Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pulmonary arteriovenous malformations (PAVMs) consist of varyingly sized dilated vascular channels connecting pulmonary arteries and veins directly with no intervening capillary bed. These are generally congenital and usually found in patients with hereditary hemorrhagic telangiectasia (HHT), although the PAVM is also often applied to acquired arteriovenous fistulae. These shunts are frequently asymptomatic but paradoxical embolization and hemorrhagic rupture can produce sudden severe consequences, problems that can be ameliorated with embolotherapy.
Hereditary hemorrhagic telangiectasia is reported in 56%–97% of patients with congenital PAVM, with the real prevalence probably in the higher range. This autosomal dominant heterozygous genetic disorder occurring in 1 in 5000–8000 causes arteriovenous malformations (AVMs) of variable size in multiple organs and is clinically diagnosed in the presence of at least three of four criteria, whereas it is possible with two criteria: (1) multiple telangiectases of the skin and mucous membranes, especially at characteristic sites such as the fingers, lips, oral cavity, and nose (Fig. 54.1 (2) repeated episodes of spontaneous epistaxis (occurring in more than 90%), (3) typical visceral vascular malformations, consisting of PAVM, central nervous system AVM, liver AVM, and gastrointestinal tract telangiectases or larger AVMs, and (4) a family history of HHT in a first-degree relative. Three genetic types of HHT have been identified, with pathogenic variants in ENG (type 1) and ACVRL1 (or ALK1) (type 2) accounting for 73%–93% whereas those in SMAD4 account for 2%–3%. The last gives the combined syndrome of juvenile polyposis-HHT. Given a small false-negative rate, genetic testing is only helpful if positive, except in families with a known mutation, in which case a negative result is conclusive. Given the other organ involvement and familial nature of the disease, patients with HHT are best managed at or in conjunction with an HHT center.

Isolated, sporadic congenital PAVM is uncommon. Acquired pulmonary arteriovenous fistula is most commonly associated with cirrhosis as hepatopulmonary syndrome, in which the lesions are typically microscopic. Other causes are cavopulmonary anastomosis for cyanotic congenital heart disease (which can create macroscopic lesions), schistosomiasis, actinomycosis, hypervascular metastatic cancer (such as choriocarcinoma), amyloidosis, Fanconi syndrome, trauma, or erosion of an aneurysm into a vein.
Evaluation and treatment of PAVM is indicated in all patients having this condition because clinical manifestations can eventually occur in more than 70%. Effects can be related to right-to-left shunting or hemorrhage. The most common serious events are related to paradoxical embolization. Ischemic stroke or transient attack occurs in 11%–55% (possibly contributing to seizures that occur in 5%–15%), which can be silent. Bacterial embolization, with brain abscess, occurs in 5%–25%, and other abscesses in 4%–8%. Larger feeding arteries increase the risk for stroke, whereas a greater number of PAVMs and lower oxygen saturations are two factors that increase the risk for brain abscess. Migraine occurs in 16%–46% and is also likely related to the right-to-left shunt. Bleeding accounts for the next level of serious events, with hemoptysis or hemothorax in 3%–18%. Pregnancy, significant pulmonary hypertension, and diffuse involvement appear to increase the risk for serious complications. Patients often accommodate to hypoxemia, so exertional dyspnea and fatigue are typically minor or absent, except with larger or more extensive disease. Polycythemia is infrequent given coexistent HHT-related bleeding.
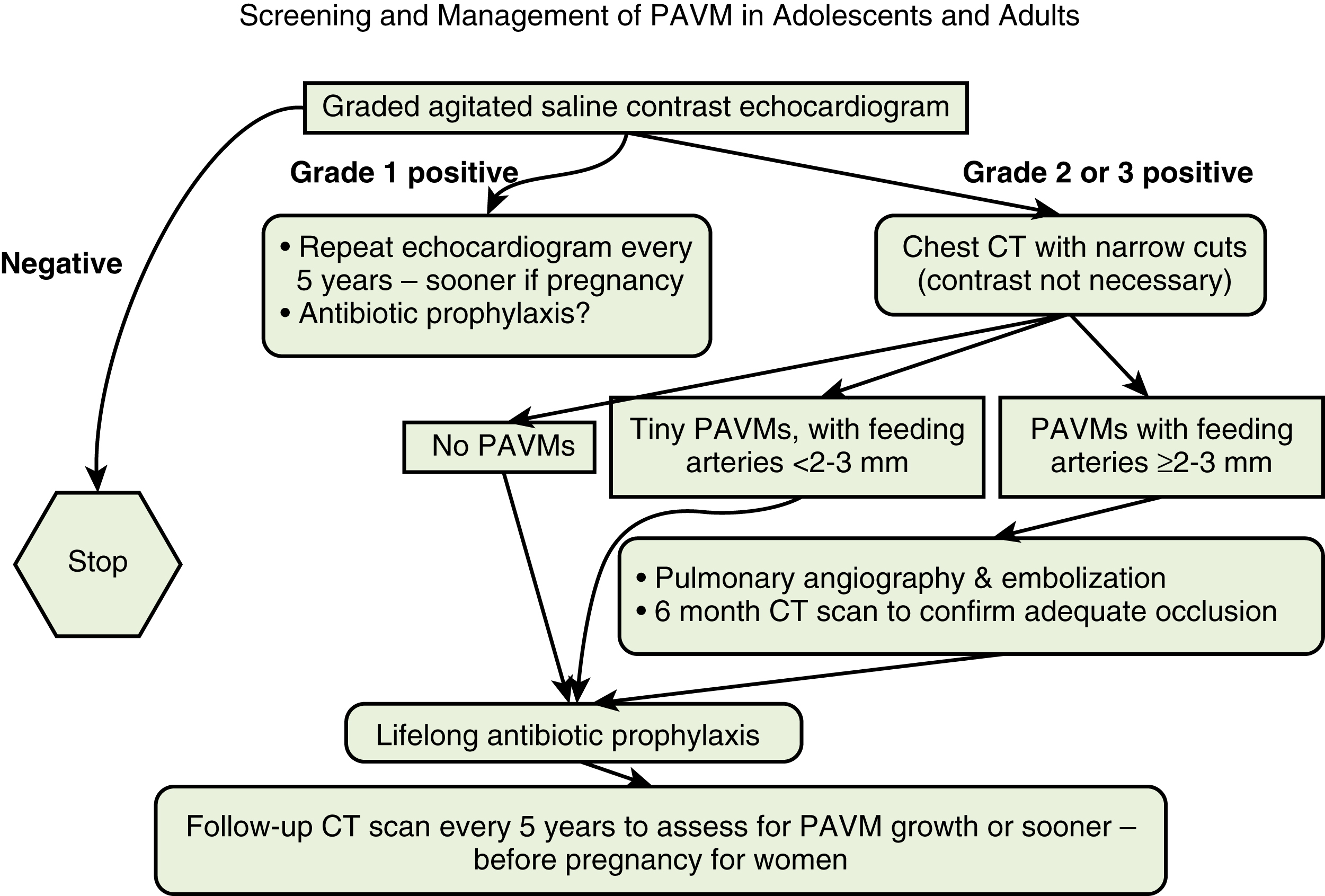
Screening for PAVM is positive in 23%–61% of patients with HHT, greater in those with type 1 than type 2. Agitated saline contrast echocardiography is the best screening study, looking for delayed appearance of left cardiac chamber echogenic microbubbles by 3–10 beats. Information concerning the extent of PAVM that would be found on computed tomography (CT) is gained by quantitating the bubbles. A study with no bubbles nearly excludes PAVM, and CT is not needed. A grade 1 positive study of up to 30 left-chamber bubbles on a single frame means that either no PAVMs or only tiny ones not requiring embolization would be found on CT, so CT is not needed. In fact, up to 28% of the general population can have a grade 1 study, so it is not proof of PAVM. Grade 2 and grade 3 positive studies have 30–100 and more than 100 left-chamber bubbles, respectively, and are proof of PAVM. Chest CT is needed with these higher grades because 25% and 77% would have PAVMs large enough to embolize. At our HHT center, echocardiographic screening starts in mid-adolescence ( Fig. 54.2 ) because children younger than this having no symptoms or signs of PAVM appear safe from having serious events. Children can be screened with periodic pulse oximetry; a value below 97% would raise suspicion although it is probable that spontaneous events do not become of significant risk until the saturation is below 90%–93%.
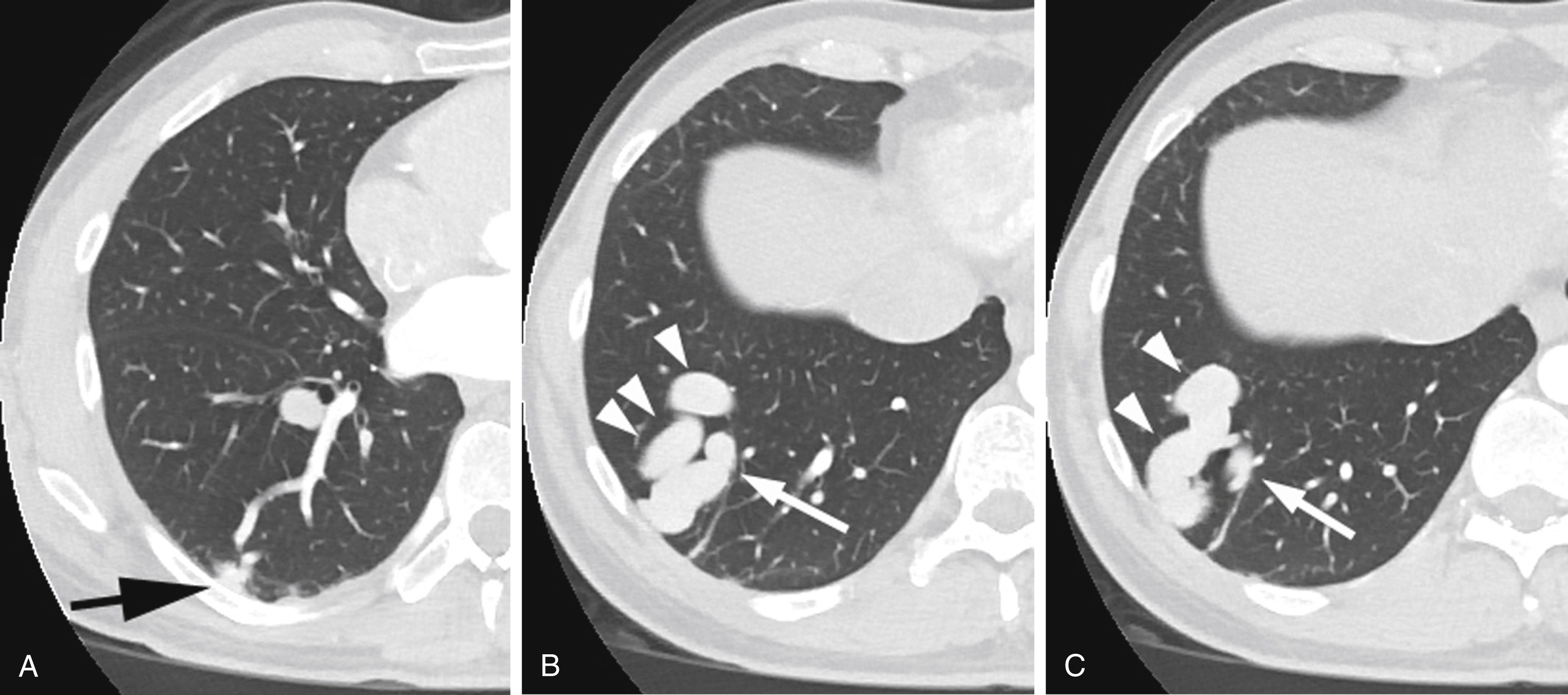
Chest CT accurately depicts the size, type, location, and number of PAVMs. Thin slices without contrast medium suffice, although some prefer CT angiography. Simple PAVMs are 80%–90% of lesions, having their arterial supply within one segment, complex PAVMs are responsible for 10%–20%, having several arteries derived from more than one pulmonary segment, and up to 5% are diffuse. Most commonly seen is a well-defined, lobular soft tissue nodule or serpiginous mass with enlarged connecting vessels, although occasionally a more inhomogeneous connection or nidus is present, especially with complex and diffuse disease ( Fig. 54.3 ). Although delineation of the precise angioarchitecture may require pulmonary angiography, this level of information is typically not necessary in making a decision to embolize. Most centers believe that magnetic resonance imaging or magnetic resonance angiography has not yet achieved a level of accuracy to replace CT.
Embolization is indicated for PAVMs having a feeding artery more than 2–3 mm. Because smaller lesions can still permit paradoxical bacterial embolization, lifelong antibiotic prophylaxis before procedures prone to result in bacteremia is essential, as is care to avoid air or blood clots in intravenous lines; if possible, an air filter is recommended. Of particular concern are any dental procedures. Scuba diving is also contraindicated because of the risk of embolization of decompressive air bubbles. Surgical resection of larger PAVM is rarely indicated but may be considered for intractably reperfused lesions and regionally limited diffuse involvement.
No absolute contraindications exist to PAVM embolization but some issues need to be considered. As noted in the Indications section, children are less likely to suffer adverse consequences unless they are significantly hypoxemic. In addition, embolization in this growing population may have a higher risk for collateral reperfusion, which is more difficult to treat, and exposure to ionizing radiation is clearly concerning. Therefore, every effort should be made to delay treatment to their midteens. Pregnant women are also of concern for radiation exposure, but are also at higher risk for PAVM complications; treatment can be performed during the second trimester.
Pulmonary hypertension is more common in patients with HHT, both primary and secondary to elevated flow from liver AVM, and might be worsened by occlusion of a low-pressure shunt. However, the effects of embolization are uncertain and embolization likely can be safely performed.
Diffuse PAVM is difficult to manage, with embolization often having little effect on oxygen saturation. Such treatment is typically reserved for focally larger shunts that would permit larger paradoxical emboli.
Patients with a history of serious contrast reaction can still be treated using premedication and possibly general anesthesia.
7Fr or 8Fr introducer sheath for venous access.
5Fr pigtail catheter for pulmonary angiography.
Guide catheter through which 5Fr or 6Fr catheters can be placed. The 7Fr or 8Fr White LuMax guiding catheter systems (Cook Medical, Bloomington, IN) have been designed for selective pulmonary catheterization and consist of an outer 80-cm 7Fr or 8Fr multipurpose guide catheter and inner 100-cm 5Fr or 6Fr short-angled catheter.
Variously shaped 5Fr catheters, 100–125 cm long that can be placed through the larger guide catheter as needed to enhance selection. A Judkins left coronary catheter (Cordis Corp., Miami Lakes, FL) is particularly useful for initially selecting lingula arteries, and then exchanged for the forward-angled catheter for more distal catheterization.
Microcatheters may rarely be needed to reach more distally when 5Fr catheters cannot be advanced sufficiently.
Mechanical embolization agents. Commonly used ones are pushable coils, detachable coils, Amplatzer Vascular Plugs, versions I, II, and IV (St. Jude Medical, Abbott, St. Paul, MN), and Micro Vascular Plugs (Covidien, Medtronic, Minneapolis, MN).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here