Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The primary purpose of the esophagus is to transport food from the mouth to the stomach, and the esophagus has no digestive or absorptive function. The esophagus is a muscular tube that starts at the inferior border of the cricoid cartilage in the neck and traverses the chest, ending as it enters the stomach in the upper abdomen. Esophageal surgeons need to be familiar with the anatomy and clinical importance of the relationship of the esophagus to surrounding structures in all three areas of the body.
The esophagus is anchored superiorly to the cricoid cartilage and inferiorly to the diaphragm. Its length from the cricoid cartilage at C6 to the gastric orifice at T11 ranges from 22 to 28 cm ( Fig. 4.1 ). The length of the esophagus varies with the height of the patient. The esophageal bed lies in the posterior mediastinum along the ventral surface of the vertebra. This is the shortest distance for reconstruction after esophagectomy and measures approximately 30 cm. When the orthotopic route is not available due to previous surgery, the retrosternal (32 cm) or subcutaneous (34 cm) routes are alternatives.
On endoscopy, the upper esophageal sphincter is approximately 15 cm from the incisors, the carina at 25 cm, and the lower esophageal sphincter at 38 to 40 cm in men and 36 to 38 cm in women. When planning the surgical approach to the esophagus, it is useful to consider the location of the tumor relative to the carina at 25 cm in deciding whether to perform a left or a right thoracotomy to avoid the aortic arch, which blocks access to the upper thoracic esophagus on the left.
While the cervical esophagus is flattened by surrounding structures, the thoracic esophagus is more round due to negative intrathoracic pressure. Once the esophagus enters the abdomen, it becomes more flattened again as a result of positive intraabdominal pressure. The overall diameter of the esophagus is approximately 2.5 cm. There are three anatomic narrowings of the esophagus ( Fig. 4.2 ). The narrowest part of the gastrointestinal tract is at the cricopharyngeal constriction at the upper esophageal sphincter, where the esophagus is 1.5 cm in diameter. In the superior mediastinum, the aortic arch, left atrium, and left mainstem bronchus compress the left anterolateral aspect of the esophagus around 22 cm from the incisors. The third area of narrowing is at the lower esophageal sphincter. These areas are important since swallowed foreign bodies often lodge in these areas.
The esophageal wall is composed of four layers, including an inner squamous mucosal layer, submucosa, muscularis propria, and adventitia. The mucosal layer consists of the squamous epithelium, lamina propria, and muscularis mucosa, while the muscularis propria consists of an inner circular and outer longitudinal layer of muscle ( Fig. 4.3 ). The longitudinal layer originates from the cricoid cartilage as two muscle bundles that converge 3 cm distal to the cricopharyngeus muscle, leaving a V -shaped weakened area posteriorly covered only with circular muscle fibers, known as Laimer triangle ( Fig. 4.4 ). The cricopharyngeal muscle and up to 2 cm of the cervical esophagus are composed mostly of striated muscle. There is a gradual transition from striated muscle, which is only present in the upper 40% of the esophagus, to smooth muscle ( Fig. 4.5 ). As a result, most dysmotility disorders, which involve smooth muscle, predominantly affect the distal two-thirds of the esophagus.
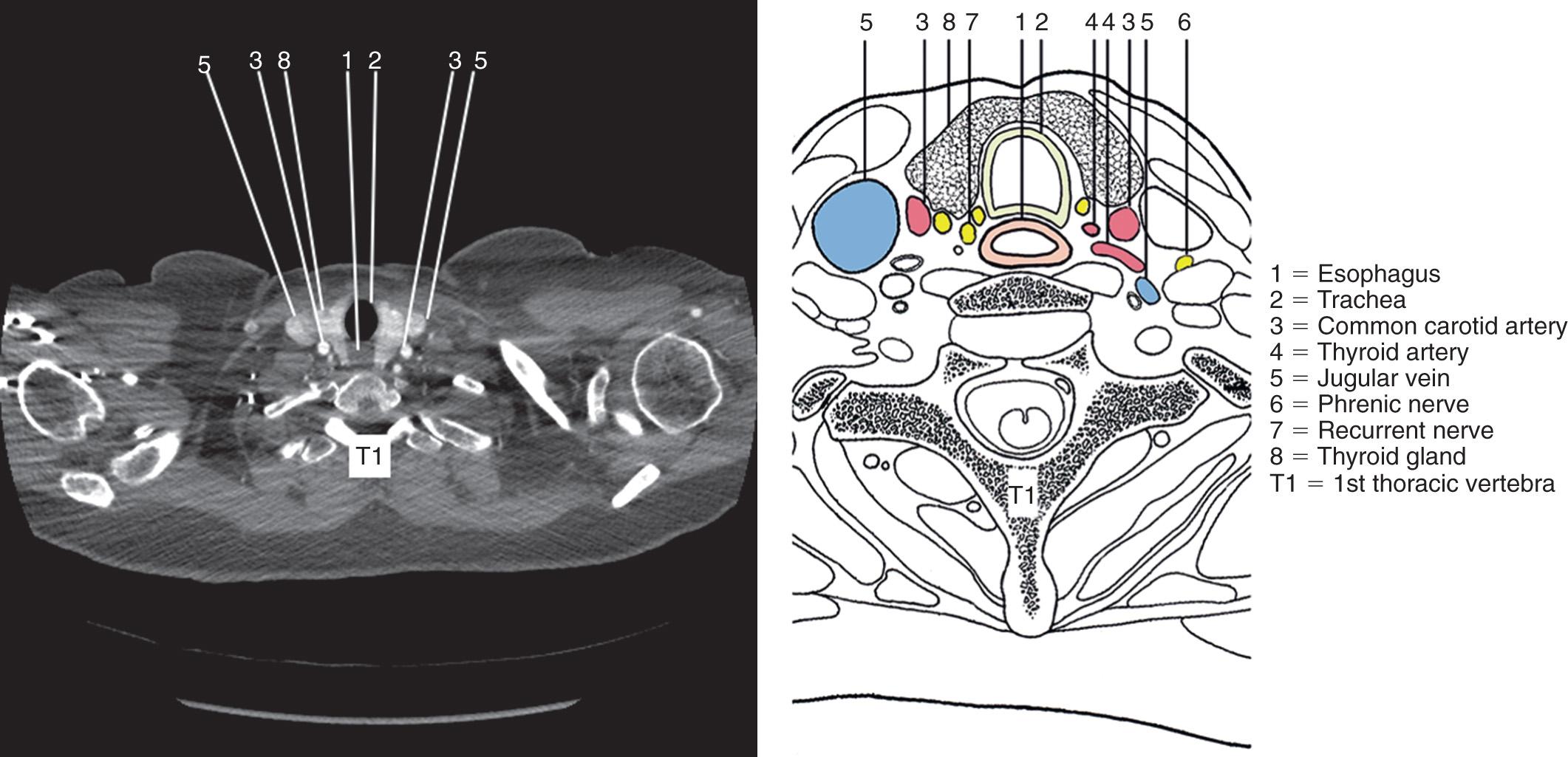
The cervical esophagus shifts to the left at the base of the neck, so the best approach to the cervical esophagus is a left neck incision (e.g., during the cervical anastomosis for a transhiatal esophagectomy or resection of a Zenker diverticulum). The cervical esophagus is 5 cm in length and extends from the cricoid cartilage at the C6 vertebra to the suprasternal notch anteriorly and the T1-T2 interspace posteriorly. The esophagus is surrounded by loose fibroareolar tissue, and unlike the remainder of the gastrointestinal tract, there is no serosal lining or mesentery.
The pretracheal fascia anteriorly, prevertebral fascia posteriorly, and carotid sheaths laterally create two cervical compartments, the paraesophageal space anteriorly, and the retroesophageal space posteriorly. The pretracheal fascia extends to the pericardium, while the prevertebral fascia extends to the diaphragm, connecting compartments in the neck and chest, allowing infections from tonsillar or dental abscesses to spread quickly into the mediastinum. A descending infection can rapidly lead to potentially fatal necrotizing mediastinitis, emphasizing the importance of early surgical drainage. Iatrogenic perforations most commonly occur above the narrowing of the cricopharyngeal muscle, resulting in a posterior pharyngeal perforation (see Fig. 4.4 ).
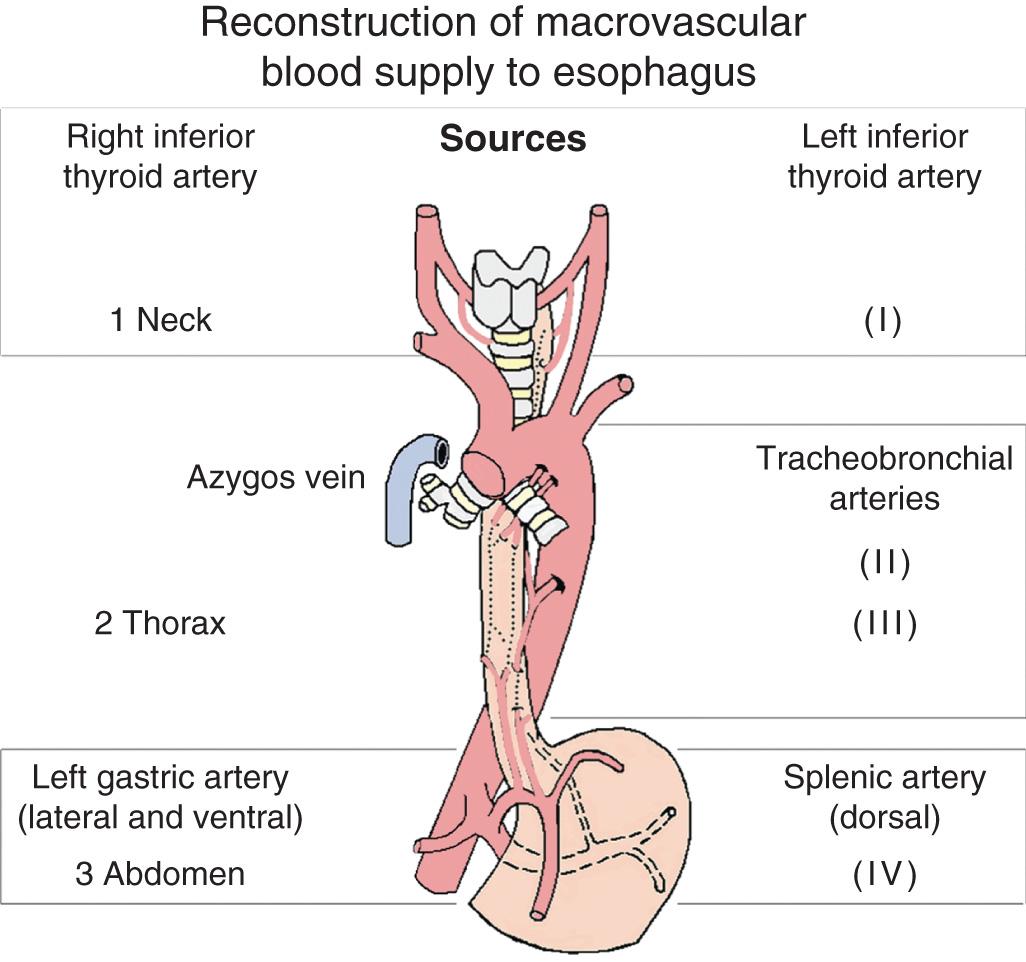
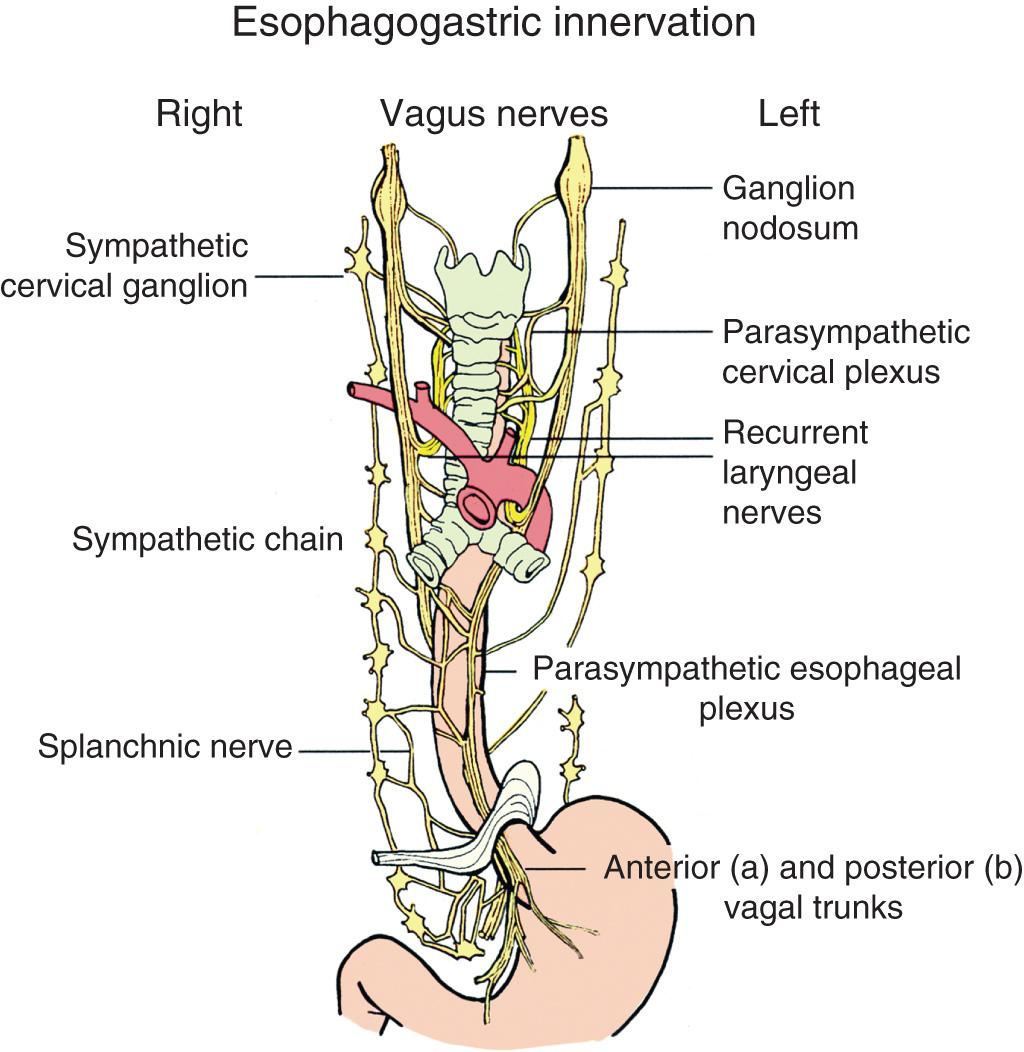
The arterial blood supply for the cervical esophagus originates from the right and left superior and inferior thyroid arteries ( Fig. 4.6 ). There are also smaller branches from the common carotid and subclavian arteries. Venous drainage is through the inferior thyroid vein. The middle thyroid vein crosses from the internal jugular vein to the thyroid gland, and often is divided to improve exposure of the cervical esophagus. Innervation of the cervical esophagus is from the recurrent laryngeal nerves and the sympathetic chains.
The posterior pharynx consists of three bilateral constrictor muscles originating from the base of the skull, the hyoid bone, and the thyroid and cricoid cartilages. These constrictor muscles converge in the midline posteriorly to form a median raphe. The cricopharyngeus forms a continuous band of muscle originating from the cricoid cartilage without a raphe and blends with the oblique fibers of the inferior pharyngeal constrictor and the circular muscles of the esophagus. Between the inferior constrictor muscle and the cricopharyngeal muscle is a relatively weak area known as Killian triangle (see Fig. 4.4 ). A pulsion pharyngoesophageal, or Zenker, diverticulum can form in Killian triangle, due to hypertrophy of the cricopharyngeus muscle or underlying dysmotility. There is a 2- to 4-cm high-pressure zone between the pharynx and the cervical esophagus, corresponding to the semicircular cricopharyngeal muscle. The upper esophageal sphincter is composed of the cricoid cartilage, the hyoid bone, and the cricopharyngeal and inferior pharyngeal constrictor muscles. The cricopharyngeus muscle includes a mixture of fast- and slow-twitch striated muscle fibers, allowing a basal tone but also permitting rapid changes for swallowing. The upper esophageal sphincter relaxes as intrapharyngeal pressure increases during swallowing, allowing the food bolus to enter the cervical esophagus.
The esophagus is closely related to the membranous trachea, and care must be taken during dissection of the cervical esophagus to avoid injury to the trachea ( Fig. 4.7 ). A tracheoesophageal fistula can also result from direct invasion, radiation of tumors in this area, or dilation of proximal radiation-associated or anastomotic strictures. Laterally, the esophagus is adjacent to the common carotid arteries and the thyroid gland.
The cervical esophagus is directly anterior to the vertebra. A cervical esophageal perforation or anastomotic leak can lead to a spinal abscess and should be drained by opening the neck to help prevent this complication. Anterior spinal procedures can also result in inadvertent esophageal injury. In addition, esophageal surgeons should be aware of previous anterior cervical spinal operations that could lead to adhesions to the esophagus and potential infection of spinal hardware.
The recurrent laryngeal nerves originate from the vagus nerves ( Fig. 4.8 ). The right nerve recurs posteriorly around the right subclavian artery, while the left nerve recurs around the aortic arch. Both recurrent nerves ascend in the tracheoesophageal groove, although the left nerve comes closer to the esophagus, since the cervical esophagus deviates to the left and the right nerve recurs around the subclavian more laterally. A nonrecurrent nerve occurs rarely on the right. Toniato et al. report an incidence of 0.1% (31/6000) of patients on the right, with none on the left. The recurrent laryngeal nerves also innervate the cricopharyngeal muscle and the cervical esophagus. Care must be taken to protect the left recurrent laryngeal nerve when dissecting out the cervical esophagus during a transhiatal esophagectomy or Zenker diverticulectomy. The fat in the tracheoesophageal groove containing the nerve should be sharply dissected from the wall of the esophagus, and care should be taken to gently retract the trachea medially with a finger to expose the esophagus, avoiding the use of any metal retractors on the nerve. With experience and these precautions, the incidence of recurrent laryngeal injury should be approximately 1%. Injury to the recurrent laryngeal nerve not only results in hoarseness but also affects the mobility of the cervical esophagus and function of the cricopharyngeal muscle, with impaired swallowing and an increased risk of aspiration. Injury to both recurrent nerves can result in bilateral vocal cord paralysis, with airway obstruction and the need for a tracheostomy.
The thoracic esophagus is 20 cm in length and extends from the thoracic inlet to the diaphragmatic hiatus (see Fig. 4.1 ). The esophagus passes through the middle mediastinum and shifts to the right at the level of the seventh thoracic vertebra, so the best approach to the mid-esophagus is through a right thoracotomy or thoracoscopy, for example, during an Ivor-Lewis or minimally invasive three-hole esophagectomy. However, the esophagus angulates to the left after passing through the diaphragmatic crura, and along with the location of the liver on the right, the best approach to the distal thoracic esophagus is from the left for a transthoracic hiatal hernia repair or resection of an epiphrenic diverticulum, even when the hernia or diverticulum extend into the right chest.
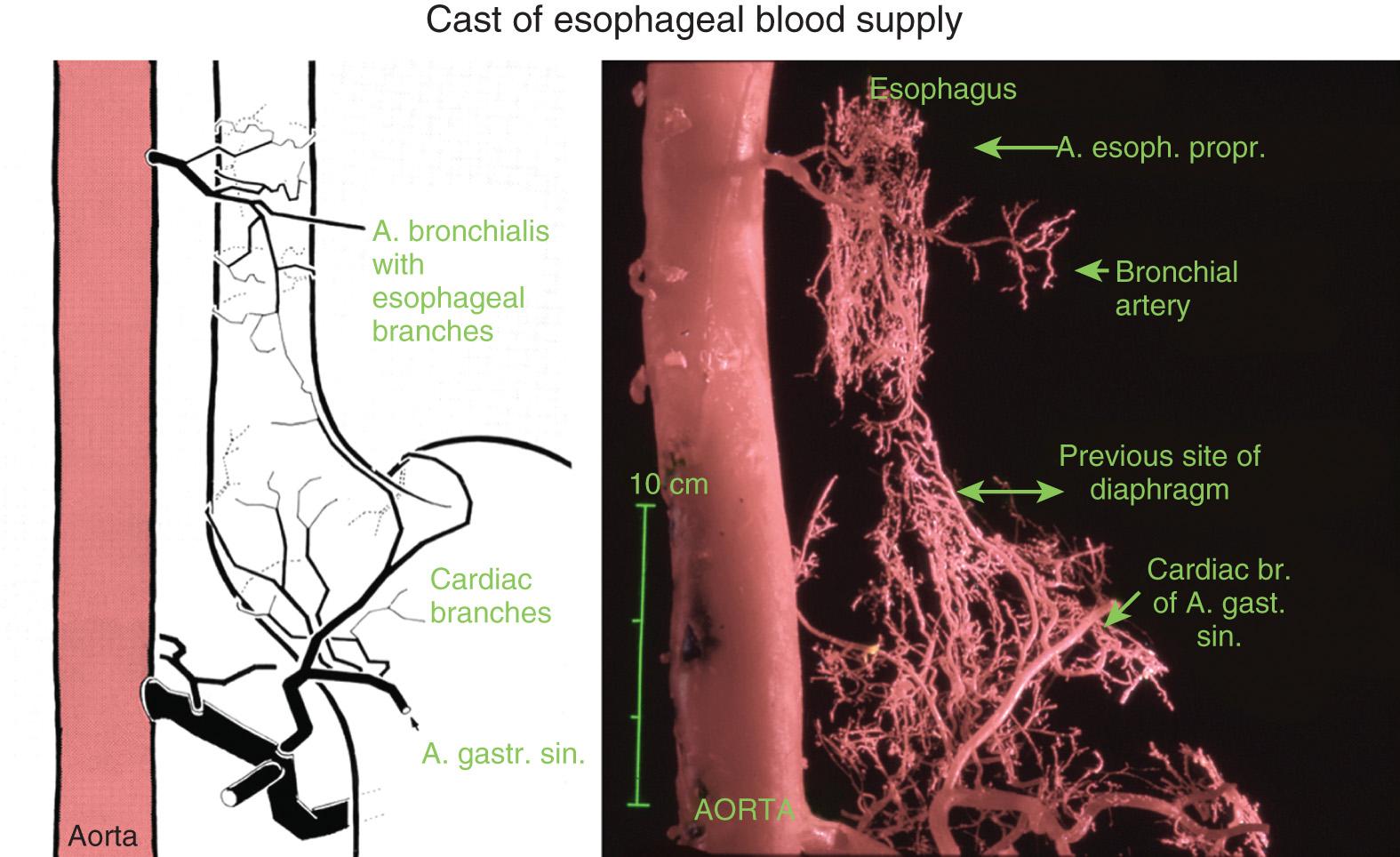
The arterial blood supply originates from the bronchial arteries, and the majority of patients have one right-sided branch and one to two left-sided branches. There are usually two esophageal branches from the descending aorta between the sixth and ninth thoracic vertebrae. There is a vast network of collateral vessels within the wall of the esophagus, allowing the esophagus to receive blood supply from larger vessels perfusing other organs such as the thyroid, trachea, and stomach ( Fig. 4.9 ). Because of this rich intramural network of small vessels, the esophagus can be completely mobilized from the stomach to the aortic arch, yet continue to be well perfused. However, care should be taken if the inferior thyroid artery has been ligated during a previous thyroidectomy. The arterial vessels supplying the esophagus branch into small, fine vessels at a distance from the esophageal wall, and bleeding can be controlled by packing the mediastinum, allowing for blunt dissection during a transhiatal esophagectomy. Venous drainage is through the azygos vein, with some drainage through the hemiazygos and bronchial veins.
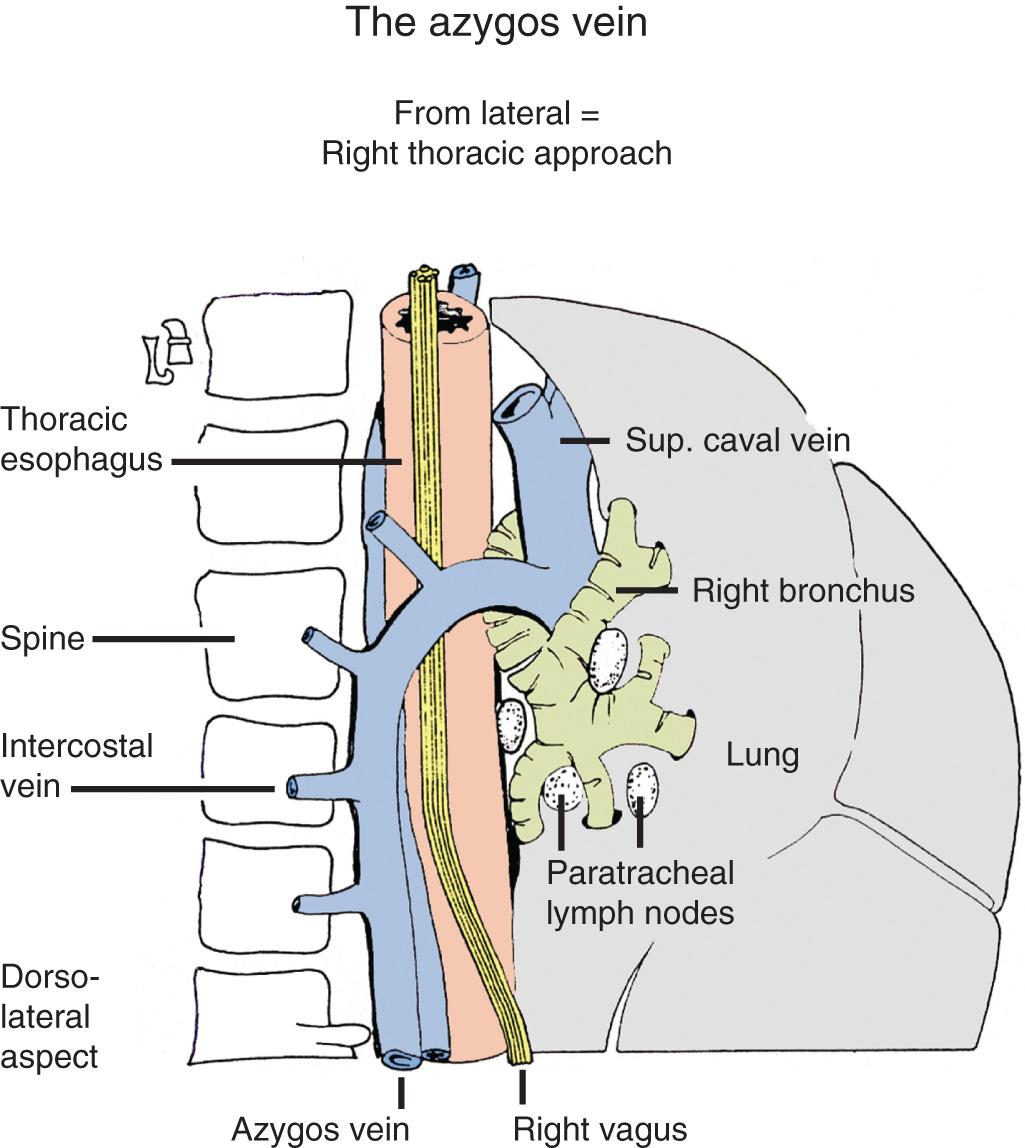
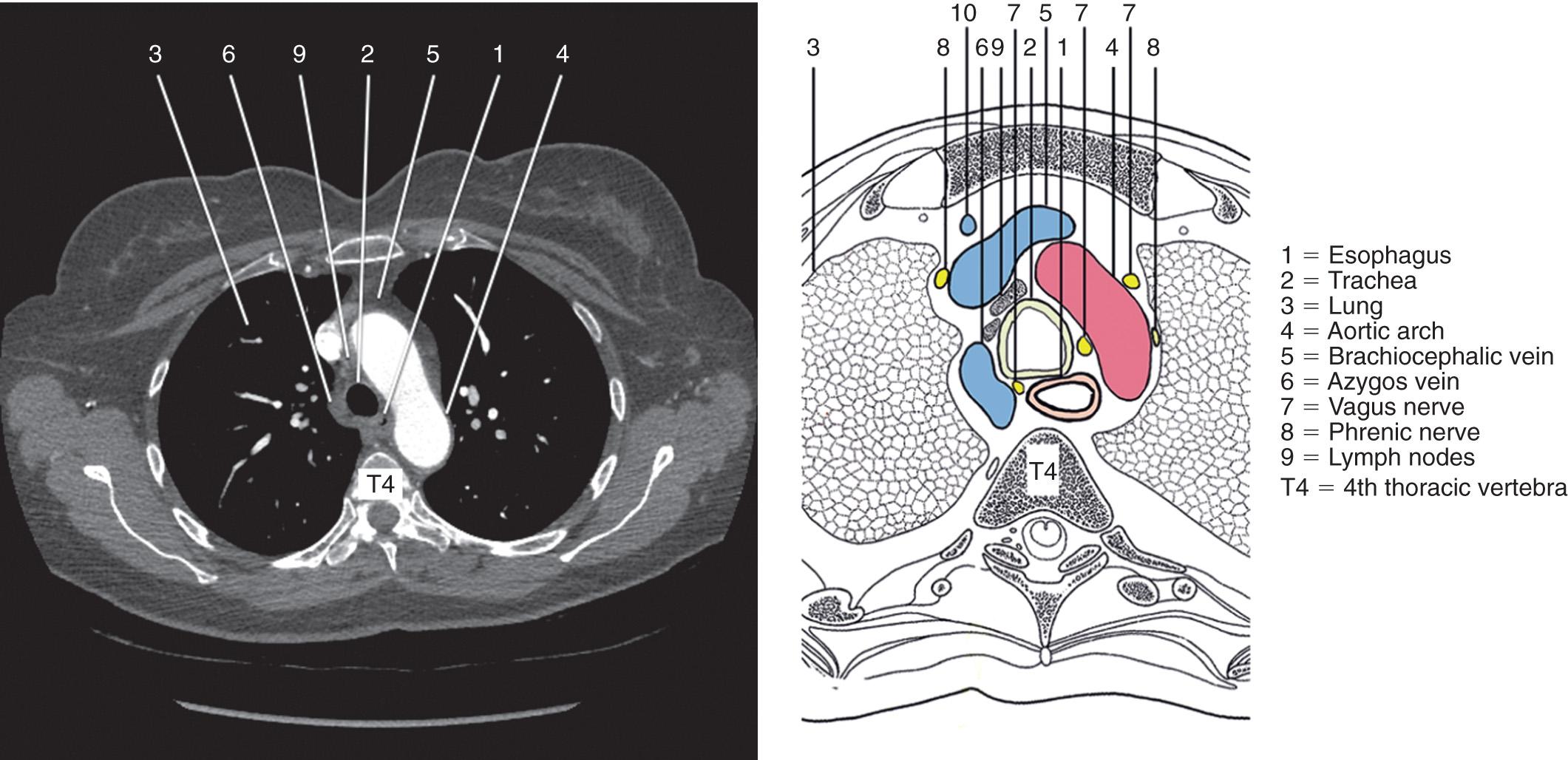
The thoracic esophagus is bordered by the mediastinal pleura on either side. The esophagus is surrounded by loose fibroareolar tissue. This loose investing tissue, with no dense fibrous attachments in the chest, allows the esophagus to be bluntly dissected during a transhiatal esophagectomy. During transhiatal or laparoscopic dissection of the esophagus, it is important to recognize entry into either pleural space. A chest tube is placed for drainage of blood during an esophagectomy, and a tension pneumothorax must be recognized during laparoscopy. In the upper thorax, the trachea is anterior, the azygos is on the right ( Fig. 4.10 ), and the left subclavian artery and aortic arch are to the left of the esophagus ( Fig. 4.11 ). The descending aorta turns posteriorly and continues to the left of the esophagus until T8, where the esophagus moves anterior to the aorta.
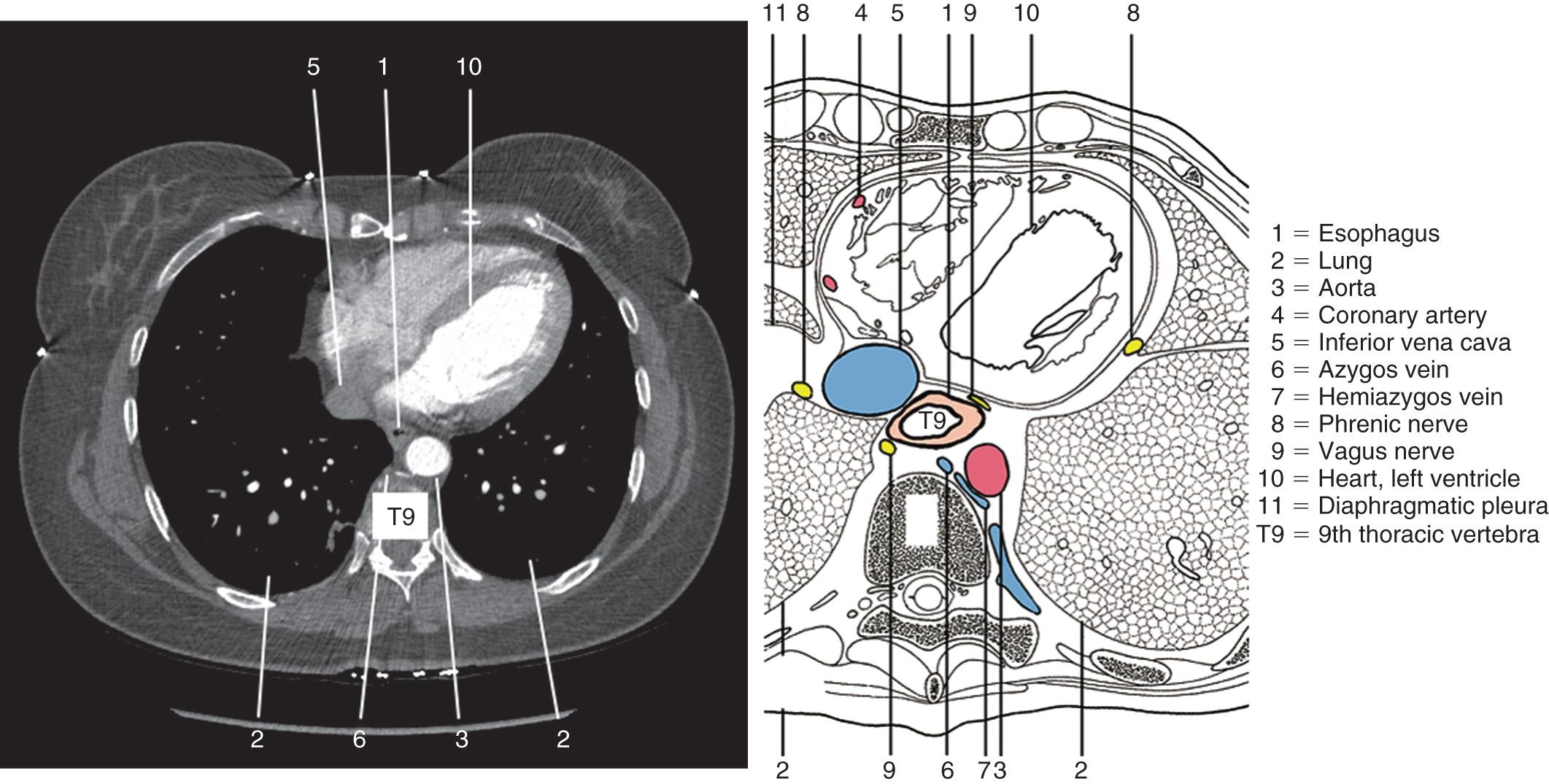
In the lower thorax, the pericardium and left atrium lie anterior to the esophagus ( Fig. 4.12 ). Invasion of the heart or the aorta in locally advanced esophageal cancer is unresectable and can be evaluated on a chest computed tomography with contrast or endoscopic ultrasound. Direct invasion of the aorta can also lead to an aortoesophageal fistula. Hematemesis in a patient with esophageal cancer can represent sentinel bleeding from an aortoesophageal fistula, which must be recognized early to prevent fatal exsanguinating hemorrhage. However, if the tumor just abuts these structures, often there is no invasion at intraoperative exploration. Posteriorly, the esophagus is adjacent to the spine from the thoracic inlet to T8, where the esophagus moves anteriorly to enter the esophageal hiatus. The left lateral distal esophagus is covered only with mediastinal pleura. As a result of the relative weakness in this area, spontaneous Boerhaave perforation occurs most commonly along the left lateral aspect of the distal esophagus.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here