Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Collapse and atelectasis are terms which are often used synonymously and refer to loss of volume within the lung. In North America, the term collapse is often reserved to denote complete loss of volume within an entire lobe or lung. Atelectasis can be described according to extent (linear, plate-like or subsegmental atelectasis, sublobar and lobar atelectasis) or due to the underlying aetiology: compression or passive atelectasis (e.g. by pleural effusion, pneumothorax or bulla) and obstructive or post-stenotic atelectasis. Rounded atelectasis refers to a specific type of a sublobar atelectasis associated with previous (often haemorrhagic) exudative pleural effusion (e.g. post-thoracotomy, trauma and asbestos exposure). It is associated with adjacent visceral pleural thickening and has characteristic computed tomography (CT) appearances which are described elsewhere.
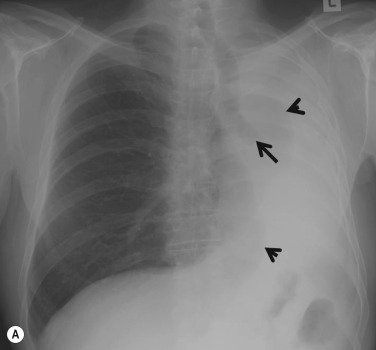
Broadly, lobar collapse can be divided into those due to endobronchial obstruction (either intrinsic or extrinsic) and those without obstruction. The common causes differ slightly between adults and children. In adults the frequent causes of intrinsic obstruction are tumours and mucous plugs. In the clinical context of a middle-aged or elderly smoker, lobar collapse should always be suspected to be due to a bronchogenic carcinoma until proved otherwise. All cell types of bronchogenic carcinoma can potentially cause intrinsic large airway obstruction and produce segmental, lobar or whole lung collapse ( Figs 7.1 and 7.2 ). More rarely, foreign bodies, broncholiths and focal bronchostenosis due to inflammation or trauma may be encountered. In children, causes such as inhaled foreign bodies or mucous plugs are common, with tumours being very rare.
Intrinsic:
Bronchogenic carcinoma
Bronchial carcinoid
Adenoid cystic carcinoma
Metastases (e.g. breast, renal cell and colonic carcinoma, melanoma, sarcoma)
Lymphoma
Benign tumours (e.g. lipoma, hamartoma, papillomas, endometriomas)
Granulomatous diseases (e.g. sarcoidosis and tuberculosis)
Miscellaneous conditions (e.g. aspirated foreign bodies, mucous plugs, gastric contents, malpositioned endotracheal tubes, bronchial torsion or rupture, amyloidosis, Wegener granulomatosis)
Extrinsic:
Hilar or mediastinal lymphadenopathy (commonly due to bronchogenic or breast carcinoma)
Mediastinal masses
Fibrosing mediastinitis
Aortic aneurysms and congenital vascular anomalies
Cardiac enlargement
Miscellaneous conditions (e.g. passive collapse due to pleural fluid or pneumothorax, radiation-induced collapse, tumour replacement [adenocarcinoma])

The cardinal radiographic features of lobar collapse are increased opacity of the affected lobe and volume loss. The latter can be inferred by direct and indirect signs. Direct signs of volume loss refer to displacement of interlobar fissures, pulmonary vessels and bronchi, whereas indirect signs include compensatory shifts of adjacent structures such as hyperinflation of other lobes. The effects of a lobar collapse are often maximal on immediately adjacent structures; for example, an upper lobe collapse often results in a shift of the superior mediastinum, whereas a lower lobe collapse often demonstrates elevation of the posterior part of the diaphragm in particular. However, the general principles and fundamental radiographic signs are similar for all lobes.
A collapsed lobe appears radiographically dense due to a combination of retained secretions or fluid within the lobe and reduction in aeration of the lobe. However, retained fluid is the dominant process, resulting in increased opacity of a partially collapsed lobe, as virtually complete collapse is required to displace sufficient air for the normally radiographically hyperlucent lung to appear dense.
Displacement of fissures is a reliable feature of lobar collapse, and is generally characteristic depending on the affected lobe. The pulmonary vessels and bronchi become crowded together in the affected lobe as the lung loses volume. The sign may be one of the earliest seen in lobar collapse and can often be readily appreciated by comparison with previous radiographs.
Hilar elevation on the posteroanterior (PA) chest radiograph is a well-known sign of upper lobe collapse; the ipsilateral interlobar and lower lobe arteries remain visible as these structures are still outlined by aerated lung. It would seem logical to consider ‘hilar depression’ to be a sign of lower lobe collapse, but some authorities believe the small hilum to be a more accurate description. This is due to the fact that when a lower lobe collapses, the opaque, collapsed lobe obscures the lower lobe artery that lies within it, and the interlobar artery is usually rotated so the margin is no longer in profile to the frontal x-ray beam. Consequently, it is difficult to recognise the hilum as being depressed and, instead, smaller vascular structures are noted at the expected position of the hilum. Occasionally, confusion with a central hilar mass/adenopathy can arise if the convex margin of an interlobar artery remains visible due to minimal rotation.
As well as vascular reorientation, hilar bronchial alterations also occur. The central large bronchi undergo characteristic changes in position with collapse of either the upper or lower lobe. When either upper lobe collapses significantly, the ipsilateral main bronchus becomes more horizontally orientated than usual; hence the bronchus intermedius and the left lower lobe bronchus swing laterally. Conversely, when either lower lobe collapses, each main bronchus is more vertically orientated than usual, with a medial swing of the bronchus intermedius on the right and the lower lobe bronchus on the left.
Compensatory hyperinflation of adjacent lobes occurs with lobar collapse, resulting in fewer vessels per unit volume of lung. It is often easier to detect a paucity of vessels, which are more widely spaced than on the unaffected side, than subtle increased radiolucency. In isolation, the sign may be due to causes other than lobar collapse and other confirmatory features should be sought before making the diagnosis. The normal lung parenchyma should expand proportionally to compensate for the degree of collapse and often the greater the degree of lobar collapse, the greater the compensatory overinflation. Therefore when small lung volumes are involved, the hyperinflation usually only involves the remainder of the ipsilateral lung, whereas with larger volumes, the contralateral lung may expand across the midline. On a frontal radiograph the lung may expand across the midline superiorly, thus displacing the anterior junctional line to the contralateral side (see Fig. 7.1A ). On a lateral view, the anterior mediastinum appears hyperlucent (see Fig. 7.1B ). Displacement of the azygo-oesophageal line and posterior junctional line on the PA radiograph, which denote protrusion of contralateral lung through other weak areas between the oesophagus and vertebral column and the retrocardiac space, respectively, may be more difficult to recognise. Although the term ‘mediastinal herniation’ is sometimes used, some authorities emphasise that there is no actual mediastinal defect or hiatus and the sign more accurately denotes displacement of mediastinal structures.
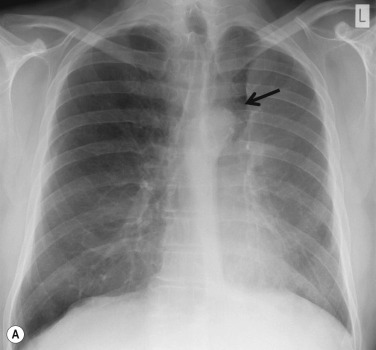
A divergent or parallel pattern of vascular reorientation seen near the hilum has been described in marked upper lobe collapse. The pattern is seen more commonly on the left than on the right, as a result of the different degree of compensatory overinflation in the superior segment of the ipsilateral lower lobe on each side. The right middle lobe can also overinflate in compensation, which further explains the lesser degree of overinflation of the superior segment of the right lower lobe. The sign of vascular reorientation can be helpful when unusual patterns of upper lobe collapse are present. Hyperexpansion may also result in a change in position of lung lesions, such as granulomas resulting in the so-called shifting granuloma sign ( Fig. 7.3 ). Of particular note, the Luftsichel sign (from German, meaning air crescent) is due to the overinflated superior segment of the ipsilateral lower lobe occupying the space between the mediastinum and the medial aspect of the collapsed upper lobe, resulting in a paramediastinal translucency ( Fig. 7.4 ). The sign is more common on the left than on the right and is regarded as a typical appearance of left upper lobe collapse. CT demonstrates the increased paramediastinal lucency to be due to a wedge shape of the collapsed upper lobe, with the apex of the V resulting from tethering of the major fissure by hilar structures (see Fig. 7.4B ).

Mediastinal shift is another indirect sign of volume loss and the degree varies according to the position of the affected lobe. Usually the least mediastinal shift occurs in right middle lobe collapse, whilst the greatest shift, particularly of the inferior mediastinum, is seen with lower lobe collapse. The amount of mediastinal shift due to upper lobe collapse is often dependent on the chronicity; in acute upper lobe collapse there is often little shift, whereas in chronic upper lobe volume loss with fibrosis, the shift may be greater. The position of the trachea may be a useful indicator of superior mediastinal shift as it should be central in the superior mediastinum between the anterior ends of the clavicles or slightly deviated to the right by the aortic arch. Inferiorly within the mediastinum, anywhere between one-half and one-fifth of the cardiac outline normally lies to the right of the midline and greater or lesser variations indicate mediastinal shift. However, because of the wide variation in normal subjects, displacement of the cardiac outline may be more difficult to assess than changes in position of the trachea.
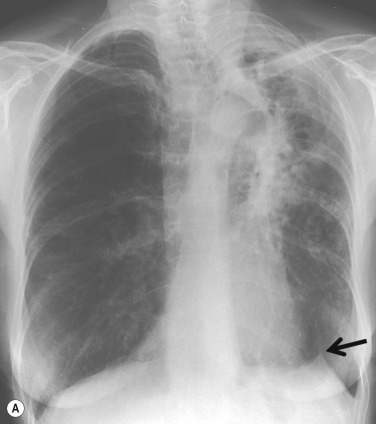
The hemidiaphragms may be elevated in lobar collapse, particularly involving the left upper lobe and to a lesser extent the right upper and both lower lobes. However, the sign is of limited value because the position of the right hemidiaphragm is highly variable (0–3 cm higher than the left on the frontal chest radiograph). A useful ancillary sign of upper lobe collapse (or a combination of right upper and middle lobe collapse) is a juxtaphrenic peak of the diaphragm ( Fig. 7.5A ). The sign refers to a small triangular density at the highest point of the dome of the hemidiaphragm, due to the anterior volume loss of the affected upper lobe, resulting in traction and reorientation of an inferior accessory fissure (see Fig. 7.5B ).
Reduction in the volume of a hemithorax may result in relative reduction of the spaces between the ribs by comparison to the unaffected side. Rib crowding or approximation may be recognisable on the frontal radiograph in cases of chronic lobar collapse, but in acute collapse it may be more difficult to appreciate. Furthermore, the sign is considered to be unreliable as patient rotation and minor degrees of scoliosis may result in apparent rib crowding.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here