Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
|
|
|
|
Primary bone tumors of the cervical spine remain relatively rare but potentially devastating conditions. Most cervical spine tumors are the result of metastatic spread from remote sites. Fortunately, most primary cervical spine bone tumors are benign. However, given the possibility of cortical disruption and local tumor growth into surrounding vital structures, even benign tumors can be problematic. Primary malignant tumors of the cervical spine are very rare but have a poor prognosis because most of these tumors cannot be excised with wide margins.
For most patients with primary cervical spine tumors, the presenting symptom is localized pain. The pain is typically of insidious onset and is located in the posterior neck or occipital area. Neurologic findings are less common on initial presentation because of the slow progression of many of these tumors. Pain can be the result of cortical expansion, microfracture of the trabeculae, gross pathologic fracture, or compression of the spinal cord or exiting nerve roots. Motor weakness in a specific nerve root distribution can occur with nerve root compression, whereas generalized weakness can occur with epidural compression of the spinal cord. Bowel and bladder dysfunction and signs of myelopathy are rare findings, but they can manifest in later stages with more severe spinal cord compression.
Following the appropriate patient evaluation including medical history, physical examination, imaging, and laboratory studies, the surgeon must often obtain a tissue biopsy to confirm the suspected diagnosis. The biopsy technique should allow for collection of adequate tissue for diagnosis while avoiding contamination of the surrounding tissues. Unfortunately, this crucial portion of the process is frequently not given sufficient consideration or is performed inappropriately. The location of the biopsy specimen should be determined on the basis of imaging studies. The specimen should be taken from the most accessible location, with the fewest risks to adjacent structures, and the entire biopsy tract should be maintained in line with the planned surgical excision so it can be removed en bloc with the tumor if necessary. The biopsy should be performed at the medical center responsible for the definitive treatment to reduce the risks of the following: contamination of the surrounding tissues; inadequate sample size; inexperience of the pathology staff in bone tumors, which can lead to a delay in diagnosis; tumor recurrence; and the need for more extensive surgical procedures.
These tumors present a significant challenge to the treating clinician. Consultation with appropriate specialists including internal medicine and medical and radiation oncology is necessary to provide the patient with the best treatment plan. An understanding of the natural history of the condition, along with the risks and benefits of complementary treatment options including chemotherapy and radiation therapy, is essential. This chapter introduces the diagnosis and treatment of primary cervical spine tumors. Specific benign and malignant tumors are discussed individually.
An aneurysmal bone cyst is a nonneoplastic lesion that can be aggressive and expansile. Its origin remains uncertain, and it can occur as a solitary lesion or in combination with other tumors, including giant cell tumor, chondroblastoma, chondromyxoid fibroma, and fibrous dysplasia. It is most commonly found in children, with a peak incidence in the second decade of life. A slight female predominance is seen. The most common locations are the spinal column and the long bones.
Of those cysts that affect the spine, 70% are located in the thoracolumbar spine, with only 25% in the cervical spine. They are often found in the posterior elements including the lamina, spinous process, and pedicles. Patients often present with vague complaints of pain, stiffness, and swelling. The slow growth of the lesion and the vague initial symptoms often lead to a delayed diagnosis.
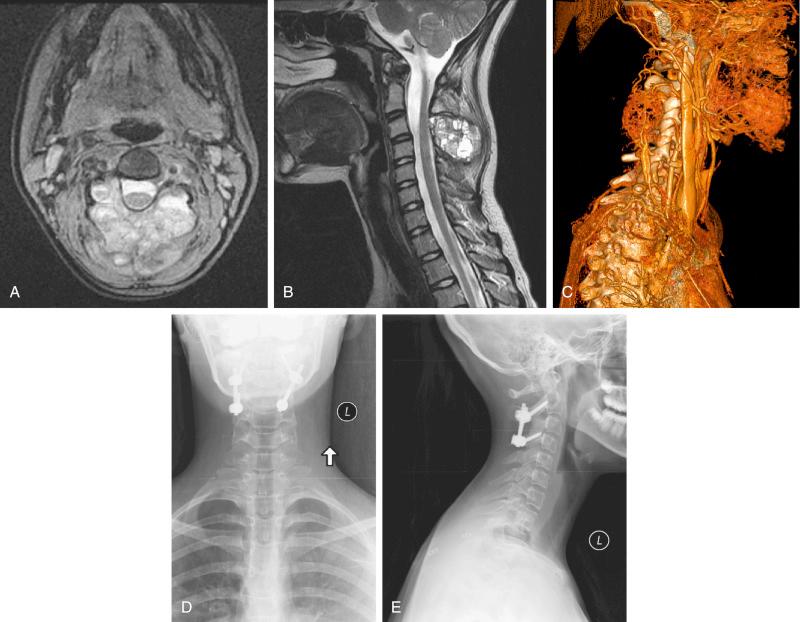
Radiographic features include an expansile lesion with a thin rim of calcification. The cysts have a characteristic “soap bubble appearance” resulting from bony trabeculae and septa. Involvement of multiple vertebral levels is possible, as are pathologic fractures. Computed tomography (CT) scans can reveal multiple fluid-filled cavities. Magnetic resonance imaging (MRI) scans can reveal heterogeneous signals with fluid-fluid levels best seen on T2-weighted images ( Fig. 23-1 ). Despite characteristic imaging, biopsy is necessary to confirm the diagnosis and to differentiate this cyst from other lesions with similar imaging findings, including giant cell tumor and telangiectatic osteosarcoma.
Historically, treatment of aneurysmal bone cysts was intralesional excision with curettage and bone grafting. Because of high rates of local recurrence with this technique, complete surgical resection is recommended with short segment posterior spinal fusion. Preoperative angiography is useful to identify the vascular supply, and preoperative embolization can reduce the risk of bleeding. Although surgical excision is typically considered the treatment of choice for accessible lesions, other treatment options include percutaneous intralesional injection and repeated embolization. Intralesional injection of calcitonin and methylprednisolone is reported to stimulate ossification of the cyst, increase the formation of cancellous bone, and reduce angiogenesis. Repeated, selective arterial embolization procedures have been reported as the potential definitive treatment for aneurysmal bone cysts of the cervical spine that are not amenable to surgical excision. Although it is possible in some cases to avoid the need for surgical intervention, this technique requires multiple embolization procedures over a prolonged time and carries the risk of embolic complications.
Giant cell tumors are common primary bone tumors, but they occur infrequently in the spine above the sacrum. Although these tumors are benign, they can become locally aggressive and metastasize to the lung in up to 14% of cases. A slight female predominance is noted, and the tumors are most commonly found in the third and fourth decades of life. Local, progressive pain in the posterior neck and shoulder is the most common presenting symptom. The diagnosis is often delayed because of the insidious onset of symptoms. Patients can present with radicular symptoms resulting from nerve root compression, and paraparesis or paralysis can occur rarely. Neurologic findings are much more common in patients with giant cell tumors of the cervical spine than with other benign cervical spine lesions.
Characteristic imaging findings include osteolysis and cortical expansion without a marked sclerotic border. A large soft tissue component with a thin sclerotic rim may be visible. Pathologic fractures are relatively common at presentation. The lesions can involve a single vertebra or multiple vertebrae, but the intervertebral space is spared. MRI reveals a hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted images. Biopsy is necessary to confirm the diagnosis.
Although results in the long bone are very successful, results for giant cell tumors of the spine are less promising. Various treatment options have been recommended for cervical spine giant cell tumors depending on the location, involvement of surrounding vital structures, and the patient’s neurologic symptoms. These options include arterial embolization, curettage, surgical excision, radiation therapy, and cryotherapy. Because of the high risk of recurrence, en bloc surgical excision remains the preferred treatment when possible. Local tumor recurrence following intralesional excision is up to 70%; even in cases of attempted en bloc excision, the risk of recurrence is high, up to 31%.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here