Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Achieving aesthetic surgical outcomes after reconstruction of cutaneous cheek defects requires knowledge of cheek anatomy and facial aesthetic regions. The size and location of the defect and the structures adjacent to the defect are assessed to determine where tissue can be recruited for construction of skin flaps without adversely affecting the nose, lips, and eyelids by secondary tissue movement. Analysis of each cheek defect is essential, and fundamental concepts of cutaneous flap biomechanics should be addressed (see Chapter 3 ) to facilitate tension-free wound closures with optimally positioned scars.
The cheek is the largest aesthetic region of the face and has a broad, slightly convex contour. The aesthetic region of the cheek may be divided into the zygomatic, medial, lateral, and buccal units as a conceptual framework for determining reconstructive options. This concept is based on the anatomic characteristics of inherent skin elasticity and mobility and the presence of adjacent mobile facial structures. The following discussion of reconstruction of cutaneous defects of the cheek is organized by aesthetic units of the cheek and by size of the defect. Each section highlights the facial structures that can be distorted by secondary tissue movement in the process of reconstructing a defect and details tissue amenable for recruitment to construct local flaps.
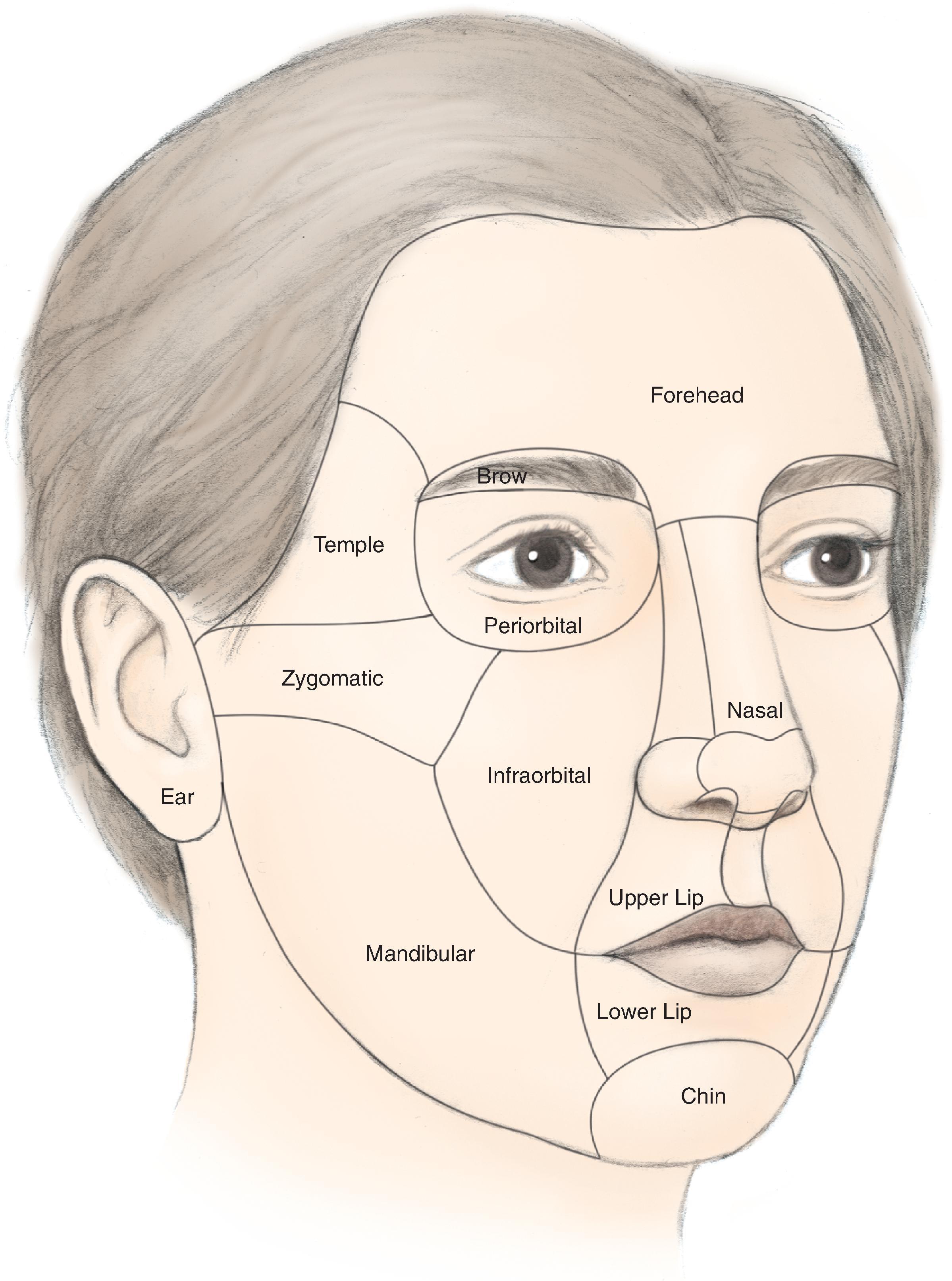
The cheek is the largest facial aesthetic region and is juxtaposed to the orbital, nasal, and lip aesthetic regions. The aesthetic region of the cheek has the following boundaries: inferior bony orbital rim, nasofacial (cheek-nose junction) sulcus, line from the lateral canthus to the root of the helix, preauricular crease, melolabial crease, labiomandibular crease, and inferior border of the mandible ( Fig. 20.1 ). The cheek can be conceptually divided into areas based on the difference of underlying bone, soft tissue, skin quality, and skin laxity. On the basis of these anatomic differences, there are four aesthetic units: medial, lateral, zygomatic, and buccal. The skin of the medial and buccal units is thicker and more mobile than the skin of the other units of the cheek. The skin of the lateral unit is moderately fixed to the underlying fascia, and the skin of the zygomatic area is quite fixed, in part by the cutaneous retaining ligaments in the region. This unit also has the least skin laxity.
Several important ligaments collectively referred to as cheek retaining ligaments support the soft tissues of the cheek. Retaining ligaments in the area of the zygoma (known as McGregor’s patch ) serve as strong bone anchors for supporting the skin overlying the zygoma. More inferiorly and anteriorly, a dense attachment to the skin known as the mandibular retaining ligament is present at the cheek where it joins the lower lip. This ligament accounts for the formation of the labiomandibular crease. Fibrous attachments of the superficial musculoaponeurotic system (SMAS) to the cheek skin at the junction of cheek and upper lip create the melolabial crease. The labiomandibular and melolabial creases provide important landmarks for concealing incisions and represent aesthetic boundary lines between the cheek and the upper and lower lips. The contour of the cheek is because of the convexity of the maxilla and the malar fat pad. The fat pad is well known to plastic surgeons for its role in the aging of the midface. In addition to retaining ligaments, the cheek is supported by the muscles of facial expression. Most notable is the zygomaticus major positioned deep to the malar fat pad and invested by the SMAS.
Lymphatic drainage of the cheek is primarily to the submental, submandibular, and preauricular lymph nodes. Additional drainage occurs to the second echelon of lymph nodes in the superior jugular chain. The vascular supply to the cheek skin is derived from three major sources, which perfuse the dermal and subdermal plexuses. The superficial temporal artery provides a minor supply through the transverse facial branch. The infraorbital artery provides collateral supply to the midcheek with anastomotic connections to the facial artery. The facial artery and its continuation as the angular artery provide the majority of blood to the skin of the cheek. The venous drainage is based on vessels that follow the named arterial supply.
The facial nerve provides motor innervation to the muscles of facial expression that form a base on which the subcutaneous tissue and skin of the cheek rest. The majority of sensory innervation of the cheek is provided by branches of the second division of the trigeminal nerve through the infraorbital nerve. The third division of the trigeminal nerve contributes to the sensory supply of the lateral cheek through the auriculotemporal nerve and of the inferior cheek through the mental nerve.
The aesthetic units of the cheek vary in terms of skin color, texture, and thickness. These factors determine the preferred reconstructive option. To select the best option, it is helpful to assess the mobility and laxity of skin surrounding the defect and to determine which facial structures may be distorted by secondary tissue movement. Particularly important in this regard are the nasal ala, lips, and lower eyelid. It is also important to mentally outline the borders of the cheek and adjacent facial aesthetic regions and to determine where the final scars will lie after reconstruction.
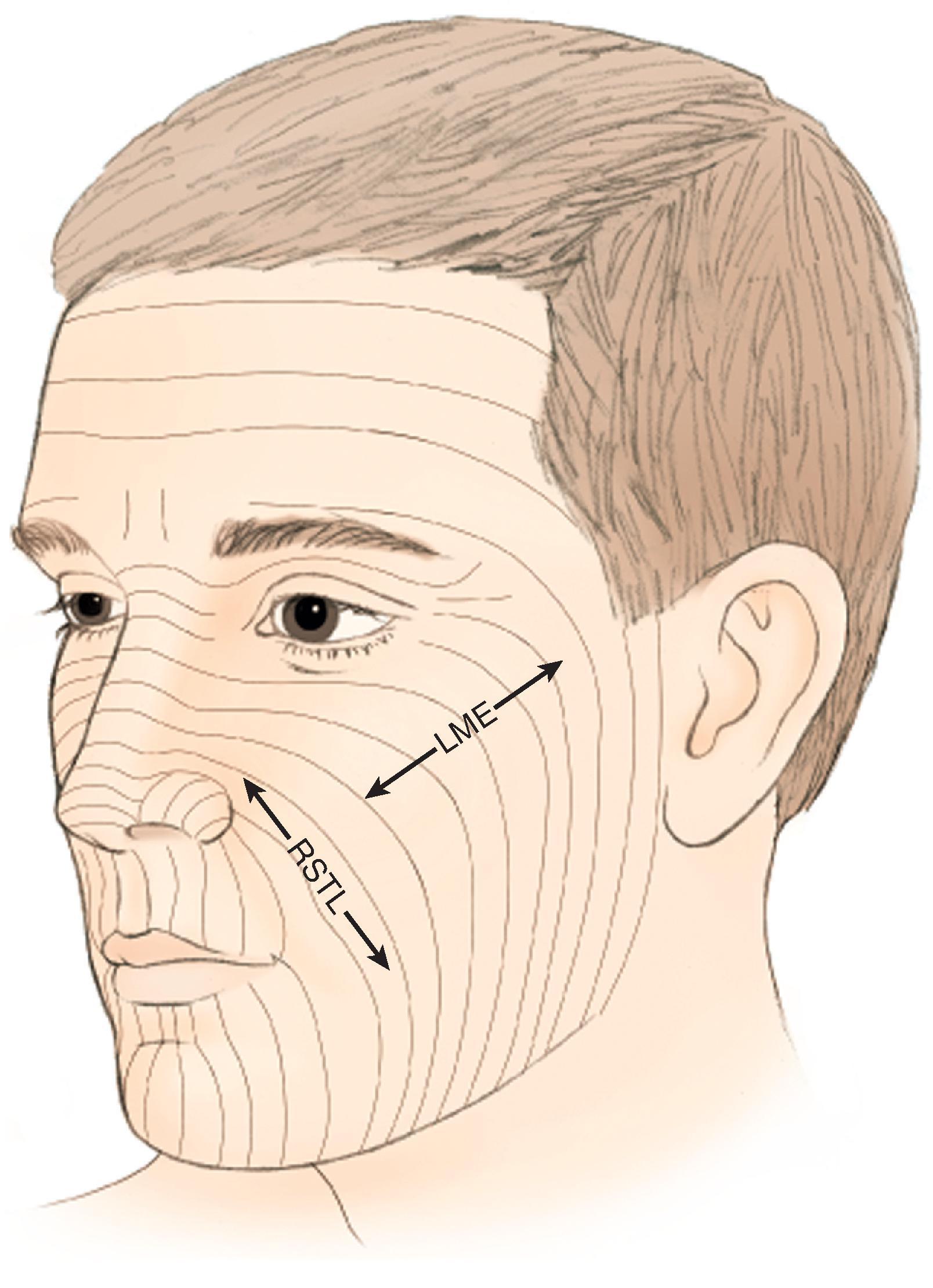
When possible, scars should be positioned at the border of aesthetic units to provide the best camouflage. When scars cannot be placed in borders of aesthetic units, they should be aligned parallel to relaxed skin tension lines (RSTLs), which are curvilinear in the cheek ( Fig. 20.2 ). RSTLs are a result of the intrinsic elasticity of the skin and are perpendicular to lines of maximal extensibility. Therefore wound closure oriented in an axis parallel to RSTLs results in less wound closure tension and more favorable scar camouflage. Wrinkles located in the lateral canthal region are largely because of the action of the orbicularis oculi muscle and provide a useful site in which to place incisions. In general, the boundaries of cheek aesthetic units and facial creases are more favorable locations than the RSTLs for the positioning of scars.
A number of clinical factors influence the method selected for reconstruction of cutaneous defects of the cheek. The etiology of the defect is important to consider in evaluating reconstructive options. This is particularly important when one is reconstructing defects after surgical excision of melanoma. In these cases, primary wound closure, healing by secondary intention, or skin grafting may be the preferred method of repair if the risk for recurrent disease is high. Although these methods of wound repair may offer poorer aesthetic results, they may clinically provide for better tumor surveillance. This decision must be individualized; however, it may be prudent to choose the simplest option, reserving local flap reconstruction for a second stage after an appropriate time interval to ensure that recurrence of the melanoma is unlikely. Nonmelanoma skin cancer, primarily basal cell carcinoma and squamous cell carcinoma, is often treated with micrographic surgery, with a cure rate approaching 99%. Given the low rates of recurrence, the procedure that provides the most aesthetically appealing result can be selected within the confines of the patient’s desires and general health condition. Micrographic surgery typically results in a defect with 45° beveled edges. Failure to remove this beveled tissue at the time of reconstruction may cause a barrier to precise wound edge apposition and eversion. “Freshening the edges” of the defect by perpendicularly excising the beveled tissue margins is a useful technique for providing healthy viable wound margins. If skin grafting is selected for repair of the defect, however, the beveled edge is advantageous and may be intentionally maintained to lessen the discrepancy in thickness between the skin graft and the native cheek skin. Postoperative radiation therapy is at times indicated, and in this setting, the reliability of the method of reconstruction selected must be considered.
The patient’s health history and social habits are factors that influence the options for reconstruction of cutaneous defects of the cheek. Patients with a prior history of irradiation, smoking, or diabetes mellitus may exhibit impaired wound healing. In these circumstances, the most reliable flap is selected. When a patient is diabetic, blood glucose levels should be optimally controlled before surgery. For patients who smoke, every effort should be made to encourage the patient to stop smoking.
Patients receiving immunosuppressive therapy, most notably those with a transplanted organ, often have histologically aggressive skin cancers coupled with impaired healing capabilities. In these patients, there is a high probability for development of other cutaneous malignant neoplasms. There is also an increased likelihood of local flap necrosis compared with patients not taking immunosuppressive medications. All of these factors may lead the surgeon to select a reconstructive option that sacrifices aesthetic results in exchange for tissue preservation with the knowledge that additional flaps will be necessary in the future to treat additional cutaneous malignant neoplasms.
The size of a cutaneous cheek defect is an important factor affecting the surgical approach to reconstruction of the cheek. When the defect occupies more than 50% of the surface area of an aesthetic unit, the remaining skin of the unit may occasionally be removed and the entire unit covered with a cutaneous flap. For smaller defects, repairs are designed that preserve the remaining normal tissue and place scars at the cheek perimeter or parallel with RSTLs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here