Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pressure sores are a common problem associated with great morbidity and cost.
The etiology of pressure sores is multifactorial, and includes pressure, friction, shear, moisture, malnutrition, and infection.
Successful treatment of pressure sores requires a multidisciplinary evaluation in order to accurately stage wounds, identify/eradicate wound/bone infection, minimize risk factors for recurrence, and optimize wound healing potential.
Prevention and treatment of pressure sores should focus on correcting risk factors and optimizing the condition of the patient, including social support. Operative reconstruction should be delayed until the patient is optimized.
As with any wound, pressure sores involving infected soft tissue and/or bone must be thoroughly debrided prior to definitive closure. The lack of overt signs of infection should not give the surgeon a false sense of comfort, as biofilm is usually still present.
Locoregional fasciocutaneous and musculocutaneous flaps remain workhorse flaps, allowing for adequate padding, dead space obliteration, and readvancement/rerotation as needed.
Prevention remains the most effective treatment of pressure sores.
![]() Access video lecture content for this chapter online at Elsevier eBooks+
Access video lecture content for this chapter online at Elsevier eBooks+
The term pressure ulcer applies specifically to any injury to the skin and underlying tissue that is due to pressure. The terminology is quite imprecise: while an ulcer usually refers to an open wound, not all pressure ulcers are open (for example, stage I pressure ulcers and deep tissue injuries are usually closed at the time of diagnosis). Synonyms of pressure ulcer are also imprecise, namely decubitus ulcer , which implies that the ulcer occurred from lying down – the Latin word decumbere means “to lie down”. In reality, many types of pressure ulcers are not due to lying down. For example, ischial pressure ulcers are due to sitting on poorly padded surfaces for prolonged periods of time. Some pressure ulcers on the leg are due to a poorly padded cast, while others on the ear are due to prolonged wear of nasal cannulas in hospitalized patients. The terms pressure ulcer and pressure sore are likely the best terms to use when describing these lesions ( ![]() ).
).
Pressure ulcers are fairly common among the elderly, critically ill, and spinal cord injury population. Every year, approximately 2.5 million patients develop pressure ulcers in the United States. In 1999, 14.8% of patients in acute care facilities had a pressure ulcer, 7.1% of which were facility-acquired. In 2009, those prevalence rates were 12.3% and 5%, respectively. Overall prevalence rates were highest in long-term acute care facilities (22%), while facility-acquired rates were highest in adult intensive care units (ICUs). Overall, pressure ulcer prevalence does not appear to be decreasing over the past few decades, despite significant advances in treatment and prevention.
Particular populations have been identified as particularly high risk. There is a strong association between hip fractures and pressure ulcers, with incidences ranging from 8.8% to 55%. In patients with spinal cord injury (SCI), the incidence of pressure ulcers has been reported to be as high as 60%.
Pressure ulcers also constitute a significant economic burden on the healthcare system. However, calculating the exact financial costs associated with pressure ulcers is complex, since many patients are admitted with pressure ulcer-related problems, such as septicemia, and carry pressure sore as a secondary diagnosis. The National Pressure Ulcer Advisory Panel (NPUAP) has estimated the cost to treat and heal hospital-acquired pressure sores to be up to $100,000 per patient. When taking the additional costs, both surgical and non-surgical, of managing pressure sores at nursing homes and home care facilities into consideration, the annual financial burden in the United States was estimated by the Agency for Healthcare Research and Quality at approximately $11 billion in 2006. Ten years later, Padula et al . estimated the cost to have increased to $26.8 billion annually.
In 2002, the Center for Medicare & Medicaid Services (CMS) identified eight hospital-acquired complications as never events . These never events include hospital-acquired stage III and IV pressure ulcers. In 2008, CMS implemented the Hospital-Acquired Conditions (HACs) initiative, a policy that denies reimbursement for these preventable conditions. Waters et al . analyzed data from 1381 US hospitals between July 2006 and December 2010, comparing the rate of stage III/IV pressure sores before and after the implementation of the HACs initiative. Unfortunately, the initiatives did not seem to lead to a decrease in the incidence of pressure ulcers over that four year period.
Classically, in the early acute phase after SCI, the sacral area tends to be the most common site of pressure sores as patients are treated for their initial injuries in the supine position. In the later phases after SCI, ischial pressure ulcers become more common as patients begin to sit up. Overall, the most common location for pressure ulcers is the sacrum (28% to 36%), followed by the heel (23% to 30%) and the ischium (17% to 20%).
![]() Access the Historical Perspective section online at Elsevier eBooks+
Access the Historical Perspective section online at Elsevier eBooks+
Multiple studies describe risks associated with the development of pressure sores. Fisher et al . found that increased age, male sex, friction, shear, moisture, malnutrition, immobility, and altered sensorium all independently place patients at risk of developing pressure sores. More recently, Baumgarten et al . found that increased age, male sex, moisture caused by incontinence, poor nutrition, and immobility limiting turning in bed all correlated with the diagnosis of pressure sores. Recognition of these factors has led to the understanding of pressure sores as multifactorial entities.
As their name implies, the main culprit in pressure ulcer formation is pressure, specifically sustained external pressure exceeding the closing pressure of nutrient capillaries. In 1930, Landis performed a classic series of experiments and found that the average capillary closing pressure is approximately 32 mmHg. Fronek and Zweifach later reported similar findings, noting perfusion pressures between 20 and 30 mmHg ( Fig. 16.1 ).
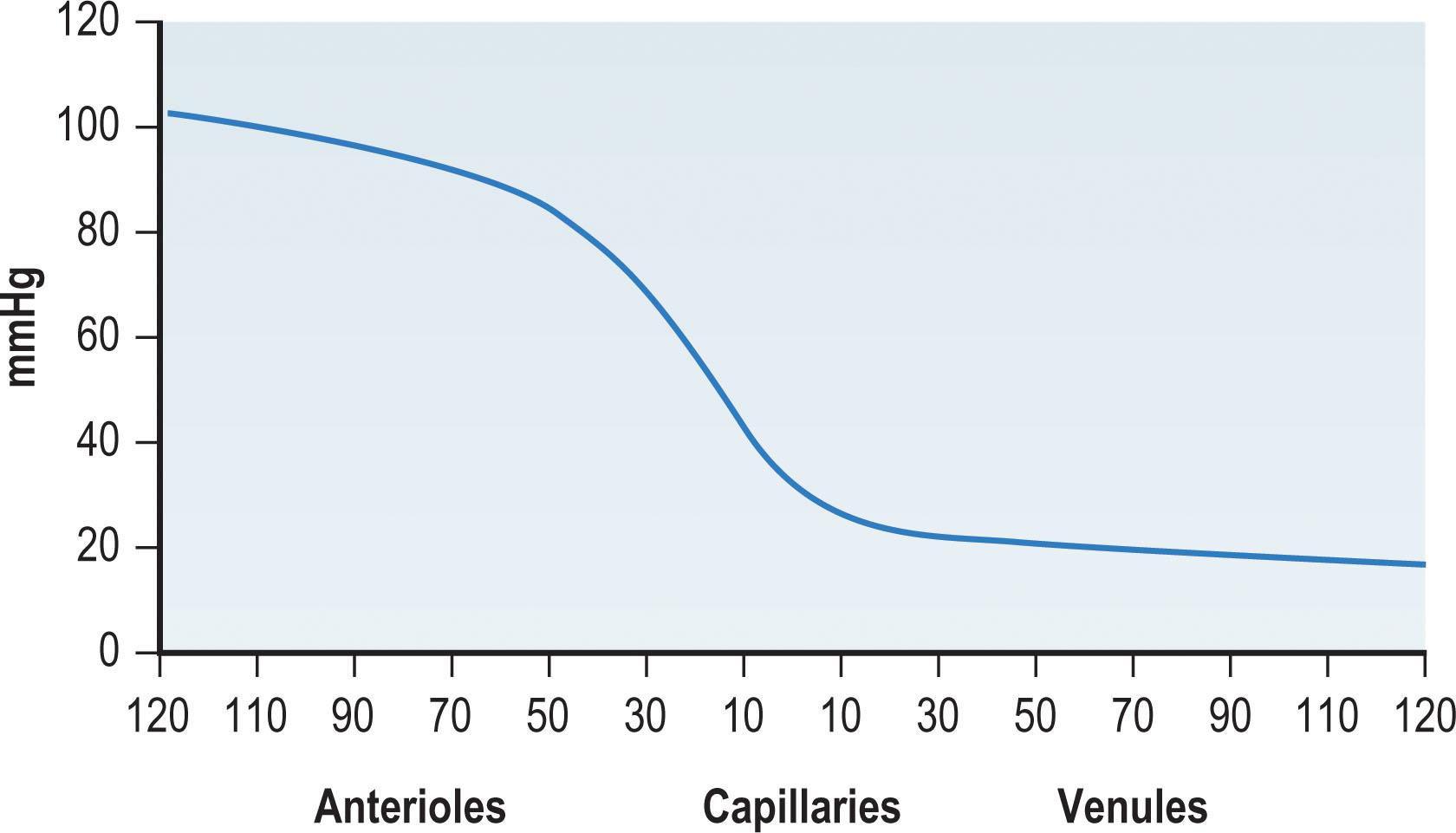
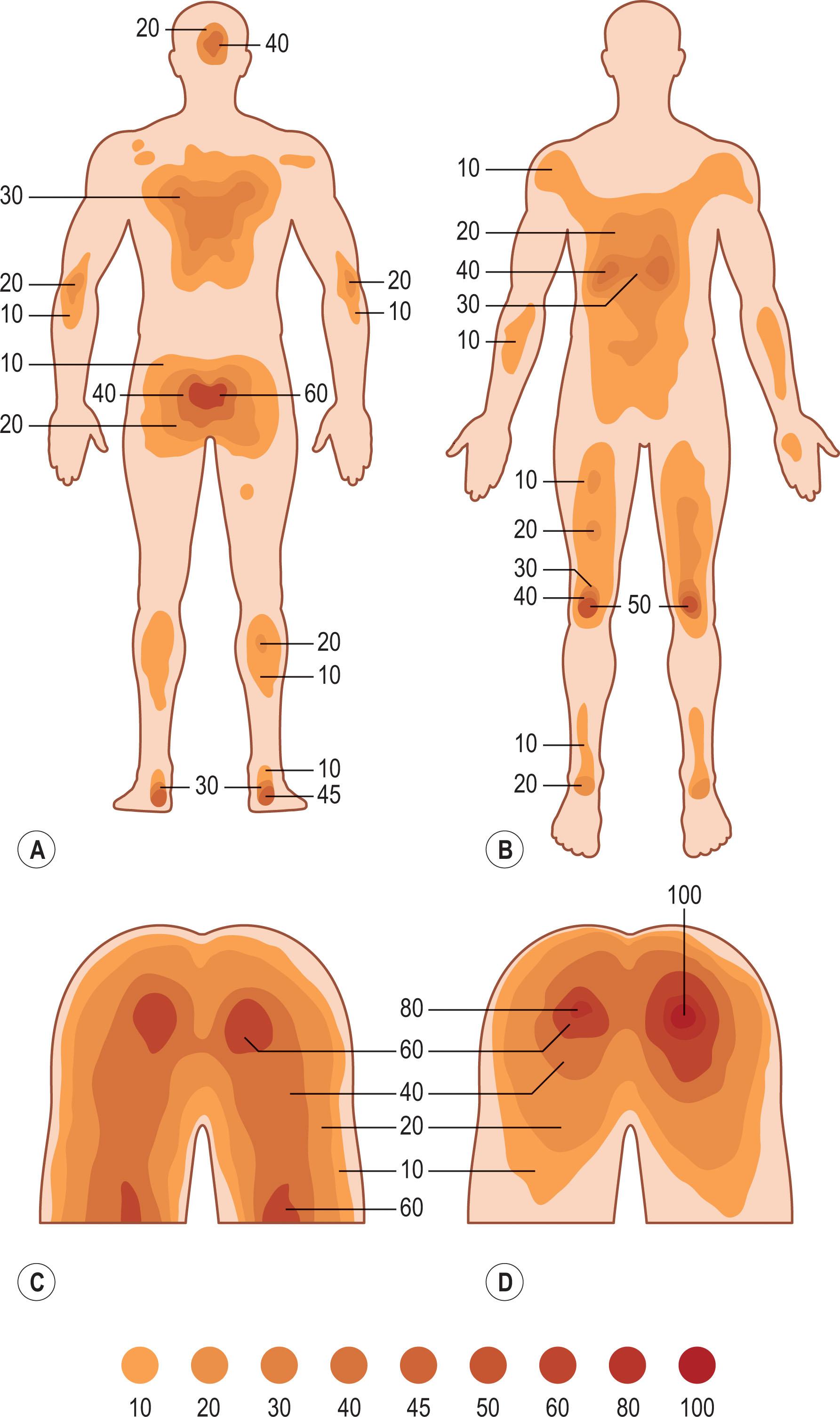
Lindan et al . measured pressure points : when supine, the highest pressure is applied to the sacrum, buttocks, heel, and occiput, all of which are subjected to pressures of roughly 50–60 mmHg. When sitting, pressures up to 100 mmHg are applied over the ischial tuberosities ( Fig. 16.2 ).
However, simply applying pressure in excess of these levels does not necessarily result in tissue ischemia. Much of the pressure applied to tissues is sustained by the connective tissues surrounding the blood vessels. Furthermore, autoregulatory mechanisms tend to vasodilate blood vessels in response to pressure, a process known as pressure-induced vasodilation , which will be discussed in more detail in the Neurological Injury section below.
Efforts have been made to quantify the degree and time of pressure necessary to cause tissue damage. Dinsdale found that pressure roughly double capillary closing pressure, applied for 2 hours, resulted in irreversible ischemic damage to tissue. Pressures below this threshold were unlikely to cause tissue necrosis. Kosiak et al . noted similar findings in dog tissues, but noted that if the pressure was released every 5 minutes, no injury occurred. Groth noted, in rabbits, that higher pressures caused damage in shorter amounts of time. Husain had similar results in a rat model, also noting that pressure applied over a large area was less injurious than when applied over a smaller one.
Furthermore, various tissues have different susceptibility to pressure. Nola and Daniel both noted that muscle was more susceptible to pressure injury than skin, requiring less pressure for a shorter duration, likely owing to its increased metabolic demands.
Friction is the force resisting relative motion between the patient’s skin and other surfaces, such as bedding, transfer devices (sheets, rollers, slide boards), various appliances and orthotics, and mobility devices such as wheelchair cushions. Excess friction causes direct injury to the skin, consisting of abrasions, blisters, and even tears in patients with fragile skin ( Fig. 16.3 ). While relatively minor in isolation, such injuries may potentiate further damage. As the integrity of the skin is compromised, transepidermal water loss increases and allows moisture to accumulate. Moisture, in turn, increases the coefficient of friction and promotes adherence to sheets and other contact surfaces, leading to a positive feedback loop.
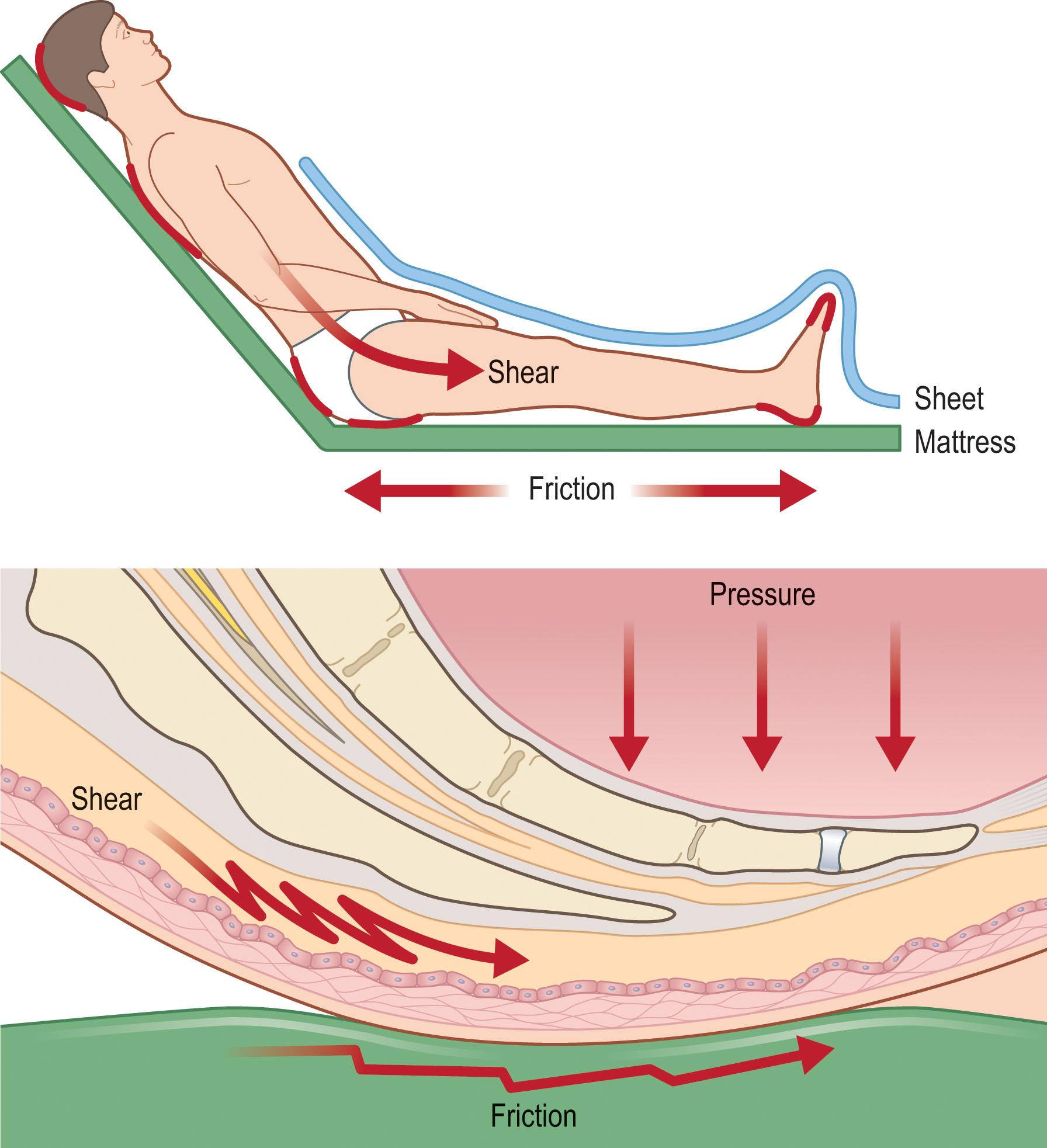
Shear, on the other hand, represents the deep tissue injury that occurs as a result of friction. When friction causes the skin and subcutaneous tissue to move in relation to the deeper tissues, blood vessels are stretched, angulated, and potentially injured. Shear forces potentiate the effects of pressure, acting in synergy to cause tissue injury. Dinsdale noted that addition of shear forces greatly decreased the amount of pressure needed to cause ulceration in a pig model, concluding that “a shear force is more disastrous than a vertical force”. Goossens et al . noted similar results in human subjects, finding that the addition of a small shear component drastically reduced the level of pressure needed to cause critical ischemia over the sacrum.
Transferring patients, sliding or dragging them in bed, “boosting” them up in bed, or allowing them to elevate themselves in bed by pushing with elbows and heels all cause significant shear. Certain positions also cause elevated levels of shear: patients in the semi-Fowler’s position or sliding down in a wheelchair both experience significant shear over the lower back and buttocks. This can explain why wheelchair-bound patients may still develop a sacral pressure sore if they are not sitting upright in their chair, despite the fact that theoretically the ischial tuberosities should be bearing the majority of their weight.
Pressure sores are an ancient problem, observed at autopsy of Egyptian mummies. As early as the 16th century, Ambrose Paré recognized the importance of pressure and nutrition in the treatment of these lesions. By 1873 Sir James Paget correctly surmised that pressure led to compression of the cutaneous vasculature, leading to necrosis. Though he incorrectly attributed them to central nervous system lesions, in 1878 Charcot provided a detailed description of what he termed decubitus ominosus , noting not only the clinical manifestations of the disease but the poor prognosis they portended. Though well over a century old, Charcot’s description could be applied to any number of modern patients with pressure sores of various stages:
The skin there has a rosy hue, sometimes it is dark red, and even violet, but the dolor disappears momentarily on pressure with the finger. […] On the morrow, or after-morrow, vesiculae or bullae make their appearance toward the central part of the erythematous patch; […] The subcutaneous connective tissue, and sometimes even the subjacent muscles are themselves already invaded by sanguine infiltration. […] The eschars, if they but attain a certain extent, constitute, as you are aware, dangerous foci of infection; and, in fact, putrid intoxication, denoted by a more or less intense remittent fever.
In 1938, John Staige Davis was the first to suggest reconstructing the fragile scar of a healed pressure ulcer with a flap. However, it was not until 1945 that Lamon described the first closure of open pressure sores. Thereafter, surgical treatment of pressure sores gained immediate attention, and by the end of the decade most of the surgical techniques used in the treatment of pressure sores today had been reported, including excision of bony prominences, use of flaps, tension-free closure, and back-grafting of donor sites.
In the following decades, wound care became ever more complex, and numerous technical refinements were developed, but the basic concepts of patient optimization, complete debridement, and tension-free soft-tissue coverage have remained constant.
Moisture also potentiates the effects of pressure. Moisture increases the coefficient of friction between the skin and other surfaces, making friction and shear injuries more likely. Moisture also directly causes skin maceration and breakdown.
Though excess moisture can have many causes, urinary and fecal incontinence are common in patients with pressure sores, with rates from 20% to 77% for urinary incontinence and 17% to 50% for fecal incontinence. In addition to causing excess moisture, urine also negates the acidic pH of skin through the introduction of nitrogen derivatives. Fecal contamination introduces a large bacterial load. Lowthian noted a fivefold increase in pressure sores in patients who were incontinent, though he did not distinguish between urinary and fecal incontinence. While some studies have found a relationship between urinary incontinence and pressure sores, others have failed to find a correlation while noting a significant correlation between fecal incontinence and pressure sores.
While excess moisture is clearly deleterious, the opposite is also true. Excessively dry skin is prone to cracking, has decreased tensile strength and lipid content, and impaired barrier function, and this appears to be an independent risk factor for pressure ulceration. Thus the importance of controlling the microclimate around the patient’s skin within specific parameters.
Malnutrition, manifested by low serum albumin, prealbumin, or transferrin levels, is a common comorbidity in patients in pressure ulcers. The prevalence of malnutrition ranges from 1%–4% in elderly patients living at home, to 20% in hospitalized patients and 37% in institutionalized patients. Protein malnutrition impairs wound healing and increases the risk of wound infection. In addition, protein malnutrition, as measured by low serum albumin, is an independent predictor of postoperative mortality. The importance of nutrition for pressure ulcer healing will be discussed in more detail later in this chapter.
Pressure sores are the most common complication and the second most common cause of hospital admission in patients with a spinal cord injury (SCI). While this is mostly due to the loss of protective sensation, there is also a large role for the loss of pressure-induced vasodilation . In healthy individuals, moderate pressure over tissue is known to induce vasodilation in that tissue, leading to increased blood flow. This pressure-induced vasodilation is mediated by a local reflex loop, whereby local sensory nerves detect pressure and induce the release of calcitonin gene-related peptide, which mediates vasodilation. In patients with impaired peripheral nerve function, such as diabetics, paraplegics, and the elderly, pressure-induced vasodilation is lost, making tissues much more susceptible to ischemia as a result of local pressure.
Another neurologic issue that may potentiate the formation of pressure ulcers is spasticity, which affects up to 78% of SCI patients one year after injury. Spasticity is characterized by hyperreflexia, clonus, and increased muscle tone. While it is not included in most pressure sore risk scales, it directly increases mechanical stress, alters weight distribution, and complicates patient positioning, skin inspection, and hygiene.
Chronic wounds seldom exhibit overt signs of infection (erythema, purulence). Instead, bacteria in chronic wounds are often encased in a extracellular polymeric substance (EPS), forming what is known as biofilm. Biofilm infections are problematic in pressure ulcers for several reasons. Biofilm infections are difficult to diagnose using traditional culture techniques. Instead, biofilm requires advanced diagnostic techniques such as polymerase-chain reaction and scanning electron microscopy. In addition, bacteria encased in biofilm are much more recalcitrant to topical and systemic antibiotic therapy than bacteria in the planktonic state. This is because the EPS acts as a barrier to antibiotic diffusion, and bacteria in biofilm exist in a low metabolic state.
Biofilms are also known to promote an inflammatory milieu that inhibits wound healing. This milieu is rich in proteases and ceramidase, both of which cause wound and skin degradation. Biofilm promotes the influx of numerous but ineffective host neutrophils. Those neutrophils in turn produce reactive oxygen species that further exacerbate the inflammatory milieu.
Pressure ulcers have an imbalance of matrix metalloproteinases (MMPs). MMPs are zinc-dependent proteases, which are capable of degrading various extracellular matrix proteins, and which play a role in cell proliferation, differentiation, apoptosis, angiogenesis, and host immunity. Under homeostatic conditions, a balance must be maintained between MMPs and their counterparts, namely tissue inhibitors of metalloproteinases (TIMPs) in order to maintain orderly formation/degradation of extracellular matrices. In chronic wounds from 56 patients with stage III/IV pressure sores, Ladwig et al . found that as chronic wounds heal, the ratio of MMP-9:TIMP-1 decreases, thus suggesting that higher levels of MMP-9 and TIMP-1 are necessary for appropriate healing of chronic wounds and may serve as markers of healing/non-healing.
Pressure ulcers are also known to have decreased levels of cytokines that promote wound healing, such as platelet-derived growth factor (PDGF), basic fibroblast growth factor (bFGF), epidermal growth factor (EGF), and transforming growth factor-beta (TGF-β).
The most commonly used staging classification for pressure ulcers is the one originally developed by Shea, and modified by the National Pressure Sore Advisory Panel Consensus Development Conference in 2007. Though used in basic form for many years, two additional definitions, suspected deep-tissue injury and unstageable, have been added relatively recently to the NPUAP system.
| Stage | Description |
|---|---|
| I | Intact skin with nonblanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. The area may be painful, firm, soft, warmer, or cooler as compared with adjacent tissue. Stage I may be difficult to detect in individuals with dark skin tones. May indicate “at risk” persons (a heralding sign of risk). |
| II | Partial-thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled blister. Presents as a shiny or dry shallow ulcer without slough or bruising. † This stage should not be used to describe skin tears, tape burns, perineal dermatitis, maceration, or excoriation. |
| III | Full-thickness tissue loss. Subcutaneous fat may be visible, but bone, tendon, and muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. The depth of a stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput, and malleolus do not have subcutaneous tissue, and stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep stage III pressure ulcers. Bone/tendon is not visible or directly palpable. |
| IV | Full-thickness tissue loss with exposed bone, tendon, or muscle. Slough or eschar may be present on some parts of the wound bed. Often includes undermining and tunneling. The depth of a stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput, and malleolus do not have subcutaneous tissue, and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon, or joint capsule) making osteomyelitis possible. Exposed bone/tendon is visible or directly palpable. |
| Unstageable | Full-thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green, or brown) and/or eschar (tan, brown, or black) in the wound bed. Until enough slough and/or eschar is removed to expose the base of the wound, the true depth and therefore stage cannot be determined. Stable (dry, adherent, intact, without erythema, or fluctuance) eschar on the heels serves as “the body’s natural (biological) cover” and should not be removed. |
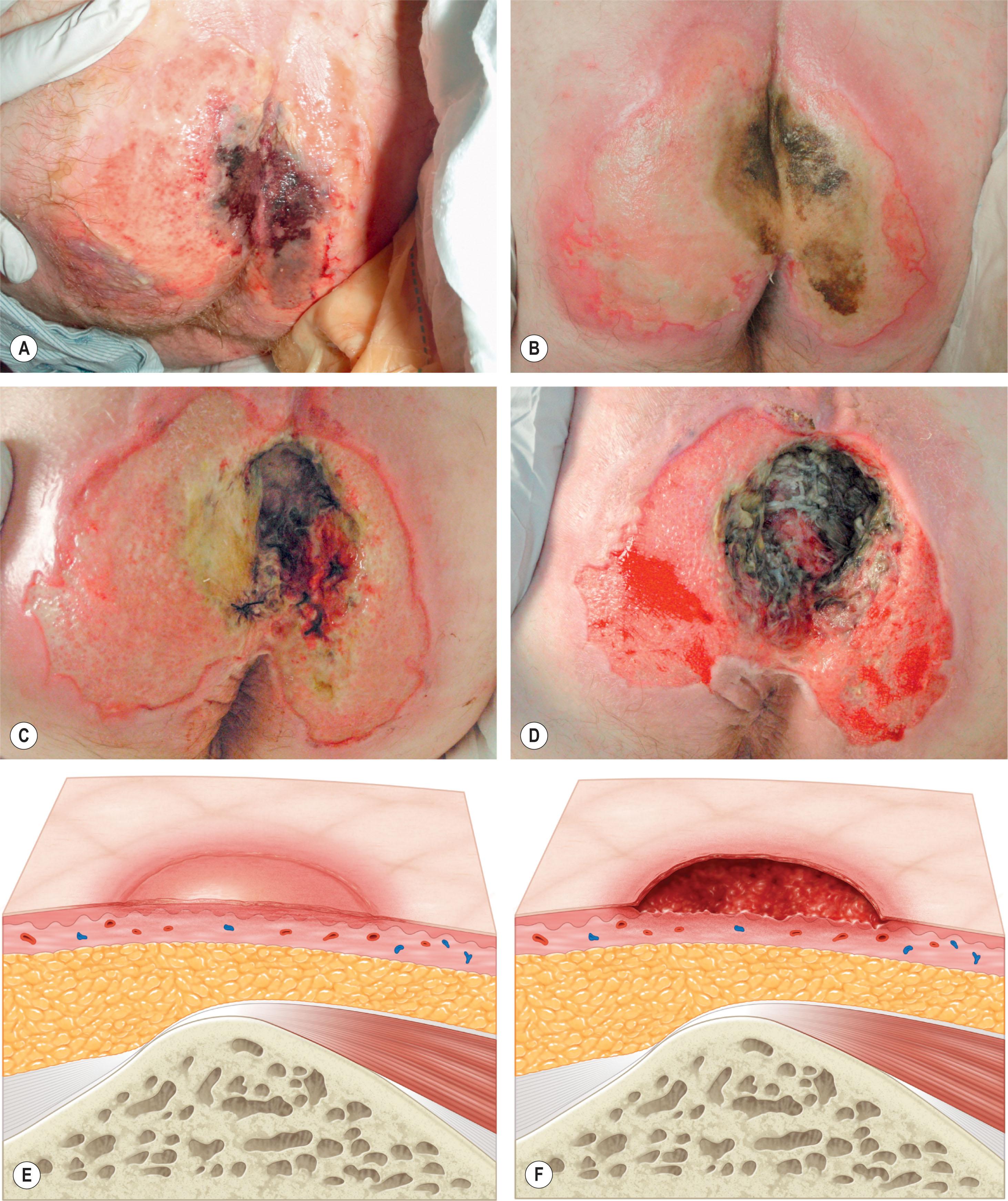
“Stage” is somewhat of a misnomer, as it implies a progression that does not reflect reality. Stage IV ulcers do not necessarily start as stage I ulcers, a fact emphasized by the addition of the suspected deep-tissue injury classification. Likewise, healing pressure sores do not progress in reverse order but instead granulate and close by secondary intention in the absence of surgical treatment. Though panel members were aware of these issues, the term “stage” was retained due to its historical use and widespread adoption.
When evaluating a new patient with a pressure sore, several factors must be considered. Both the wound and the patient should be meticulously examined. A wound history, noting the onset, duration, prior treatments and procedures, and wound care regimen, should be documented. Wounds should be measured in three dimensions, with notes made regarding any tunneling or undermining. The tissue at the margins of the wound should be examined for any signs of occult deep-tissue injury, infection, and scarring. The base of the wound should be characterized, noting the presence of eschar, slough, or other necrotic tissue. If necrotic material obscures the base of the wound, it should be debrided until a full assessment can be performed. Granulation should be noted in terms of both character and percentage of the wound bed covered. Exposed tissues, such as bone, tendon, or joint, should be noted. If easily accessible, the bone should be characterized as hard, soft, or obviously necrotic. The amount and character of the wound exudate should be documented as well. A measuring tape and camera can improve documentation and make tracking progression easier.
Attention should also be paid to the risk factors specific to pressure sores. An attempt should be made to identify the etiology of the patient’s pressure sore, though it is often multifactorial. Sources of friction, shear, and pressure should be evaluated, and recommendations for proper pressure relief surfaces and skin care regimens made as appropriate. If incontinence is present an effort should be made to control this, possibly involving the assistance of other specialties. Likewise, spasticity should be evaluated and, if needed, controlled medically or surgically. Nutrition should be evaluated with serum albumin and prealbumin. If needed, nutrition should be supplemented, and progress of therapy monitored with weekly serum studies. Any underlying medical problems, such as hypertension, diabetes, or history of cardiac disease, should be investigated and optimized.
A reasonable initial set of studies would include a complete blood count, basic metabolic panel, creatinine, and blood urea nitrogen. Albumin and prealbumin should be obtained at the initial consult and regularly thereafter to evaluate for malnutrition and follow the progression of therapy. C-reactive protein and erythrocyte sedimentation rate (ESR) can be obtained to evaluate for osteomyelitis, though they will almost certainly be positive when deep ulcers are present. The evaluation of the pressure sore patient for osteomyelitis is discussed in the next section. Unlike core-needle and open surgical biopsy, swab cultures of the open pressure sore are of little value and should not be used to direct antibiotic therapy.
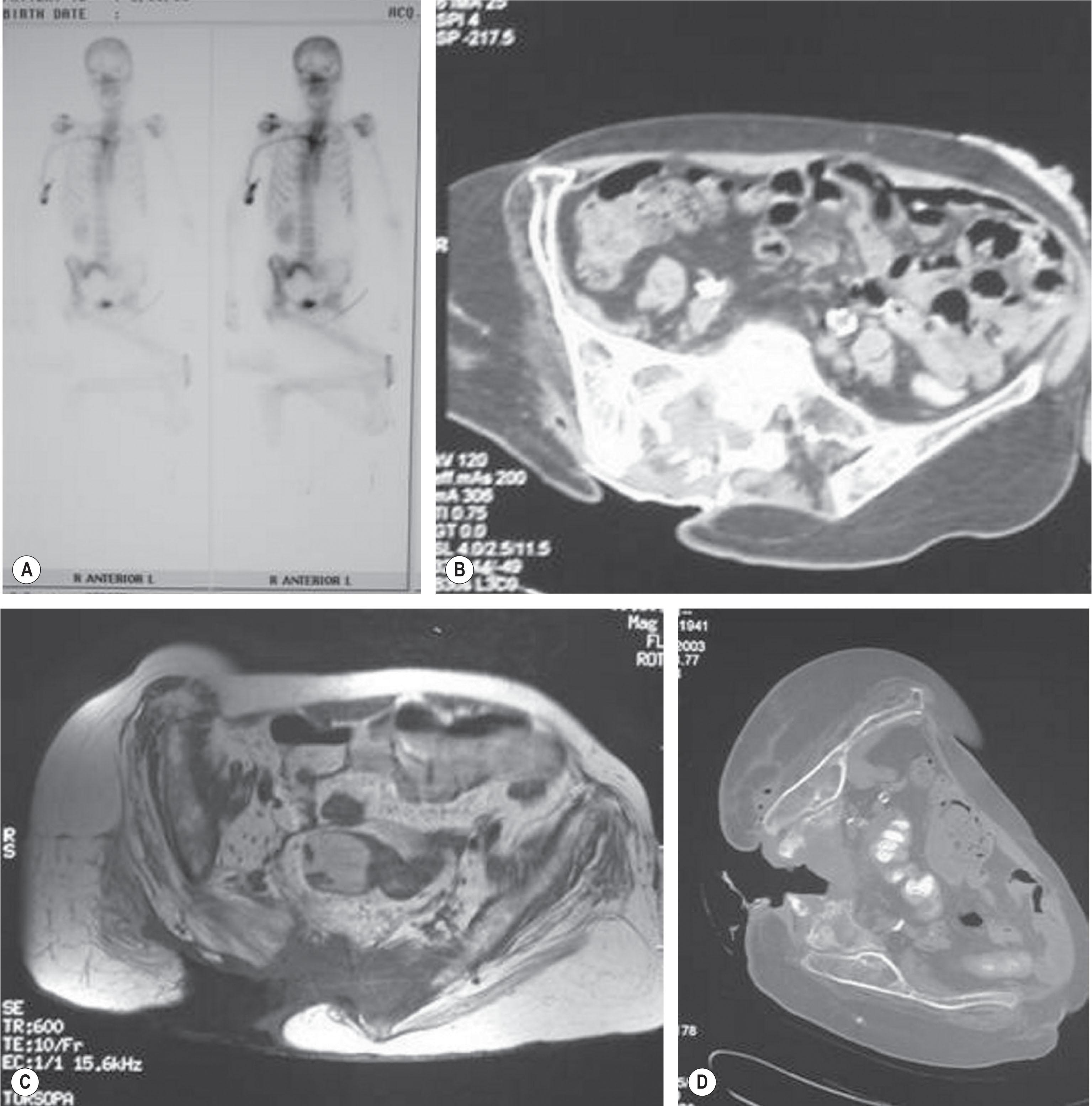
Osteomyelitis has been known for years to cause wound infection and breakdown after reconstruction ( Fig. 16.5 , Algorithm 16.1 ). Therefore, the diagnosis of osteomyelitis must be established before surgical reconstruction is undertaken.
The gold-standard for the diagnosis of osteomyelitis remains open bone biopsy. This technique also allows for identification of the pathogenic organisms, thereby facilitating tailored antibiotic therapy. However, attempts have been made to identify less invasive diagnostic modalities. Some individual modalities have been attempted in isolation, but have not been found to be accurate. The clinical assessment of bone (firm versus soft and crumbly) is a poor predictor of osteomyelitis.
Lewis et al . found that a combination of white blood cell count, ESR, and two-view X-ray was an easy, accurate, and noninvasive method to diagnose osteomyelitis, with a sensitivity of 89% and a specificity of 88%. Only one positive test was needed to make the diagnosis. In contrast, they found that isolated radiographic imaging (CT or X-ray) has limited sensitivity (10%–30%), but high specificity (90%–100%).
Rubayi found that nuclear bone scans tend to have limited utility in chronic pressure ulcers, as they are nonspecific, and therefore have a high rate of false positivity for osteomyelitis.
MRI has been found to have an overall accuracy of 97%, sensitivity of 98%, and specificity of 89%. Not only is MRI accurate, but it also helps define the extent of infection, which can guide surgical resection.
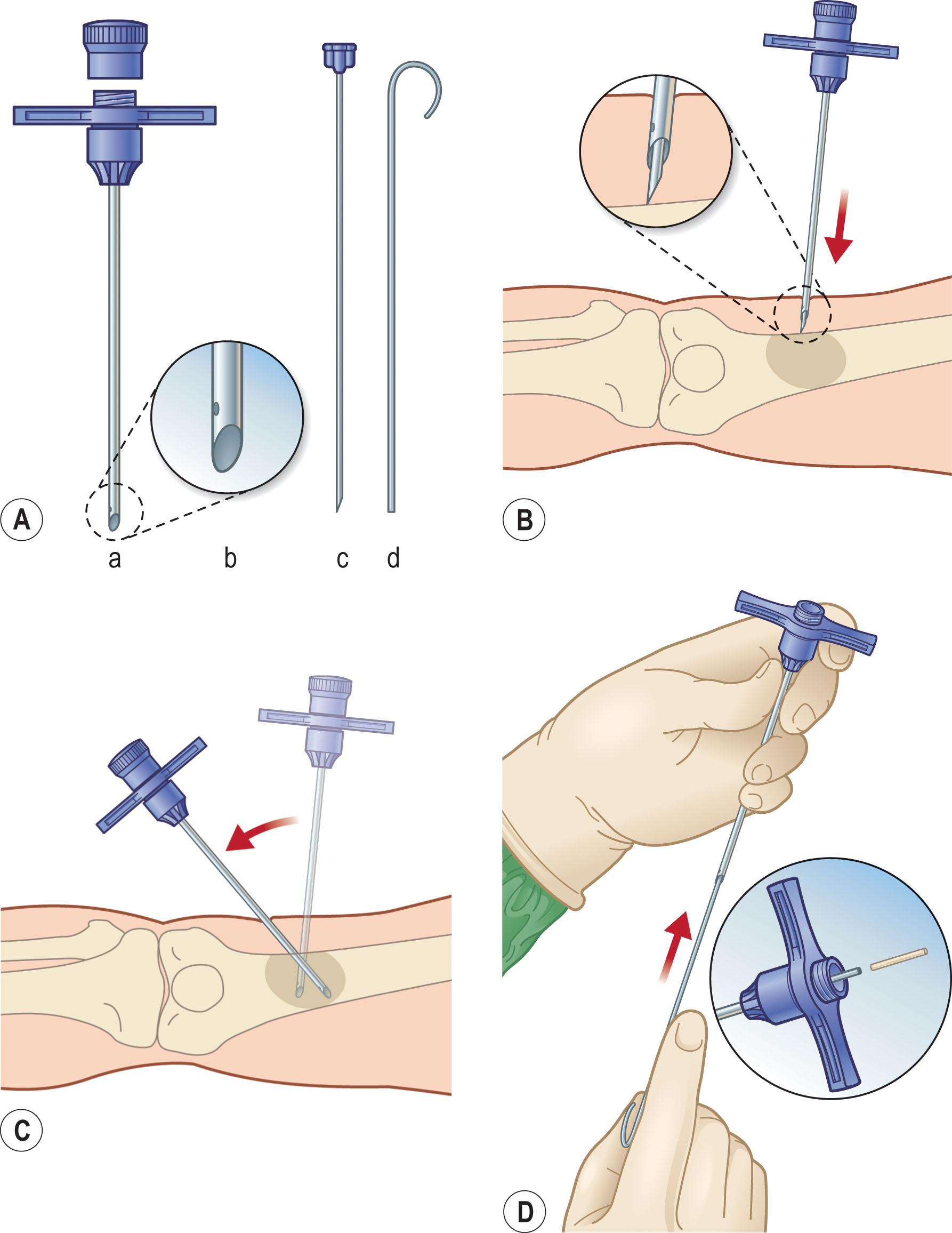
Han et al . analyzed the results of two-stage surgical management, consisting of wound debridement and Jamshidi core needle bone biopsy at the first operation, followed by delayed wound closure ( Fig. 16.6 ). If the biopsy results were positive, closure was delayed for 6 weeks while the osteomyelitis was treated with antibiotics; otherwise the wound was closed once biopsy results were available. The authors also noted that bone cultures alone were not as useful as bone cultures and histopathology of the bone biopsy together, and found that the biopsy had positive and negative predictive values of 93% and 100%, respectively. These results are in keeping with several other studies that support the utility of bone biopsy in the diagnosis of osteomyelitis. Marriott and Rubayi have used the results of bone biopsy to determine the duration of antibiotic therapy, in some cases truncating treatment if pathology reveals only chronic osteomyelitis.
Ultimately, the combination of MRI with bone biopsy allows high diagnostic accuracy, while identifying the extent of disease and the pathologic organism.
Psychological problems are common in the pressure sore population, with a diagnosis of major depression in SCI patients ranging from 22% to 47.4%. Risk factors for depression include female gender, younger age, multiple previous operations for pressure sores. Foster et al . suggest that psychological factors may play a role in pressure ulcer recurrences.
All patients with pressure sores should be optimized with regard to the risk factors already enumerated. It is worth remembering that pressure sores are rarely life-threatening, and there is no need to rush to treatment or surgery if the patient has not been optimized. Many superficial wounds will heal with conservative therapies if correctable risk factors are identified and addressed. On the other hand, a patient who is malnourished, bedbound on an inappropriate mattress, with undiagnosed osteomyelitis, is doomed to failure regardless of the surgical technique used.
A judgment must be made whether a wound is likely to heal by secondary intention or whether a flap is required to resurface the wound and/or fill dead space after debridement. In general, stage I and II pressure sores can be treated nonoperatively, while stage III and IV ulcers require flaps. Patients with suspected deep-tissue injury and unstageable ulcers should be debrided until they can be clearly staged. While surgical debridement is the gold standard, other methods can be used as appropriate.
While operative treatment is often delayed while the patient is optimized and risk factors corrected, it is a rare patient who never qualifies for any attempt at reconstruction. Obviously critically ill patients who cannot tolerate surgery should be stabilized before any sort of reconstruction is entertained. More uncommon is the patient with multiple severe comorbidities whose risk factors cannot be easily corrected, due to either medical or social factors. In such cases, chronic wound care may be preferable to attempted reconstruction that is doomed to failure and recurrence.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here