Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Reconstruction of the head and neck following burn injuries presents great challenges and great opportunities. Successful treatment requires sound surgical judgment and technical expertise, as well as a thorough understanding of the pathophysiology of the burn wound and contractures. Many disciplines are required to successfully care for patients with burns of the head and neck. These include skilled nursing, experienced occupational and physical therapy, and psychological and social support systems. The surgeon must also have familiarity and expertise with nonsurgical treatment modalities such as pressure therapy, steroids, and laser therapy. Realistic expectations on the part of both patients and surgeons are essential to achieve successful treatment outcomes. Burns to the head and neck of a serious nature result in tissue injury with scarring, and complete removal of scars is not possible. A scar can only be modified or exchanged for another scar or tissue of a different variety. Despite this fundamental limitation, reconstruction of the burned face and neck creates great opportunities for plastic surgery to significantly improve functional and aesthetic deformities resulting in profound improvement for this large group of challenging patients.
Recent advances in technology and improved understanding of wound-healing physiology are transforming the ways we should look at, and think about, burn scars and contractures. This change in perspective is particularly important in the head and neck because normal appearance and normal function in this area are of paramount importance. The presence of visible scarring and even minimally grotesque deformity is particularly debilitating in the face and neck. Since the early 20th century and the brilliant work of Sir Harold Gillies reconstructing facial deformities with tubed pedicle flaps, scar excision in the head and neck and replacement with flap tissue, either from regional or distant donor sites, has dominated facial burn reconstruction thinking. This was further popularized by the concept of aesthetic unit scar excision coupled with ever-improving surgical ability to transplant tissue. It is time to rethink this paradigm. It is now possible to dramatically rehabilitate hypertrophic and contracted scars on the face and neck to the point where the scars are often the patient's best reconstructive anatomy. That is because the scars are autologous, in the right location, and the closest match to normal because they are the “original equipment.” Excision and replacement of facial scars creates iatrogenic donor sites and requires extensive surgery to replace the scars with uninjured tissue from other areas of the patient's body. This surgery is typically complex and morbid with potentially severe complications. Scar rehabilitation is minimally morbid and has few complications. The secrets to success with scar rehabilitation in the head and neck are accurate early diagnosis, conservative management, and the effective use of new technologies and treatments to enable patients to reap the maximum benefit from their own amazing wound-healing and scar remodeling capabilities ( Fig. 50.1 ). This new approach will be discussed in this chapter along with more traditional methods of reconstruction in the head and neck.

Burn injuries constrict and deform the face; distorting its features, proportions, and expression. Burns also alter the surface of the facial mask by causing scars and altering texture and pigmentation. The changes to the surface of the skin are deforming but are much less important to facial appearance than are the changes in proportion, features, and expression. The removal of scars should not be the primary goal of facial burn reconstruction. A normal-looking face with scars is always better looking than an even slightly grotesque looking face with fewer scars. Mature scars that result from burn injury will often be less conspicuous than surgically created scars after excision or surgically transferred flaps or grafts. The subtle and gradual transition between unburned skin and burn scar is an excellent example of nature's camouflage and can render scarring remarkably inconspicuous. New techniques of scar rehabilitation using lasers and carefully crafted, minimally morbid surgery helps scars blend even better. The principal goal of facial burn reconstruction should be the restoration of a pleasing and tension-free facial appearance with appropriate animation and expression. If this goal is kept in mind and is pursued with persistence and determination, the amount of improvement that can result after severe facial burn injury can be remarkable. Ignoring this basic principle can result in iatrogenic catastrophes during reconstructive surgery of the head and neck following burns.
Successful reconstruction of burn deformities of the head and neck requires a well-functioning and extensive team. Major burn deformities in this area can easily be intimidating and overwhelming. Experience and a specialized infrastructure are required to take care of these patients comfortably and successfully. Familiarity with their unique problems and a firm commitment to correcting their challenging deformities is required from all members of the reconstructive team. The care of a patient from the onset of a major burn involving the head and neck to a successful reconstructive outcome requires skill, patience, determination, and enthusiasm from all who are involved.
Although the main focus of this chapter is the reconstruction of established facial burn deformities, an understanding of the acute care of facial burn injuries is necessary in order for the surgeon to have an accurate perspective. Excision and grafting of deep second-degree and full-thickness burns has become the standard of care since it was first proposed in 1947. It remains controversial whether this is the optimal treatment for facial burn injuries. Early excision and grafting of the face is problematic because of difficulty in diagnosing the depth of the facial burn and accurately predicting an individual patient's long-term prognosis both functionally and aesthetically. Laser Doppler imaging is a validated way to improve diagnosis in these difficult cases and can decrease the risk of overly aggressive excision. Preventing unnecessary early excision is particularly important with current improved techniques to rehabilitate hypertrophic scars. The overwhelming majority of facial burns treated conservatively with a moist regimen of topical antibiotics will heal within 3 weeks. Burns that are clearly full-thickness are best treated by early excision and grafting within 7–10 days to promote early wound closure and minimize contractile forces ( Fig. 50.2 ). The problem cases are those where healing has not occurred by 3–4 weeks or longer. Early tangential excision and grafting has been proposed for these patients in order to achieve more favorable healing with less eventual contracture deformities. Proponents of conservative therapy argue that early excision and grafting may result in a patient with a grafted face who would otherwise have healed favorably by successfully epithelializing their partial-thickness burn from skin appendages. Conservative management has been facilitated by the myriad ancillary techniques currently available to favorably influence the healing of facial burns such as pressure, silicone, silicone-lined computer-generated facemasks, topical and intralesional steroids, vitamin E, massage, and treatment with pulsed dye lasers (PDLs) and ablative fractional CO 2 lasers. Impressive results have been obtained by advocates for early excision and grafting. Very good outcomes, however, can also be achieved by being more conservative with this difficult group of patients ( Fig. 50.3 ). The benefits in appearance and function of rehabilitated scars over early excision and grafting are dramatically demonstrated by the patients and accompanying videos in Figs. 50.4 and 50.5 . Committing a patient to a grafted face should only be done when it is clearly the best alternative. The majority of acute facial burns are treated conservatively in most burn centers, with early excision and grafting limited to those cases where it is clear that a full-thickness burn injury has occurred.



Superficial-thickness, second-degree burns usually heal without scarring or pigmentary changes. Medium-thickness, second-degree burns that epithelialize in 10–14 days usually heal without scarring, although there can be long-term changes in skin texture and pigmentation. Deep-thickness, second-degree burns that epithelialize after 21 days or longer are unpredictable and must be carefully managed because they have a propensity to develop severe late hypertrophic scarring ( Fig. 50.6 ). These patients should be closely monitored after initial healing and, at the first sign of hypertrophy, must be managed with all available ancillary treatment modalities. Pressure garments have been shown over several decades to be effective in suppressing and reversing hypertrophic scarring. Adding silicone to pressure therapy seems to increase its efficacy. Computer-generated clear face masks lined with silicone have improved the ability to deliver pressure to facial hypertrophic scars and are better tolerated by patients ( Fig. 50.7 ). The vascular-specific PDL decreases hyperemia and seems to diminish hypertrophy. When tension plays a role in the development of early hypertrophic scarring, relief of the tension with either focal Z-plasty or judicious release and grafting can be very helpful. Ablative fractional CO 2 laser therapy can be used to decrease tension and also deliver corticosteroids into the hypertrophic scars with encouraging results. Definite full-thickness facial burns should usually be excised and grafted unless focal and small.


Facial burn reconstruction should be based on an overall strategy and a clear understanding of the fundamental problems. Many reconstructive techniques have been described in the literature and can result in improvement if the strategic goals are appropriate. The new era of scar rehabilitation has changed older strategies, and where this will eventuate is unclear at this time. It seems likely that scar excision and replacement with other parts of the patient's body will be less common in the future. The best reconstructive plan for the facial scar tissue will be scar rehabilitation using all available modalities to preserve its unique advantages as much as possible. Improved outcomes will be achieved with a judicious combination of contracture releases by Z-plasty, grafts, and flaps, followed by appropriate scar revision and laser therapy. Laser therapy preceding scar revision improves scar quality and facilitates surgery. Extensive scar excisions in aesthetic units and replacement with microvascular free tissue transfer from distant sites will likely become less frequent. The role of face transplantation in burn reconstruction of the head and neck is unclear at this time.
Deep second- and third-degree burns heal by contraction and epithelialization. The more severe the burn injury, the more contraction takes place during the healing process. The changes in facial appearance following a deep second-degree burn injury are dramatically demonstrated in Fig. 50.8 . Three weeks following a deep second-degree burn, the patient's facial features and proportions remain essentially normal. Six months later, contractile forces have deformed the facies in a pattern that is repeated to a variable degree in virtually all severe facial burns. These changes make up the stigmata of facial burn injury and are listed in Box 50.1 . The eyelids are distorted with ectropion, the nose is foreshortened with ala flaring, the upper lip is shortened and retruded with loss of philtral contour, the lower lip is everted and inferiorly displaced, the lower lip is wider than the upper lip in anterior view. The tissues of the face and neck are drawn into the same plane with loss of jawline definition. The severity of these changes is proportional to the severity of the injury.

Lower eyelid ectropion
Short nose with ala flaring
Short retruded upper lip
Lower lip eversion
Lower lip inferior displacement
Flat facial features
Loss of jawline definition
Fortunately the majority of facial burn injuries are not severe and do not involve the entire face. A relatively small number of patients sustain injuries that deeply involve the entire face, such as shown in Fig. 50.8 . It can be helpful to separate patients with facial burn deformities into two fundamentally different categories, as described in Box 50.2 . Type I deformities consist of essentially normal faces that have focal or diffuse scarring from their burns and may have associated contractures. Type II deformities make up a much smaller number of patients who have “pan-facial” burn deformities with some or even all of the facial burn stigmata. Although these categories are not rigidly defined, and there are some patients who do not fit neatly into one or the other, understanding the fundamental difference between these two groups of patients can help define treatment goals. It can also aid in selecting the most appropriate methods for reconstructive surgery.
Type I
Essentially normal facies with focal or diffuse burn scarring with or without contractures
Type II
Pan-facial burn deformities with some or all of the stigmata of facial burns
Patients with type I deformities have an essentially normal facial appearance despite scars from their burns. In these patients, one must be certain that surgical intervention does not adversely alter normal facial features or create distortion from iatrogenically induced tension. Overall facial appearance should not be sacrificed in an effort to “excise scars” ( Fig. 50.9 ). The best reconstructive options today for patients with type I facial burn deformities are laser therapy combined with scar release and revision with Z-plasties when indicated or tissue rearrangement with local flaps. The PDL was the first laser to have demonstrated efficacy in the treatment of hypertrophic and contracted facial burn scars and can be helpful for decreasing post-burn erythema and treating persistently erythematous burn scars. Z-plasties in combination with the PDL can be a powerful scar-improving combination ( Fig. 50.10 ). Full-thickness skin grafts are excellent for focal contractures. Excision of scars and resurfacing operations in aesthetic units and major flap transpositions, with or without tissue expansion, are rarely indicated.


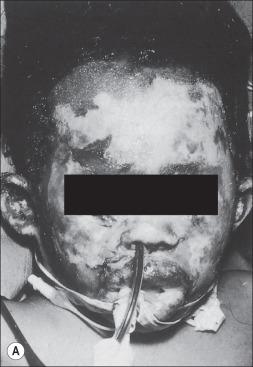
The much less frequently encountered group of patients with type II facial burn deformities presents a completely different clinical situation. Examples of patients falling into the type II category are shown in Fig. 50.11 . The surgical goals for this group of patients should be the restoration of normal facial proportion and, as much as possible, the restoration of the position and shape of normal facial features. The intrinsic and extrinsic contractures that exist in these patients require large amounts of skin. The correction of these contractures should be carried out in a carefully planned and staged fashion. The best sequence of operations is usually the following: eyelids, lower lip and chin, upper lip, cheeks, nose, and then other residual deformities. As each area is reconstructed, the addition of skin results in the relief of tension, which benefits other areas of the face. Excision of normal skin or elastic healed second-degree burned skin is almost never indicated. After facial proportion has been achieved and facial features have been restored to their normal location and shape without tension, scar revision can be carried out to smooth and blend the remaining junctional scars ( Fig. 50.12 ).


Normal faces are a mosaic of colors, textures, wrinkles, and irregularities. In a face that has undergone major burn injury, a mosaic appearance of scars, grafts, pigmentary abnormalities, and other flaws can be attractive as long as the facial features are restored to a normal location and are sufficiently loose and mobile for normal and appropriate facial expression. Laser therapy with vascular and fractional ablative CO 2 devices further blends, obscures, thins, and softens scars, enhancing facial expression and a more natural appearance ( Fig. 50.13 ). Cosmetics can be useful for blending and camouflaging areas of pigmentary and textural abnormality, particularly in females.

Burn injuries result in open wounds that either heal by contraction and epithelialization or are closed by skin grafting. Contractures result from both of these forms of wound healing. Contractures are either intrinsic or extrinsic. Intrinsic contractures result from loss of tissue in the injured area with subsequent distortion of the involved anatomic part. Extrinsic contractures are those in which the loss of tissue is at a distance from the affected area but the distorted structures, such as eyelids or lips, are not injured themselves. Corrective measures should be directed at the cause of the contracture in order to provide optimal benefit and prevent iatrogenic deformities. It is helpful to minimize the amount of skin and scar excised when correcting facial contractures. When tension is released, many scars will mature favorably and become inconspicuous. Even long-standing scars will respond to a change in their environment. Healed second-degree burns under tension may be unattractive but when restored to a tension-free state can be superior in function and appearance to any replacement tissue. Minimizing excision also decreases the amount of new skin that must be provided in the reconstruction. Every effort should be made to relieve tension from the face when performing burn reconstruction. Tight faces are never attractive. Tight scars are always hypertrophic and erythematous. Relaxed scars are happy scars. The fractional ablative laser has created a new paradigm for the management of tight, hypertrophic, erythematous, and even ulcerated pan-facial scarring with contractures. It is a clearly more powerful and efficacious treatment modality than the PDL. The patient shown in Fig. 50.13 is a perfect example of this beneficial change in the management of facial burn scars. Her scars were more diffuse and severe than those of the patients shown in Fig. 50.9 who were severely deformed by scar excision surgery. Her face is essentially normal after the rehabilitation of her “original equipment.”
The concept of facial aesthetic units has profoundly affected plastic surgical thinking since its introduction by Gonzalez-Ulloa. Initially conceived as the ideal approach for resurfacing the face following burn injury, this important concept has been emphasized in virtually all subsequent writings about facial burns. It is important to keep facial aesthetic units in mind during burn reconstruction, but the desire to adhere to this concept should not supersede common sense. When small, unburned, and unimportant islands of skin are in an aesthetic unit that is being resurfaced, they can be sacrificed. Otherwise the excision of normal facial skin is rarely indicated in burn reconstruction. All burned faces to some degree are mosaic. Scar revision with Z-plasties is an excellent technique to camouflage scars in a burned face. Mosaic faces that are proportional, tension free, and normally expressive appear much better in real life than they do in images. Lasers, as noted previously, also aid in obscuring marginal scars and add to the camouflage effect.
The Z-plasty operation is a powerful tool in the surgeon's armamentarium for facial burn reconstruction. The Z-plasty has been used for more than 150 years to lengthen linear scars by recruiting lax adjacent lateral tissue. Z-plasty can also cause a profound beneficial influence on the physiology of scar tissue when it is carried out within the scarred tissues rather than after excising them. The physiology of this phenomenon is related to the immediate and continuing breakdown of collagen that occurs in hypertrophic scars following the relief of tension. Z-plasty also narrows scars at the same time that it lengthens them. In addition, the Z-plasty adds to scar camouflage by making the borders of the scar more irregular. In order for Z-plasties to lengthen a burn scar and restore elasticity, the lateral limbs of the Z-plasty must extend beyond the margins of the scar. The improvement in the appearance of facial scars following Z-plasty and without any scar excision can be dramatic, particularly when combined with PDLs and fractional ablative laser treatments ( Figs. 50.1, 50.10, 50.13, 50.19 ).
Hypertrophic scarring is a frequent complication after partial-thickness facial burn injuries that take longer than 3 weeks to completely epithelialize. Despite conservative management and close monitoring, hypertrophic scarring can become severe during the first 2 years after the burn ( Fig. 50.6 ). The PDL has emerged as a successful treatment modality during this period of scar proliferation and is an effective alternative to scar excision in patients with hypertrophic facial burn scars. Multiple studies have demonstrated its beneficial effect on scar erythema and hypertrophy. The PDL also rapidly decreases pruritus and pain and provides an additional, low-morbidity therapeutic intervention for patients and their families during the often prolonged period of scar maturation. Restoration of hypertrophic facial scars to their previous state of a flat, epithelialized surface is a superior outcome to surgical excision with its concomitant increase in facial tension. The development of fractional ablative and nonablative laser therapy using various types of lasers, including CO 2 and erbium-YAG, offers promising new options for the management of facial burn scars in the future.
Skin grafts are an essential part of facial burn reconstruction. Surgical decisions regarding donor site selection, the use of split-thickness versus full-thickness grafts, the timing of intervention, and the postoperative management of grafts often determine the success or failure of facial burn reconstruction. Split-thickness skin grafts contract more than full-thickness grafts, wrinkle more, and always remain shiny, with a “glossy finish” look. Split-thickness skin grafts should be used primarily in the periphery of the face unless the limited availability of donor sites requires their use in more prominent areas. Split-thickness skin grafts can be excellent for upper eyelid releasing and resurfacing. Hyperpigmentation of split-thickness grafts on the face is a frequently occurring problem in dark-skinned patients, particularly those of African descent.
The full-thickness skin graft is a reliable workhorse in facial burn reconstruction. The broad, central, conspicuous areas of the face such as the cheeks, upper and lower lips, and dorsum of the nose are excellent sites for the use of full-thickness grafts. The missing or damaged parts in the vast majority of even severe facial thermal burns are the epidermis and the dermis, and that is what full-thickness skin grafts provide. After facial burns, the subcutaneous fat may be compressed or distorted by contractures but it is rare that it is injured or completely lost. Adequate skin must be provided when doing definitive resurfacing operations with full-thickness grafts. Contractures must be overcorrected, and postoperative management with conformers and pressure is essential. Full-thickness skin grafts are very reliable when used electively in the face for reconstruction after burns.
Flaps can be useful for facial burn reconstruction, but they must be used judiciously and skillfully, recognizing their problems and limitations. The thickness of skin flaps from all distant donor sites is greater than that of the normal facial skin. The face is tight following burn injury, and flaps tend to contract when transferred. They can therefore compress or obscure underlying tissue contours. Transposing or advancing flaps from the neck and chest up to the face can easily create extrinsic contractures that adversely affect facial appearance. When flaps have been enlarged by tissue expansion, they are even more dangerous in this regard. Contractures with a downward vector create a “sad” facial appearance that is distressing to patients ( Fig. 50.9 ). Cervicopectoral flaps provide the best color match in color and texture to facial skin. Distant flaps, whether transferred by traditional technique or microsurgery, share the common flaw of poor match in terms of color and texture.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here