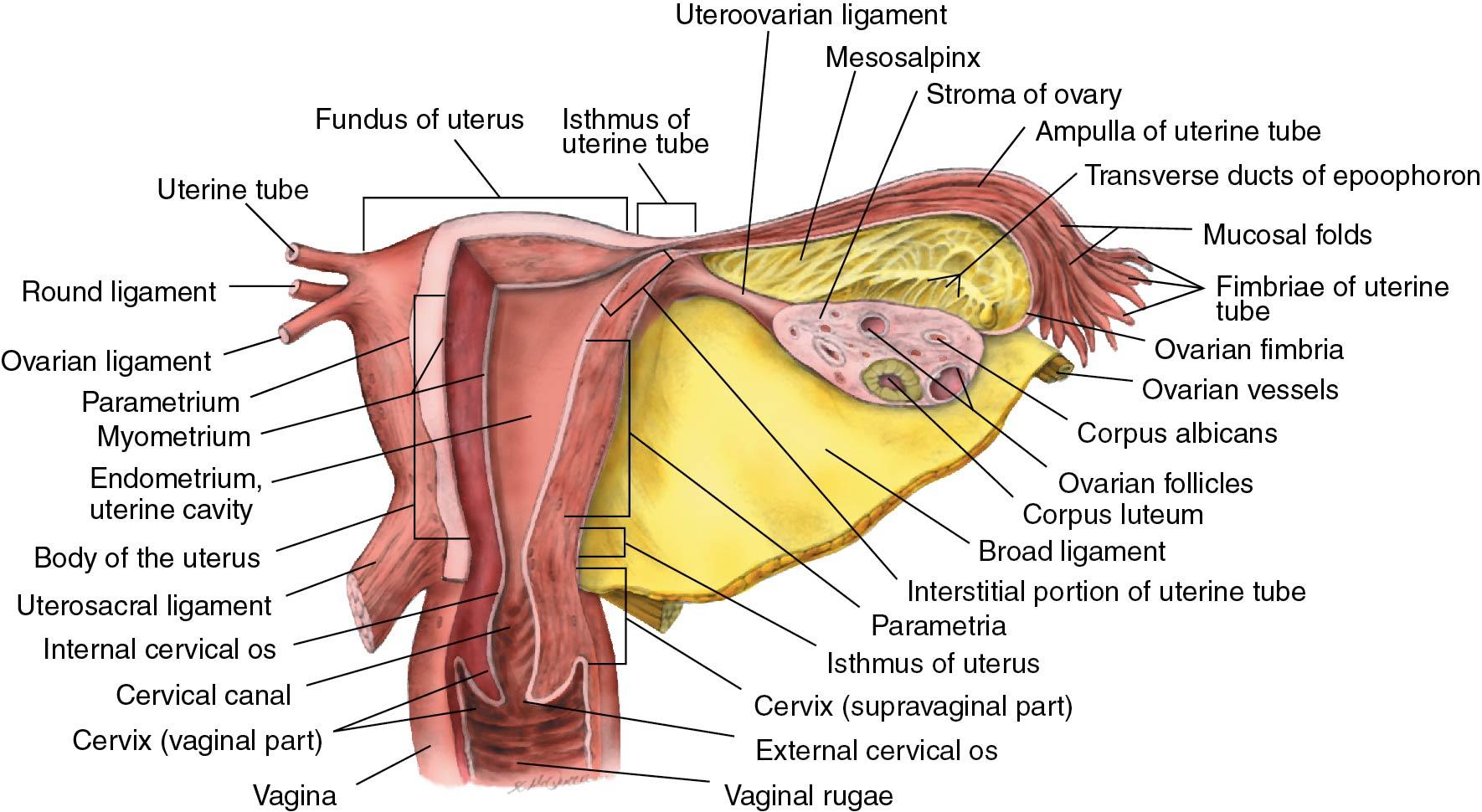
The uterus is a thick-walled, hollow, muscular organ located centrally in the female pelvis. Adjacent to the uterus are the urinary bladder anteriorly, the rectum posteriorly, and the broad ligaments laterally (see Fig. 3.7 ). The uterus is globular and slightly flattened anteriorly; it has the general configuration of an inverted pear. The short area of constriction in the lower uterine segment is termed the isthmus ( Fig. 3.15 ). The dome-shaped top of the uterus is termed the fundus. The lower edge of the fundus is described by an imaginary line drawn between the site of entrance of each oviduct. The size and weight of the normal uterus depend on previous pregnancies and the hormonal status of the individual. The uterus of a nulliparous woman is approximately 8 cm long, 5 cm wide, and 2.5 cm thick and weighs 40 to 50 g. In contrast, in a multiparous woman the uterus on average is 9 to 10 cm long, 6 to 7 cm wide, and 4 cm thick and normally weighs approximately 80 to 110 g. The capacity of the uterus to enlarge during pregnancy results in a 10- to 20-fold increase in weight at term. This growth is accompanied by an increase of blood flow to approximately 10% of cardiac output at term. After menopause the uterus atrophies and the measurements vary depending on years since menopause.
The cavity of the uterus is flattened and triangular. The oviducts enter the uterine cavity at the superolateral aspects of the cavity in the areas designated the cornua. In the majority of women, the long axis of the uterus is both anteverted in respect to the long axis of the vagina and anteflexed in relation to the long axis of the cervix. However, a retroflexed uterus is a normal variant found in approximately 25% of women ( Fig. 3.16 ).
The uterus has three layers, similar to other hollow abdominal and pelvic organs. The thin, external serosal layer makes up the visceral peritoneum. The peritoneum is firmly attached to the uterus in all areas except anteriorly at the level of the internal os of the cervix, where it is only loosely attached. The wide middle muscular layer is composed of three indistinct layers of smooth muscle. The outer longitudinal layer is contiguous with the muscle layers of the oviduct and vagina. The middle layer has interlacing oblique, spiral bundles of smooth muscle and large venous plexuses. The inner muscular layer is also longitudinal. The endometrium is a reddish mucous membrane that varies from 1 to 6 mm in thickness, depending on hormonal stimulation ( Fig. 3.17 ).
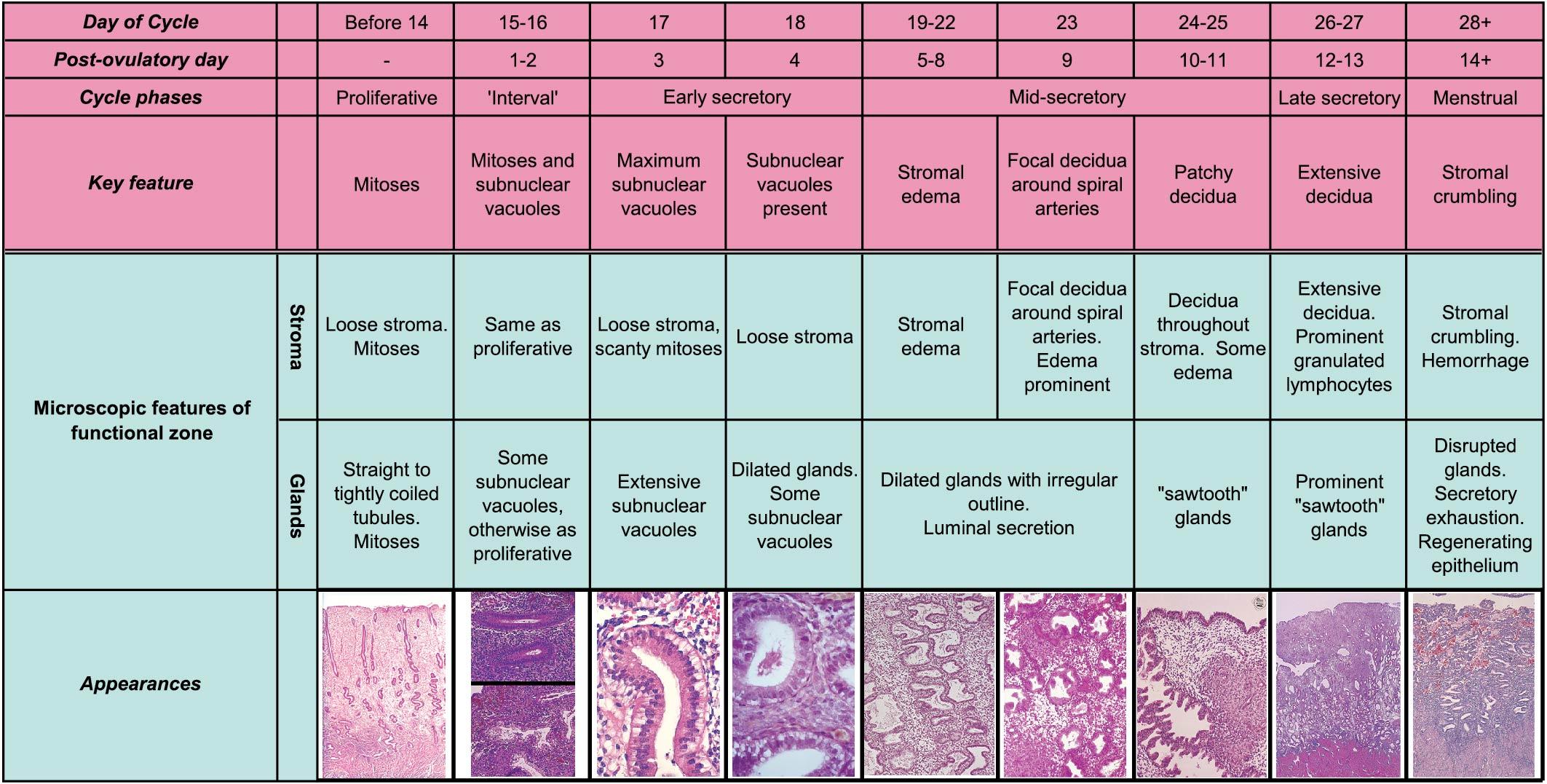
The uterine glands are tubular and composed of tall columnar epithelium. The cells of the endometrial stroma resemble embryonic connective tissue with scant cytoplasm and large nuclei. The endometrium may be divided into an inner stratum basale and an outer stratum functionale. The stratum functionale may be further subdivided into an inner compact stratum and a more superficial spongy stratum. Only the stratum functionale responds to fluctuating hormonal levels.
The uterine and ovarian arteries provide the arterial blood supply of the uterus. The uterine arteries are large branches of the hypogastric arteries, whereas the ovarian arteries originate directly from the aorta. The veins of the pelvic organs accompany the arteries. Therefore venous drainage from the fundus goes to the ovarian veins and blood from the corpus exits via the uterine veins into the iliac veins. The lymphatic drainage of the uterus is complex. The lymphatics from the fundus and the body of the uterus go to the aortic, lumbar, or pelvic nodes surrounding the iliac vessels, especially the internal iliac nodes. However, it is possible for metastatic disease from the uterus to be transported to the superior inguinal nodes via lymphatics in the round ligament or directly spread to the paraaortic nodes. Surprisingly, the lymphatic drainage of the uterus is not that different from the lymphatic drainage of the cervix.
In contrast to other pelvic organs, the afferent sensory nerve fibers from the uterus are in close proximity to the sympathetic nerves. Afferent nerve fibers from the uterus enter the spinal cord at the eleventh and twelfth thoracic segments. The sympathetic nerve supply to the uterus comes from the hypogastric and ovarian plexuses. The parasympathetic fibers are largely derived from the pelvic nerve and from the second, third, and fourth sacral segments.
Removal of the uterus is termed a hysterectomy, which is derived from the Greek word hystera, meaning “womb . ” The symptoms of primary dysmenorrhea are successfully treated in most women with the use of prostaglandin synthetase inhibitors such as nonsteroidal anti-inflammatory drugs (NSAIDs). However, it is possible to alleviate uterine pain by cutting the sensory nerves that accompany the sympathetic nerves. This operation is termed a presacral neurectomy. During the operation the gynecologist must be careful to avoid injuring the ureters and also careful to control hemorrhage from vessels in the retroperitoneal space. This operation has lost popularity because of its association with autonomic dysfunction of the bladder and rectum presumed to be secondary to the inadvertent disruption of motor fibers.
The position of the fundus of the uterus in relation to the long axis of the vagina is quite variable ( Fig. 3.16 ; see Fig. 3.7 ). Not only are there differences among individual women, but also in the same woman differences occur secondary to normal activity. In some women the uterus is anteflexed or anteverted, whereas in others the normal position is retroflexed or retroverted.
The arterial blood supply enters the uterus on its lateral margins. This relationship allows morcellation of an enlarged uterus to facilitate removal of multiple myomas without appreciably increasing blood loss during vaginal hysterectomy.
Similar to the lymphatic drainage of the cervix, the lymphatic drainage of the uterus has also been studied. Sentinel lymph nodes can be found on either side of the pelvis and paraaortic areas in 85% to 90% of cases using near-infrared fluorescence imaging and ICG ( ) ( Fig. 3.18 ).
The paired uterine tubes, more commonly referred to as the fallopian tubes or oviducts, extend outward from the superolateral portion of the uterus and end by curling around the ovary. The oviducts are also referred to using the prefix salpingo-, from the Greek salpinx, meaning “tube.” The tubes are contained in a free edge of the superior portion of the broad ligament. The mesentery of the tubes, the mesosalpinx, contains the blood supply and nerves. The uterine tubes connect the cornua of the uterine cavity and the peritoneal cavity. The ostia into the endometrial cavity are 1.5 mm in diameter, whereas the ostia into the abdominal cavity are approximately 3 mm in diameter.
The oviducts are between 10 and 14 cm long and slightly less than 1 cm in external diameter. Each tube is divided into four anatomic sections. The uterine intramural, or interstitial, segment is 1 to 2 cm long and is surrounded by myometrium. The isthmic segment begins as the tube exits the uterus and is approximately 4 cm long, narrow, 1 to 2 mm in inside diameter, and straight; it has the most highly developed musculature. The ampullary segment is 4 to 6 cm long, approximately 6 mm in inside diameter, and is wider and more tortuous in its course than other segments. Fertilization normally occurs in the ampullary portion of the tube. The infundibulum is the distal trumpet-shaped portion of the oviduct. Approximately 20 to 25 irregular finger-like projections, termed fimbriae, surround the abdominal ostia of the tube. One of the largest fimbriae is attached to the ovary, the fimbria ovarica.
The tube contains numerous longitudinal folds, called plicae, of mucosa and underlying stroma. Plicae are most prominent in the ampullary segment ( Fig. 3.19 ).
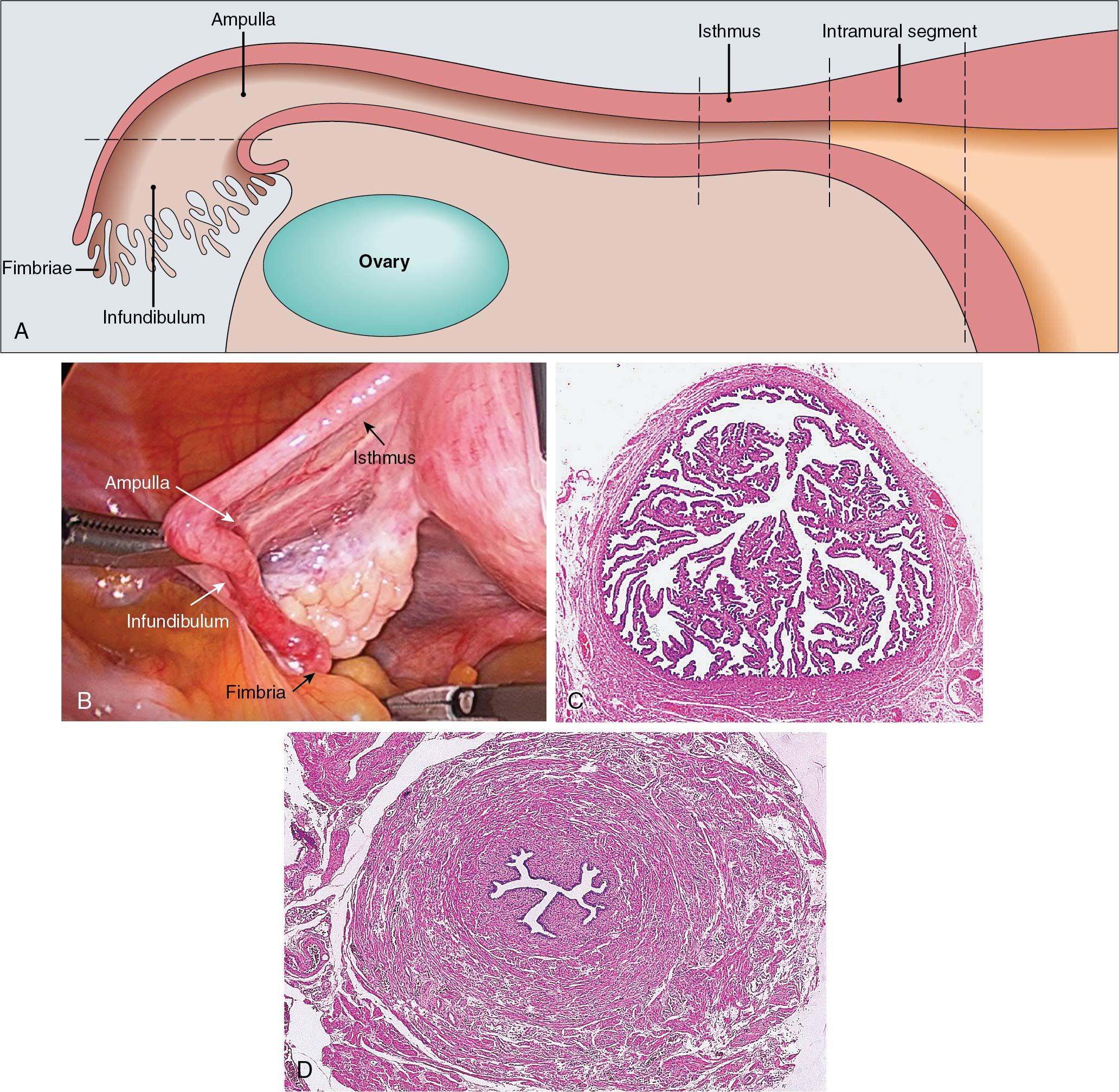
The mucosa of the oviduct has three different cell types. Columnar ciliated epithelial cells are most prominent near the ovarian end of the tube and make up 25% of the mucosal cells overall ( Fig. 3.20 ).
Secretory cells, also columnar in shape, comprise 60% of the epithelial lining and are more prominent in the isthmic segment. Narrow peg cells are found between secretory and ciliated cells and are believed to be a morphologic variant of secretory cells. The stroma of the mucosa is sparse. However, there is a thick lamina propria with vascular channels between the epithelium and muscular layers. The smooth muscle of the tube is arranged into inner circular and outer longitudinal layers. Between the peritoneal surface of the tube and the muscular layer is an adventitial layer that contains blood vessels and nerves.
The arterial blood supply to the oviducts is derived from terminal branches of the uterine and ovarian arteries. The arteries anastomose in the mesosalpinx. Blood from the uterine artery supplies the medial two-thirds of each tube. The venous drainage runs parallel to the arterial supply. The lymphatic system is separate and distinct from the lymphatic drainage of the uterus. Lymphatic drainage includes the internal iliac nodes and the aortic nodes surrounding the aorta and the inferior vena cava at the level of the renal vessels. The tubes are innervated by both sympathetic and parasympathetic nerves from the uterine and ovarian plexuses. Sensory nerves are related to spinal cord segments T11, T12, and L1.
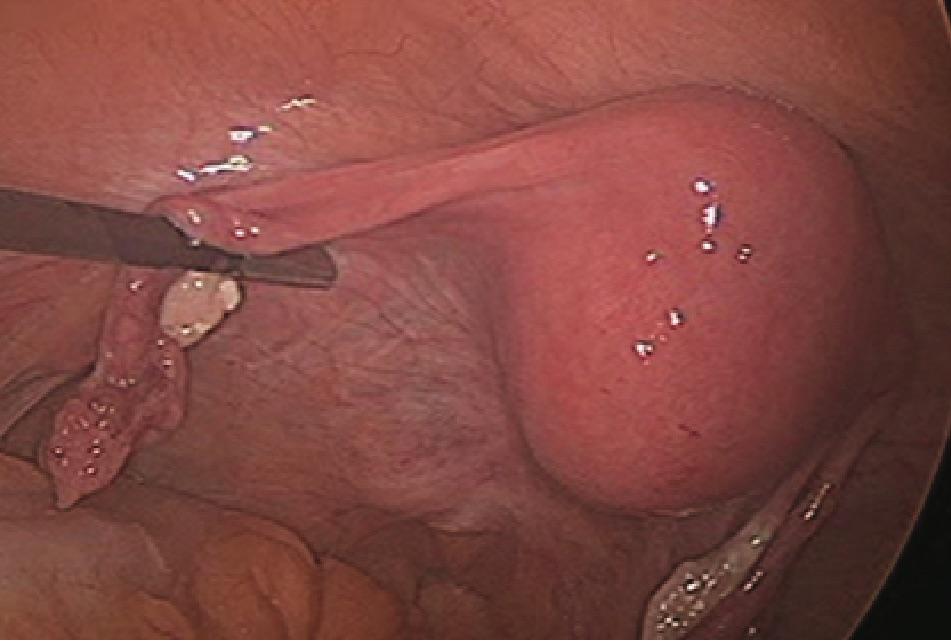
An ectopic pregnancy occurs when a fertilized ovum is implanted and develops outside the normal uterine cavity. The majority of ectopic pregnancies occur in the fallopian tube, with 70% found within the ampulla and 12% found in the isthmus of the fallopian tube. Quick evaluation and assessment are critical to this diagnosis and are often done in an emergency department setting. The most catastrophic bleeding associated with ectopic pregnancy occurs when the implantation site is in the intramural segment of the tube; many of these patients present with unstable vital signs and need to be taken the operating room emergently. The isthmic segment of the oviduct is the preferred site to apply an occlusive device, such a clip, or cauterization for female sterilization. The right oviduct and appendix are often adjacent. Clinically it may be difficult to differentiate inflammation of the tube from acute appendicitis. Accessory tubal ostia are discovered commonly and always connect with the lumen of the tube. These accessory ostia are usually found in the ampullary portion of the tube. The wide mesosalpinx of the ampullary segment of the tube allows torsion of the tube, which occasionally results in ischemic atrophy of the ampullary segment. Paratubal or paraovarian cysts can reach 5 to 10 cm in diameter and occasionally are confused with ovarian cysts before surgery.
The paired ovaries are light gray, and each one is approximately the size and configuration of a large almond. The surface of the ovary of adult women is pitted and indented from previous ovulations. The ovaries contain approximately 1 to 2 million oocytes at birth. During a woman’s reproductive lifetime, about 8000 follicles begin development. The growth of many follicles is blunted in various stages of development; however, approximately 300 ova eventually are released. The size and position of the ovary depend on the woman’s age and parity. During the reproductive years, ovaries weigh 3 to 6 g and measure approximately 1.5 cm by 2.5 cm by 4 cm. As a woman ages, the ovaries become smaller and firmer. The long axis of the ovary is vertical in a nulliparous woman who is standing, and the ovary rests in a depression of peritoneum named the ovarian fossa. Immediately adjacent to the ovarian fossa are the external iliac vessels, the ureter, and the obturator vessels and nerves.
Three prominent ligaments determine the anatomic mobility of the ovary ( Figs. 3.20 and 3.21 ).
The posterior portion of the broad ligament forms the mesovarium, which attaches to the anterior border of the ovary. The mesovarium contains the arterial anastomotic branches of the ovarian and uterine arteries, a plexus of veins, and the lateral end of the ovarian ligament. The ovarian ligament is a narrow, short, fibrous band that extends from the lower pole of the ovary to the uterus. The infundibulopelvic ligament, or suspensory ligament of the ovary, forms the superior and lateral aspect of the broad ligament. This ligament contains the ovarian artery, ovarian veins, and accompanying nerves and attaches the upper pole of the ovary to the lateral pelvic wall.
The ovary is subdivided histologically into an outer cortex and an inner medulla ( Fig. 3.22 ). The ovarian surface is covered by a single layer of cuboidal epithelium, termed the germinal epithelium. This term is a misnomer because the cells are similar to those of the coelomic mesothelium, which forms the peritoneum, and because the germinal epithelium is not related to the histogenesis of graafian follicles. If the ovary is transected, numerous transparent, fluid-filled cysts are noted throughout the cortex. Microscopically these are graafian follicles in various stages of development, active or regressing corpus luteum, and atretic follicles. The stroma of the cortex is composed primarily of closely packed cells around the follicles. These specialized connective tissue cells form the theca. The medulla contains the ovarian vascular supply and a loose stroma. The specialized polyhedral hilar cells are similar to the interstitial cells of the testis.
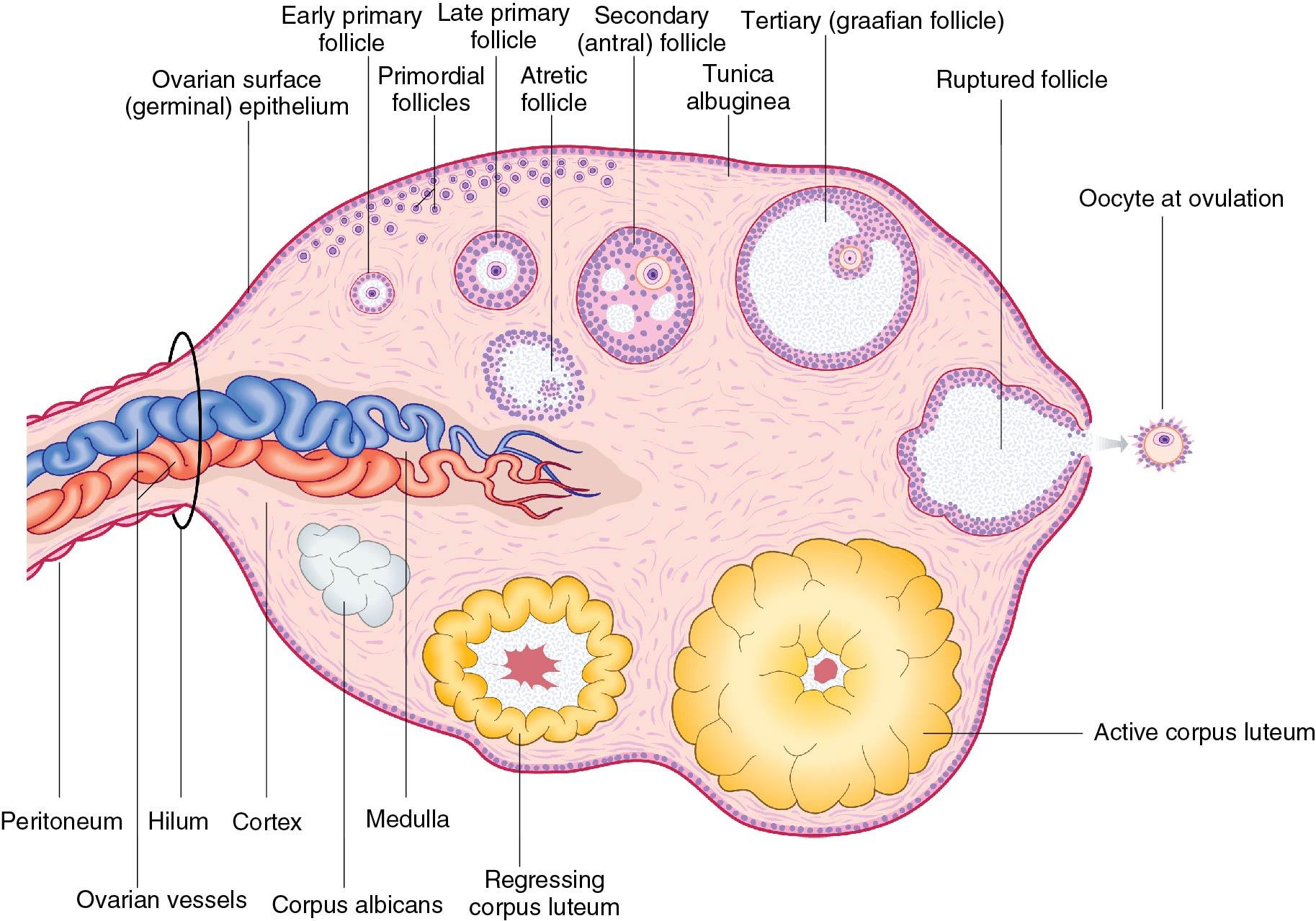
Each of the ovarian arteries arises directly from the aorta just below the renal arteries. They descend in the retroperitoneal space, cross anterior to the psoas muscles and internal iliac vessels, and enter the infundibulopelvic ligaments, reaching the mesovarium in the broad ligament. The ovarian blood supply enters through the hilum of the ovary. The venous drainage of the ovary collects in the pampiniform plexus and consolidates into several large veins as it leaves the hilum of the ovary. The ovarian veins accompany the ovarian arteries, with the left ovarian vein draining into the left renal vein, whereas the right ovarian vein connects directly with the inferior vena cava.
The lymphatic drainage of the ovaries is primarily to the aortic nodes adjacent to the great vessels at the level of the renal veins. Metastatic disease from the ovary occasionally takes a shorter course to the iliac nodes. The autonomic and sensory nerve fibers accompany the ovarian vasculature in the infundibulopelvic ligament. They connect with the ovarian, hypogastric, and aortic plexuses.
The size of the “normal” ovary during the reproductive years and the postmenopausal period is important in clinical practice. Before menopause a normal ovary may be up to 5 cm long. Thus a small physiologic cyst may cause an ovary to be 6 to 7 cm in diameter. In contrast, the normal atrophic postmenopausal ovary usually cannot be palpated during pelvic examination and is often not visible by ultrasound imaging.
It is important to emphasize that the ovaries and surrounding peritoneum are not devoid of pain and pressure receptors. Therefore it is not unusual for a woman to experience discomfort when normal ovaries are palpated bimanually during a routine pelvic examination. Patients can present in an acute setting or during a routine office visit with complaints of pelvic pain.
The close anatomic proximity of the ovary, ovarian fossa, and ureter is emphasized in surgery to treat severe endometriosis or pelvic inflammatory disease. It is important to identify the course of the ureter to facilitate removal of all of the ovarian capsule that is adherent to the peritoneum and surrounding structures so as to avoid immediate ureteral injury and residual retroperitoneal ovarian remnants in the future. Prophylactic oophorectomy is performed at the time of pelvic operations in many postmenopausal women older than 65. Sometimes bilateral oophorectomy is technically more difficult when associated with a vaginal procedure in contrast to an abdominal or laparoscopic hysterectomy. Vaginal removal of the ovaries may be facilitated by identifying the anatomic landmarks, similar to the abdominal approach, and separately clamping the round ligaments and infundibulopelvic ligaments.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here