Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Safe and effective respiratory support of newborn infants requires a good understanding of pulmonary physiology, familiarity with the available evidence regarding management of respiratory failure and knowledge of the capabilities of the ventilators at one’s disposal. The clinician must also recognize that individualized patient care is the best approach, and that requires frequent assessment of the patient’s response to treatment and regular assessment of all available information, including physical examination, assessment of patient–ventilator interaction and observation of the ventilator waveforms. Blood gas analysis and chest radiographs complete the picture but are not sufficient by themselves to provide full assessment of the adequacy of respiratory support.
Neonatal respiratory support has improved substantially over the past few decades and with the increased use of antenatal steroids and less invasive surfactant administration, many very premature babies can be successfully treated with noninvasive respiratory support. However, although mechanical ventilation has greatly reduced mortality from pulmonary causes, serious morbidity, including bronchopulmonary dysplasia (BPD) remains high. With increased use of antenatal steroids and improved delivery room stabilization, most moderately preterm and many very preterm infants can be supported noninvasively, thus avoiding ventilator-associated lung injury (VALI). Invasive ventilation is largely reserved for the relatively small number of the most immature or very sick term infants, resulting in less experience for trainees and practitioners. These more immature patients may be uniquely susceptible to lung injury because of the very early stages of lung development at which they are born, making it that much more critical to employ ventilation strategies that minimize VALI. However, some degree of lung injury is probably inevitable in mechanically ventilated extremely preterm infants even with optimal respiratory support.
Sophisticated microprocessor-based ventilators with advanced features enabling effective synchronized ventilation are now widely available. However, better technology can only improve outcomes if used with care and with optimal ventilation strategies that are appropriate for the specific condition being treated. A good understanding of the many unique aspects of a newborn infant’s respiratory physiology will help the clinician use the sophisticated tools at his/her disposal to best advantage.
Small infants with poorly compliant (stiff) lungs have very short time constants (a measure of how rapidly gas moves in and out of the lungs) and thus rapid respiratory rates with very short inspiratory times. Their limited muscle strength and a ribcage that lacks sufficient rigidity make it difficult to maintain adequate end-expiratory lung volume and tidal volume. Use of adequate end-expiratory pressure and ventilator design that allow the baby to trigger ventilator inflation with minimal inspiratory effort and minimal trigger delay are essential.
Neonates are generally ventilated using uncuffed endotracheal tubes (ETT) because of a concern about injury to the tracheal mucosa; therefore, some degree of gas leak around the ETT is present in most infants. The small size of the tubes also makes inflatable cuffs difficult to incorporate without compromising lumen size. However, large ETT leak makes tidal volume estimation increasingly inaccurate, making volume targeted ventilation more challenging. The ETT leak increases with time if prolonged ventilation is required, because the larynx and trachea are progressively dilated by the cyclic stretch of many thousands of positive pressure inflations per day. The leak varies from moment to moment because the ETT is inserted only a short distance beyond the larynx; thus the leak will change with any change in the infant’s head position and movement of the ETT up and down in the trachea.
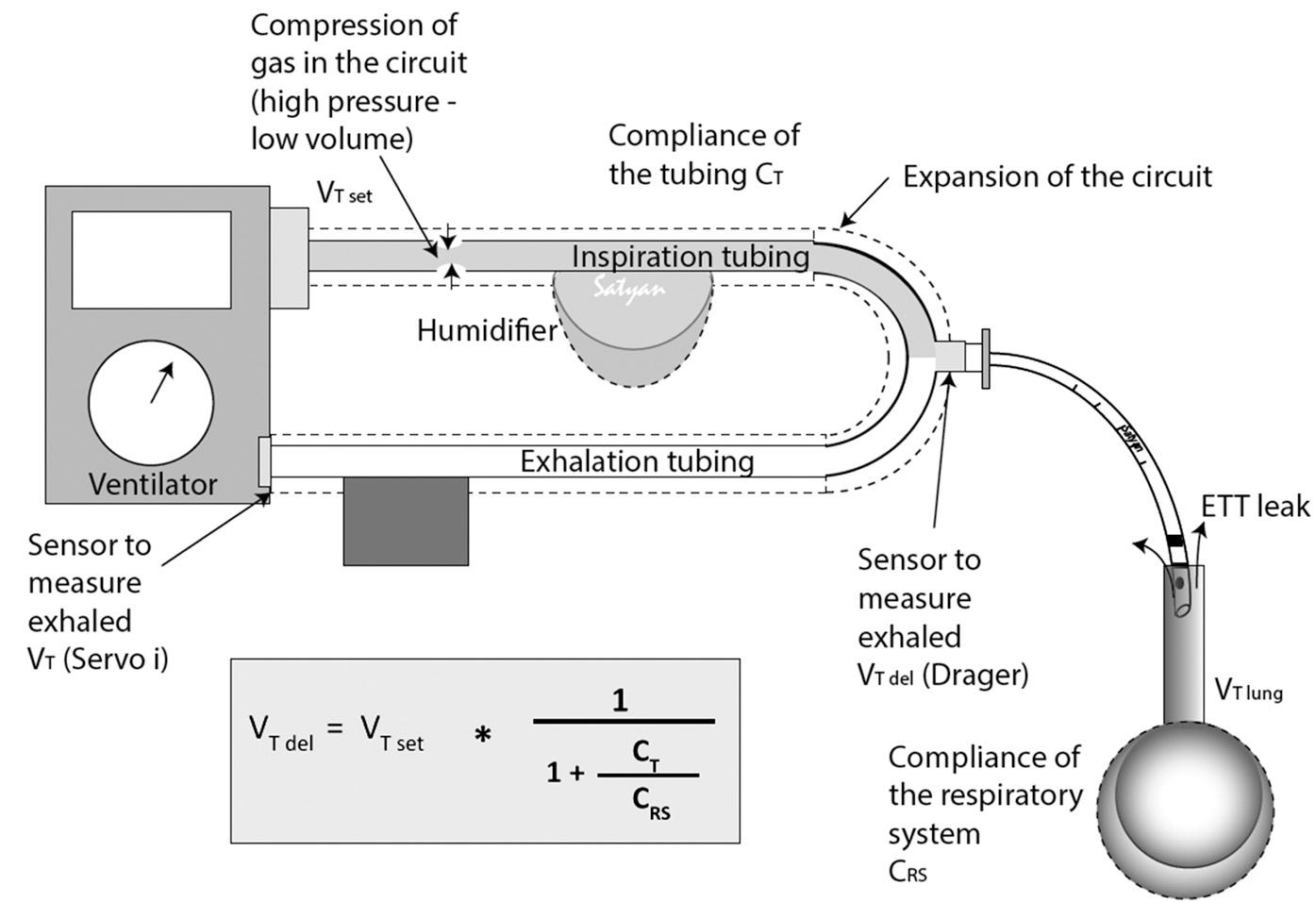
The importance of accurate tidal volume (V T ) measurement in extremely small infants is obvious, considering that these infants are ventilated with a tidal volume in the range of 2 to 5 mL. Some ventilators not specifically designed for newborn infants measure flow and calculate V T at the ventilator end of the patient circuit rather than at the airway opening. This remote placement avoids extra wires and the added instrumental dead space of a flow sensor at the airway opening but results in large overestimation of the true V T , because of compression of gas in the circuit, distention of the circuit, and leak around the ETT. The loss of tidal volume in the circuit is proportional to the compliance of the ventilator circuit and humidifier (and the compressibility of the volume of gas they contain), relative to the compliance of the patient’s lungs ( Fig. 10.1 ). In large patients with a cuffed ETT, the volume measured at the ventilator correlates reasonably well (using appropriate corrections) with the actual V T entering the lungs. In tiny infants whose lungs are very small and thus relatively noncompliant, the loss of volume to the circuit is proportionally much larger and not easily corrected, especially in the presence of significant ETT leak.
The purpose of mechanical ventilation is to maintain acceptable gas exchange with a minimum of adverse effects. These include lung injury, air-leak syndrome, hemodynamic impairment, nosocomial infection, and brain injury. Secondary objectives are achieving adequate lung aeration, reducing exposure to high oxygen concentrations, and reducing the work of breathing. Indications for mechanical ventilation include absent or inadequate respiratory effort and signs of impending respiratory failure, such as frequent apnea, high and rising P co 2 level, persistent high oxygen requirement (Fi o 2 >0.40–0.50), and excessive work of breathing despite optimized noninvasive support. Because there is a clear association between the length of ventilator support and development of chronic lung disease, ventilator support should be weaned as rapidly as possible, and the infant should be extubated to some form of noninvasive support at the earliest opportunity.
The choice of ventilator modes may be limited by the equipment available in the neonatal intensive care unit (NICU). Most modern ventilators are capable of providing the basic modes of synchronized ventilation, which include synchronized intermittent mandatory ventilation (SIMV), assist-control ventilation (AC), and pressure support ventilation (PSV) but may also include hybrid or dual-control modes. Not all widely used devices and modes are optimal for small preterm infants. Ventilators that are designed primarily for adult/pediatric patients but are capable of also supporting neonates (so-called universal ventilators) have a variety of modes, some of which have never been evaluated in newborn infants and thus should be avoided.
As described earlier, the volume-controlled ventilation mode that is available on these devices controls the volume delivered into the proximal (ventilator) end of the circuit (known as V set ), not the tidal volume entering the patient’s lungs (V deliv ) and thus overestimates the true tidal volume, especially when a large leak around the ETT is present. For these reasons, pressure-controlled ventilation (commonly referred to as time-cycled, pressure-limited ventilation in the neonatal literature) became the standard ventilation mode in the NICU. More recently, modifications of pressure-controlled ventilation that provide volume targeting have become available. These modalities, collectively known as volume-targeted ventilation, make it possible to combine the advantages of pressure-controlled ventilation and relatively stable delivered tidal volume ( ).
You are attending the delivery of a 700 g, female infant born at 25 weeks’ gestation after rapid preterm labor with no time for antenatal steroids. The infant has a good heart rate but minimal respiratory effort, and despite stimulation and application of CPAP with a few positive pressure inflations via the T-piece resuscitator (using a peak inflation pressure [PIP] of 25 cm H 2 O to achieve minimal chest rise), her color remains poor and her spontaneous respiratory effort is inadequate. You decide to intubate and initiate mechanical ventilation. You remember that your transport ventilator is only capable of basic pressure-controlled ventilation without patient triggering, known as intermittent mandatory ventilation (IMV).
What would be your initial ventilator settings?
PIP 25 cmH 2 O, positive end-expiratory pressure (PEEP) 6 cmH 2 O, rate 50/minute, inflation time (Ti) 0.3 seconds, fraction of inspired oxygen concentration (Fi o 2 ) adjusted to maintain a saturation of 90% to 95%
PIP 15 cmH 2 O, PEEP 6 cmH 2 O, rate 25/minute, Ti 0.3 s, Fi o 2 (to maintain a saturation of 90%–95%)
PIP 25 cmH 2 O, PEEP 3 cmH 2 O rate 50, Ti 0.3 s, Fi o 2 (to maintain a saturation of 90%–95%)
PIP 25 cmH 2 O, PEEP 6 cmH 2 O, rate 50/minute, Ti 0.5 s, Fi o 2 (to maintain a saturation of 90%–95%)
Choice A. Here, as always, you need to consider the disease process, the size of the infant, and the infant’s general condition. Because there is little respiratory effort, you must provide essentially all of the baby’s respiratory support. Therefore you should choose a respiratory rate that is appropriate for the tiny infant in front of you, namely 50 to 60 breaths/minute. Because you just used the T-piece resuscitator, select a PIP that is adequate to get a minimal chest rise. The basic functionality of a conventional mechanical ventilator is much like that of the T-piece resuscitator ( Fig. 10.2 ).
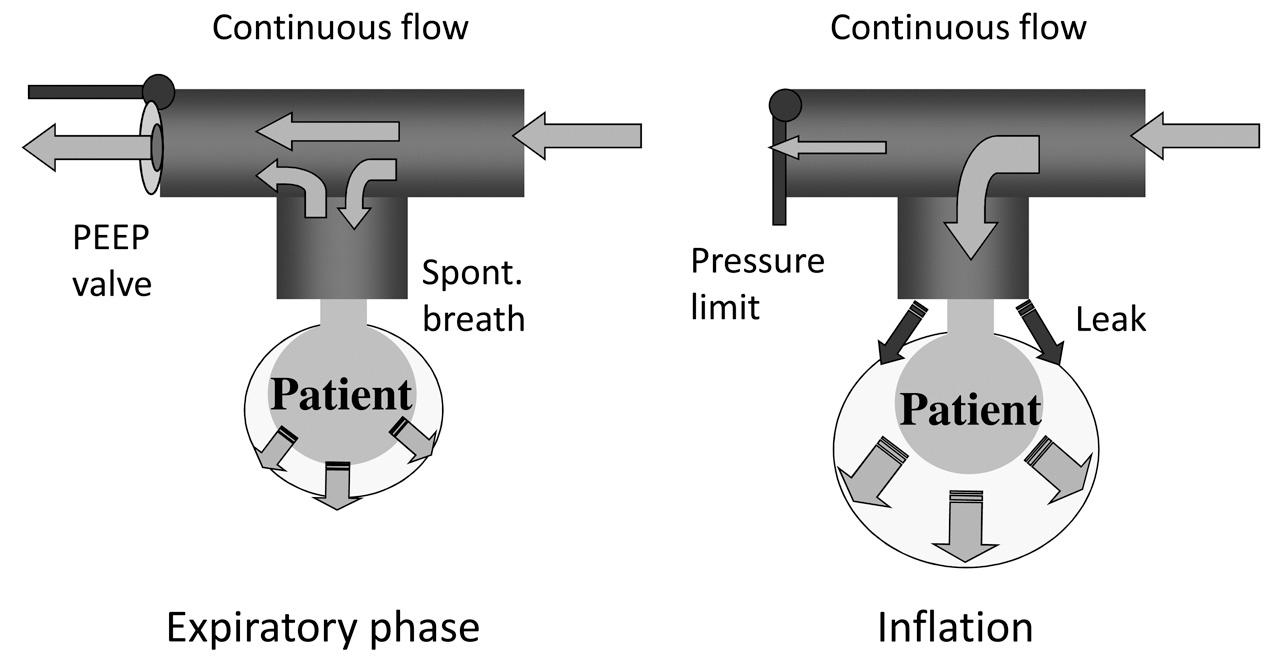
Although your PIP was 25 cmH 2 O using the T-piece resuscitator, it is a relatively high pressure, which indicates the infant has not yet achieved adequate lung aeration nor cleared lung fluid from her lungs. You now need to select an inspiratory time (Ti) and positive end-expiratory pressure (PEEP). Appropriate inspiratory time depends on the time constants of the respiratory system of your patient. Time constant is a measure of how rapidly gas moves in and out of the baby’s lungs and reflects lung mechanics, as well as patient size. In simple terms, tiny babies with low lung compliance and normal airway resistance (i.e., your patient) have very short time constants, so you would choose a Ti of about 0.3 s. Large infants with high airway resistance would need a longer Ti. Adequacy of inspiratory and expiratory time is best verified by examining the flow waveform on the ventilator display, as discussed later in this chapter. PEEP is critical in achieving and maintaining adequate lung inflation. Achieving an “open lung”—that is a lung that is optimally inflated with good ventilation–perfusion matching and even distribution of tidal volume—is a key element in lung-protective ventilation strategies and should be guided by the infant’s oxygen requirement. A high Fi o 2 usually indicates inadequate lung volume recruitment that results in ventilation–perfusion mismatch. Your goal is to get the Fi o 2 below 0.30, so you should select a PEEP of 6 cmH 2 O and increase in increments of 1 cmH 2 O to a maximum of 8 cmH 2 O if high oxygen requirement persists.
You and your patient arrive safely in the NICU. The mode of ventilation is changed to SIMV using the prior settings but a lower rate, because the infant is now starting to breathe. Settings are: PIP of 25 cmH 2 O, PEEP of 7 cmH 2 O, rate 45/min, Ti 0.3 s, and Fi o 2 of 0.32. Your respiratory therapist administers surfactant via endotracheal tube while you are preparing to place umbilical arterial and venous catheters. When you finally get appropriate line placement an hour later and obtain a blood gas, you are pleased to see that the PaO 2 is 655 mm Hg but dismayed that the P co 2 is 28 mm Hg with a pH of 7.47. You recall that hypocapnia and alkalosis increase the risk of periventricular leukomalacia and severe intraventricular hemorrhage in very in preterm infants.
Why did the hypocapnia develop?
Remember that with pressure-controlled ventilation, the amount of gas that enters the lungs (V T ) is determined by the inflation pressure (PIP−PEEP) and the compliance of the respiratory system. Compliance is a measure of how much volume (in mL) enters the lungs for any given change in airway pressure (Compliance = ΔV/ΔP). For example, if a pressure of 15/5 (PIP/PEEP, cmH 2 O) produces a tidal volume of 5 mL, the compliance is 5/(15−5) = 0.5 mL/cmH 2 O. At least three factors combined to improve lung compliance, which in turn increased the tidal volume with a fixed inflation pressure of 25 cmH 2 O. First, PEEP was appropriately increased to optimize lung inflation. Lung compliance improves when lung volume is optimized, so it was predictable that V T would improve and thus P co 2 would drop. Second, currently available surfactants rapidly improve lung aeration and lung compliance (increasing the tidal volume). Finally, with adequate respiratory support and passage of time, residual lung fluid should have cleared, also improving compliance and gas exchange.
What could you have done differently to avoid the hypercapnia?
There are two things that would have prevented this problem. When using pressure-controlled ventilation, the measured tidal volume needs to be monitored closely—this is more accurate than relying on visual assessment of chest rise or auscultating breath sounds—and adjustments to inflation pressures need to be made as often as necessary to avoid inadvertent overventilation when changes in lung compliance are occurring. The period soon after initiation of mechanical ventilation is a time of rapid change, and the clinical team may be distracted by procedures, admission documentation, etc., making close clinical observation challenging. A better alternative is to use a volume-targeted mode of ventilation that responds automatically and in real time to changes in lung compliance and patient respiratory effort and thus maintains relatively stable tidal volume.
You do not feel sufficiently comfortable with volume-targeted ventilation, so you chose to manually adjust PIP. Over the next few hours you lower the PIP to 18 cmH 2 O with a gradual rise of the P co 2 to 38 mm Hg. It is important to avoid rapid changes in minute ventilation and P co 2 , because such changes increase the risk of intracranial hemorrhage in extremely preterm infants with a vulnerable cerebral circulation. ( )
Following surfactant administration, the Fi o 2 decreases to 0.24, and the infant appears comfortable on the current ventilator settings. The infant is making adequate spontaneous respiratory effort, so you continue to lower the ventilator rate progressively to 18/min over the next 2 days. Although the P co 2 remains adequate in the mid to high 40s, the nurse complains that the baby has become more tachypneic, and the oxygen requirement is creeping back up to 0.35.
What is the cause of the tachypnea and rising oxygen requirement?
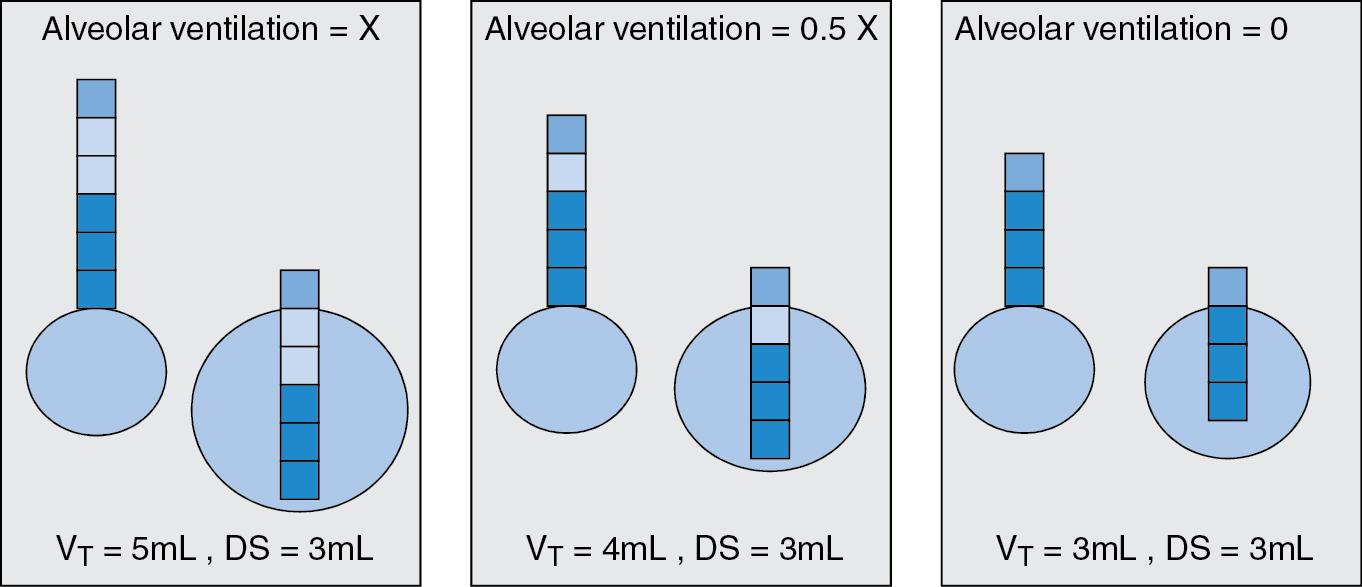
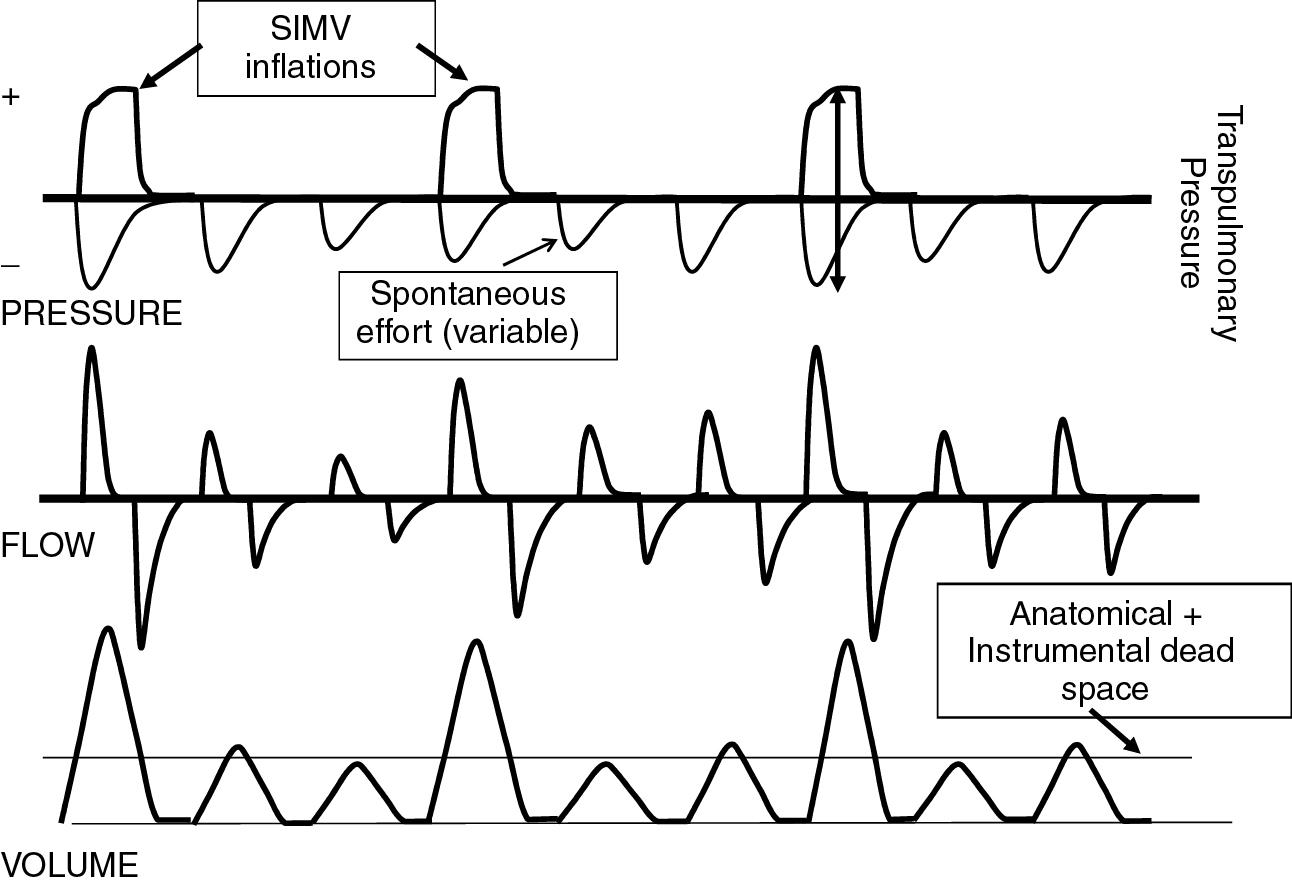
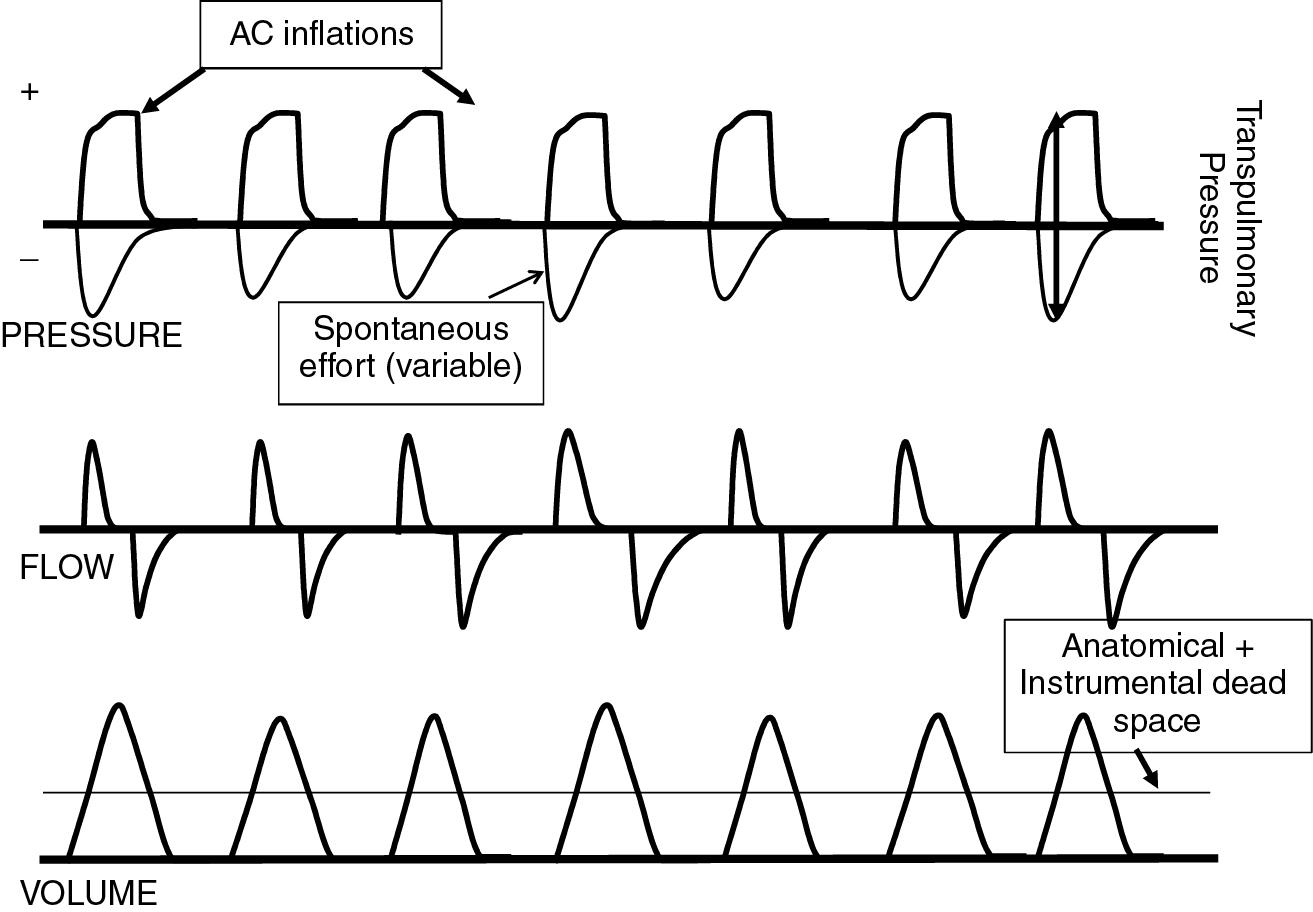
More than one explanation is possible in this scenario, but tachypnea in a mechanically ventilated infant suggests that the ventilator support is inadequate. Careful observation of the infant and the ventilator display will reveal important clues as to the cause. Blood gas measurement and chest radiograph may be helpful but will not provide the whole story. In this case, the most likely explanation is the limited muscle strength of the extremely premature infant, coupled with the high airway resistance of the small endotracheal tube. Remember that SIMV provides positive pressure inflations in synchrony with the patient’s effort only at the rate that you set. Spontaneous breaths in excess of that rate are not supported. Your suspicion is confirmed by noting that the infant’s respiratory rate is 70 to 90 breaths/minute with mild to moderate retractions and periodic pauses. You also notice that the tidal volume display is fluctuating between 3 and 6mL/kg with spontaneous breaths and mechanical inflations, respectively. The 3 mL tidal volume the infant is able to generate on her own barely clears the dead space of the upper airway, endotracheal tube, and flow sensor. Thus it contributes little to alveolar minute ventilation, the portion of the total ventilation that actually reaches the alveoli and participates in gas exchange ( Fig. 10.3 ). To maintain adequate ventilation, relatively large mechanical inflations of around 6 mL/kg are needed. As ventilator rate is decreased, the infant must increasingly rely on her spontaneous effort, but she can only muster this inefficient rapid, shallow breathing ( Fig. 10.4 ). Her high work of breathing increases oxygen consumption and may lead to fatigue, thus impairing extubation efforts. For these reasons, SIMV is not an optimal mode of ventilation for these tiny infants.
What would you do to overcome this problem?
Leaving high-frequency ventilation aside for the moment, you have the option of staying with SIMV and adding pressure support (PS) to her spontaneous breaths or to change to a synchronized mode that supports every spontaneous breath, such as assist control (AC) or pressure support ventilation (PSV). Adding PS to boost the infant’s spontaneous effort to achieve an adequate tidal volume will help the situation, but you now have to decide how much pressure boost to provide and subsequently you will need to figure out which of the two different ventilation patterns to adjust.
The first question is relatively easy to answer. You would typically start with a low value of, say 6 cmH 2 O above PEEP, and see what V T you now achieve with the supported spontaneous breaths and how comfortable (or not) the infant is. You should target a physiologic V T of about 4 mL/kg; the infant should be breathing comfortably with a rate of less than 65/min. There are no established rules for how to gradually withdraw ventilator support in an infant receiving SIMV+PS, but one reasonable way is to continue to wean the SIMV rate and maintain PS at a pressure sufficient to maintain an adequate V T with spontaneous breaths. Once the SIMV rate is down to 10 to 15/minute, and PSV pressure is not more than 6 cmH 2 O with an Fi o 2 less than or equal to 0.30, extubation to noninvasive ventilation is usually possible.
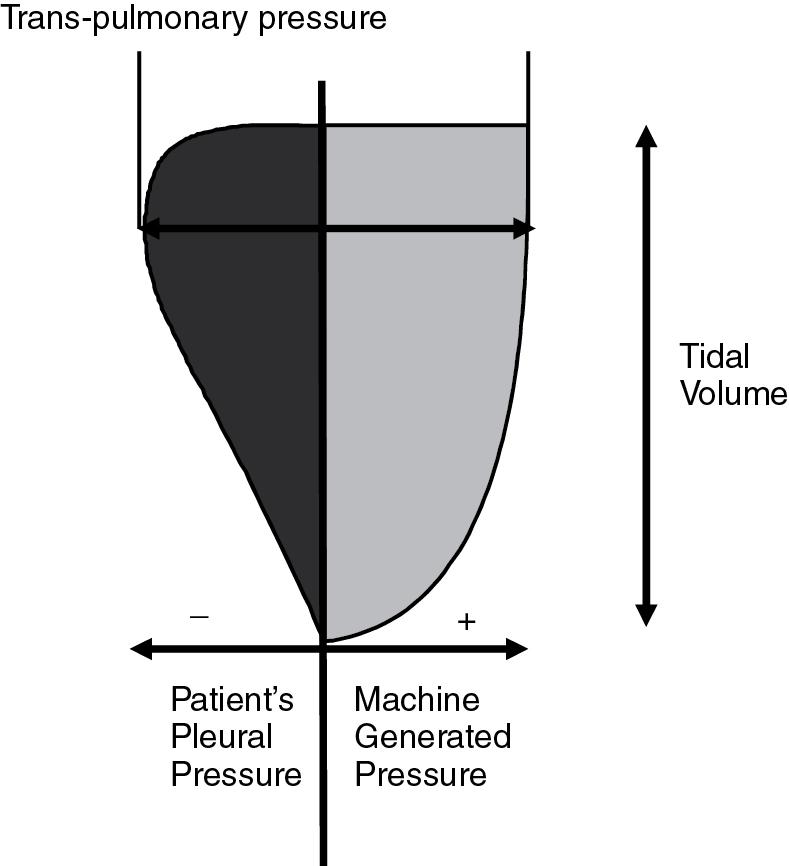
Assist control supports every spontaneous breath of the infant, thus achieving adequate and more consistent V T ( Fig. 10.5 ). The ventilator rate is driven by the infant’s respiratory effort and therefore the ventilator will cycle at the infant’s breathing rate—this is the “assist” part. If the infant fails to breathe, the ventilator will take over immediately at the set backup rate, typically 40 per minute (the “control” part). The backup rate should be just below the infant’s spontaneous breathing rate; think of it as a safety net. In a small infant who is triggering the ventilator at a rate of 60/min when breathing actively, a backup rate of 25 or 30/minute would be too low and result in a large drop in minute ventilation and rise in Pa co 2 , which is potentially dangerous. The tidal volume needed with AC is substantially lower than with SIMV, usually around 4 to 5 mL/kg, because every breath is supported and easily clears dead space. It is important to understand that the tidal volume entering the lungs results from the combined inspiratory effort of the infant (when present) and the positive inflation pressure delivered by the ventilator ( Fig. 10.6 ). Inspiratory time, PIP, and PEEP are set in a similar fashion to SIMV. Weaning is accomplished by lowering PIP, leaving the rate unchanged, because it is only a safety backup. This way, the work of breathing is gradually transferred from the ventilator to the infant.
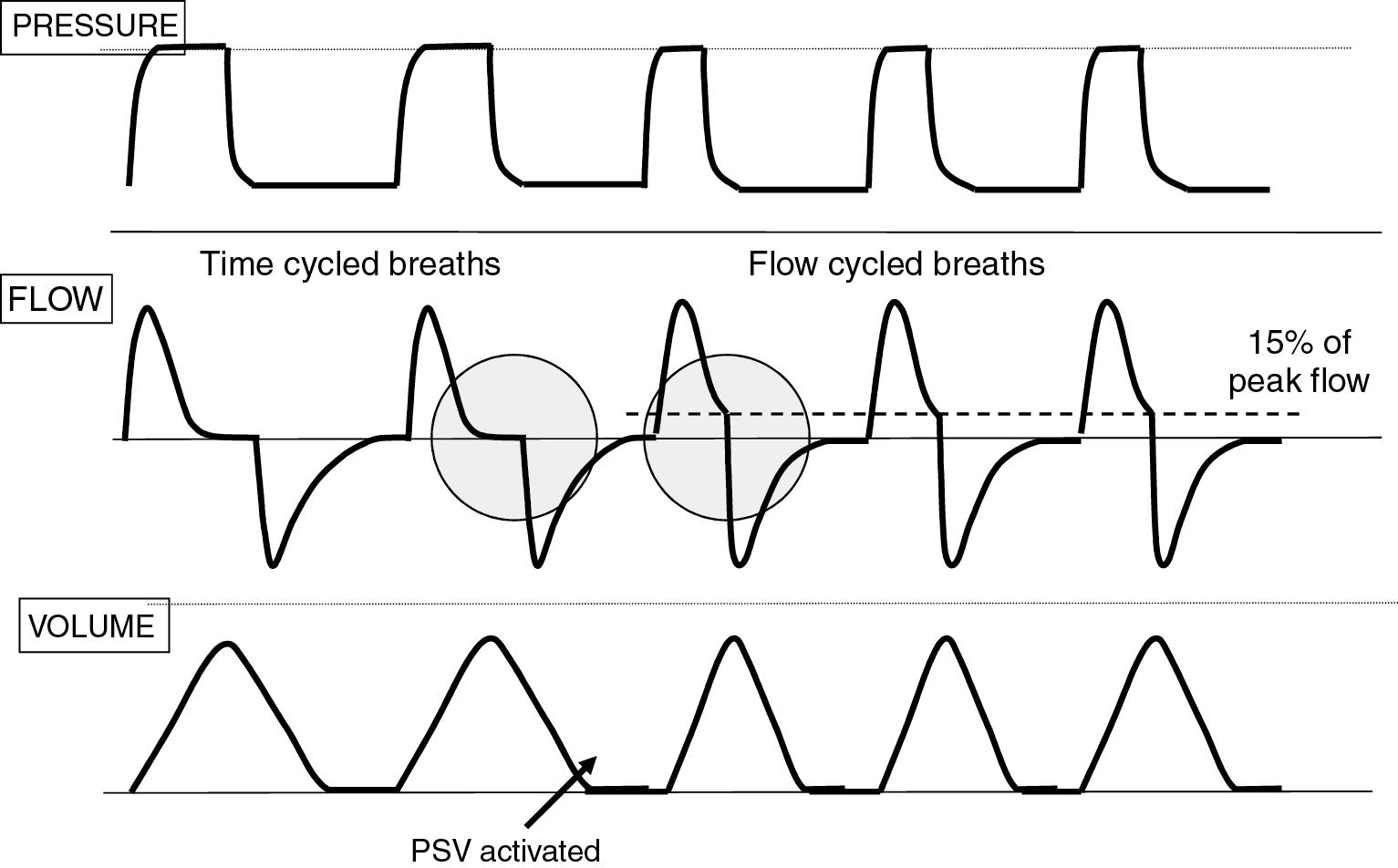
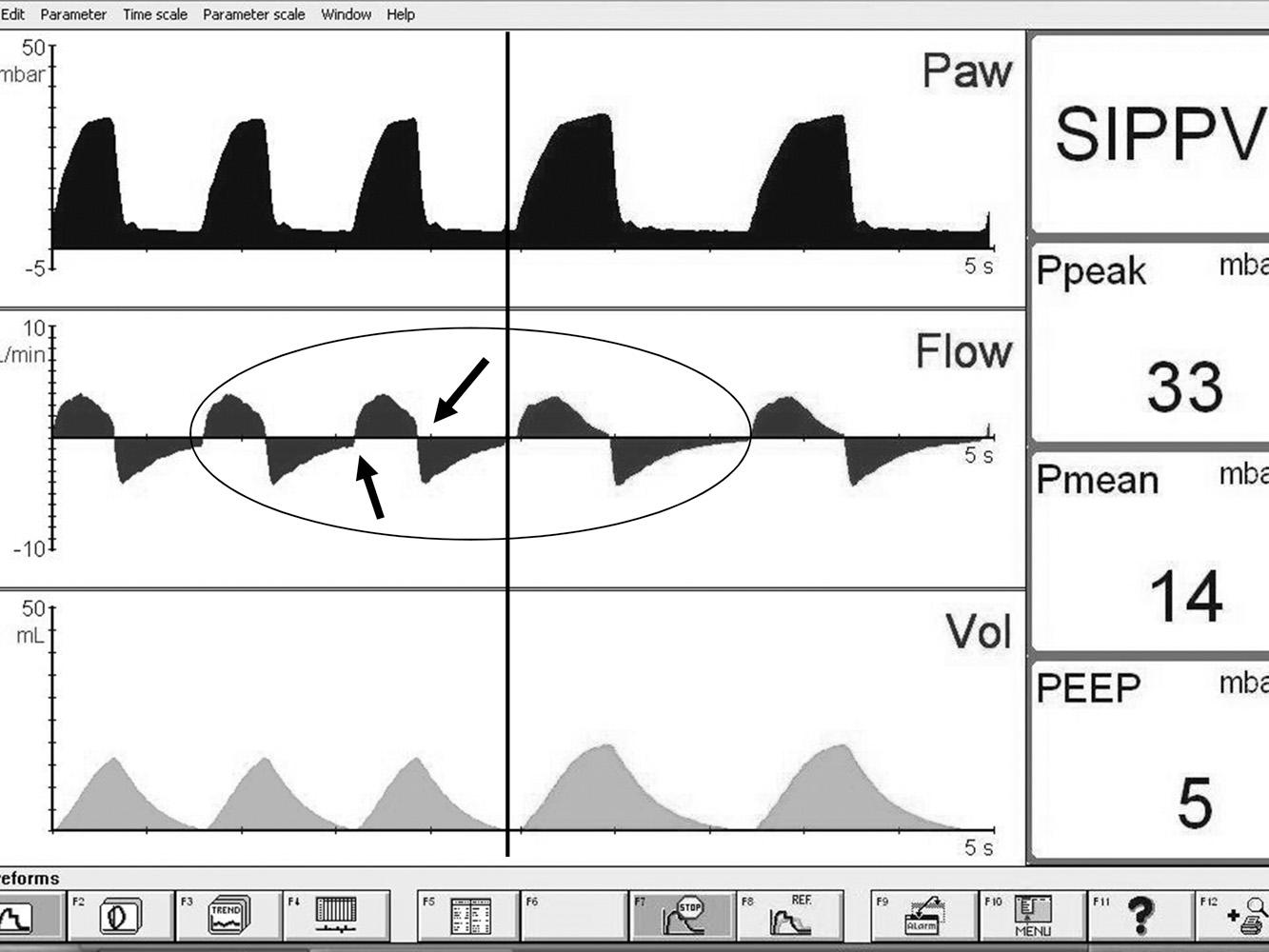
Pressure support ventilation (PSV), when used as a stand-alone mode on specialty neonatal ventilators, is identical to AC, except that the ventilator inflation is flow cycled rather than time cycled. This means that, rather than having a fixed inspiratory time, the ventilator cycles off when inspiratory flow declines to a set percentage of peak flow, typically about 15% ( Fig. 10.7 ). This method eliminates the inspiratory hold and makes for more complete synchrony. The infant now has control over both onset and termination of ventilator inflation and the inspiratory time is automatically adjusted in response to changing lung mechanics. Ventilator settings and weaning are similar to AC. Because the Ti is usually shorter than with AC, PSV typically results in a lower mean airway pressure, which could lead to atelectasis if PEEP is not adjusted to maintain the same mean airway pressure. Table 10.1 summarizes key features of the basic modes of synchronized mechanical ventilation.
| Patient Triggering | Advantages | Drawbacks | |
|---|---|---|---|
| IMV | None | Asynchrony | |
| SIMV | Set rate is patient triggered and time cycled, additional breaths are not supported. Clinician controls ventilator rate. | Simplicity, less affected by auto-triggering | High work of breathing, uneven V T , rapid shallow breathing |
| SIMV + PS | Set rate is patient triggered and time cycled. Additional breaths are patient triggered, supported with a pressure above PEEP, and time cycled. | Reduces work of breathing, provides more adequate support, faster weaning than SIMV | Complicated, results in two different types of ventilator inflations More complicated weaning |
| AC | Every spontaneous breath is supported and time cycled. Patient controls ventilator rate. | More adequate support, smaller V T , faster weaning than SIMV | Potentially affected by auto-triggering with some ventilators |
| PSV | Every spontaneous breath is supported and flow cycled. Patient controls ventilator rate. | As AC, plus more complete synchrony | Ti may be too short when time constants are very short. Shorter Ti leads to lower mean airway pressure and thus needs increased PEEP. |
You admit a 1-hour-old, 4200 g infant who was born through thick meconium by emergency cesarean delivery. The infant required intubation in the delivery room because of poor respiratory effort and inadequate response to positive-pressure ventilation by mask. Thick meconium was noted in the trachea upon intubation. You initiate ventilation with SIMV, PIP of 24 cmH 2 O, Ti of 0.5 s, and PEEP of 6 cmH 2 O. Because the infant has no spontaneous respiratory effort, you set the ventilator rate at 50/min and titrate the Fi o 2 to maintain adequate oxygen saturation. The chest radiograph shows typical appearance of MAS with patchy infiltrates and mild degree of air trapping. An arterial blood gas (ABgG) reveals a pH of 7.24, P co 2 of 52 mm Hg, P o 2 of 67 mm Hg, and BE−8. You check the ventilator display (kudos for doing that) and notice that the tidal volume (V T ) is 4.5 mL/kg, which seems reasonable to you. You also realize that to generate a larger V T , you would need to raise the PIP. You are reluctant to go higher than the current value, so you choose instead to increase the ventilator rate to 60/min, hoping to bring down the P co 2 . You are dismayed to see that the repeat ABG shows the P co 2 has risen to 61 mm Hg with a pH of 7.19. A repeat chest radiograph shows even more prominent air trapping. You therefore decide that the problem must be excessive PEEP and accordingly lower the PEEP to 4 cmH 2 O. Disappointingly, neither the chest x-ray nor the blood gas improves.
Why is the P co 2 continuing to rise?
This infant’s condition (MAS) is well known to result in increased alveolar dead space due to air trapping and heterogeneous lung inflation. Published evidence indicates a need for a tidal volume of about 6 mL/kg to achieve adequate alveolar minute ventilation ( ). Therefore the initial respiratory acidosis was predictable.
The problem with increasing the rate, rather than PIP (to increase V T ) is twofold. First, when the V T is mostly ventilating dead space, increasing the rate has relatively little impact on alveolar minute ventilation. Second, this is a large baby with high airway resistance, which leads to longer time constants. Time constants are a measure of how rapidly gas gets in and out of the lungs. Larger lungs require more time to fill and empty; high airway resistance and better compliance also increase time constants, which mathematically are the product of airway resistance and absolute lung compliance. Thus the higher rate resulted in insufficient expiratory time and worsening air trapping, leading to further CO 2 retention ( Fig. 10.8 , left panel). Lowering the set PEEP does not have much impact, because the problem is dynamic PEEP caused by incomplete exhalation.
Unfortunately, you have not yet figured this out. The bedside nurse points out that the baby has become quite active and is now “fighting the ventilator.” You decide that this is probably the reason for the poor gas exchange and order a dose of fentanyl to stop the baby from interfering with your ventilator support. Alas, though the baby is now quiet and the nurse is happy, the blood gas has deteriorated even more.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here