Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Optimal preparation for an operation facilitates a successful result and protects the patient and physician.
The most significant risk factors for postoperative morbidity are preoperative conditions. They may affect the operation, anesthesia, and postoperative course and may preclude the procedure altogether.
Approximately 0.5% of the general population and 1.5% of women older than 55 years are receiving continuous glucocorticoids.
Latex allergy is directly responsible for 12% of the perioperative anaphylactic reactions in adult women and for 70% in children. Health care workers, women with spinal cord injuries, or those who have had to perform self-catheterization are at higher risk for latex allergy.
The preoperative physical examination should answer three basic questions:
Has the primary gynecologic disease process changed since the initial diagnosis?
What is the effect of the primary gynecologic disease on other organ systems?
What deficiencies in other organ systems may affect the proposed surgery and hospitalization?
An examination while the patient is under anesthesia may provide additional information, help avoid intraoperative surprises, and affect the surgical plan.
It is estimated that 60% of routinely ordered tests would not have been performed if tests had been ordered only for an indication discovered by history or physical examination.
The American Society of Anesthesiologists (ASA) Practice Advisory for Preanesthesia Evaluation states that routine preoperative tests, defined as a test ordered in the absence of a clinical indication or purpose, should not be ordered.
A preoperative complete blood cell count and blood type and antibody screen should be performed before most major gynecologic surgeries.
Other individualized preoperative laboratory testing should be determined based on the age of the woman, extent of the surgical procedure, and findings at the time of complete history and physical examination.
Determining the preoperative creatinine or blood urea nitrogen level is especially important if the woman is going to be treated with antibiotics excreted by the kidneys.
A pregnancy test may be appropriate, depending on contraceptive and sexual history. The PREG criteria can be used to optimize screening for pregnancy in women 18 years and older. A pregnancy test should almost always be performed if the patient is a teenager, as menstrual history is at best an imperfect indication of an early pregnancy.
Serum electrolyte levels are ordered for women taking diuretics or those with a history of renal disease or heart disease. Also, serum electrolyte levels should be evaluated in women with vomiting, diarrhea, ileus, bowel obstruction, or any condition that affects electrolyte balance.
Routine radiographs on all patients often do not affect perioperative management in elective gynecologic surgery, but they should be ordered for women who are current or former smokers, women with cardiac or pulmonary symptoms, immigrants who have not had a recent chest film, and women older than 70 years.
A baseline preoperative electrocardiogram has been found to be cost effective in asymptomatic women 60 years and older without a history of cardiac disease or significant risk factors.
In the present medicolegal climate, the absence of informed consent is cited as a major problem in many lawsuits.
Preoperative orders should be standardized to avoid omissions, and electronic order sets are standard at most institutions.
If an enhanced recovery pathway is being used, the patient can usually eat solid food up until midnight and clear liquids until 30 minutes before presenting to the hospital.
To avoid hypoglycemia, most enhanced recovery after surgery (ERAS) protocols allow patients to eat solid food up to 6 hours before surgery.
Anesthesiologists classify surgical procedures according to the patient’s risk of mortality using the ASA risk class stratification (classes 1 to 5).
An emergency operation doubles the mortality risks for ASA classes 1, 2, and 3; produces a slightly increased risk in class 4; and does not change the risk in class 5.
Enhanced recovery refers to a bundled process with the aim of attenuating pathophysiologic changes and the stress response occurring with surgery. These processes replace traditional but untested practices of perioperative care with the primary goal of hastening recovery.
Adoption of enhanced recovery has resulted in an average reduction in length of stay of 2.5 days and a decrease in complications by as much as 50%.
Enhanced recovery achieved the greatest benefit in patients undergoing complex cytoreduction for ovarian cancer, of whom 57% underwent colonic or small bowel resection.
The popularity of thoracic epidural anesthesia (TEA) after major open gynecologic surgery is due to its effectiveness in controlling pain and the quicker return of bowel function seen in patients with epidural anesthetics.
The role of TEA in an ERAS care plan is less clear because it can compete at times with some of the ERAS goals and its use. TEA has been associated with more interventions to treat hypotension, longer length of hospital stay, and more complications in one series of early stage endometrial cancer patients.
A surgical site infection (SSI) is one of the most common complications after surgery. SSIs dissatisfy patients and providers, but they also increase the cost of surgical care, increase morbidity, and can increase mortality.
There are three classifications of SSIs according to the Centers for Disease Control and Prevention and the American College of Surgeons National Surgical Quality Improvement Program: (1) superficial incisional, (2) deep incisional, and (3) organ/space.
Elements shown to decrease SSI that are often included in reduction bundles include preoperative nicotine cessation, preoperative antiseptic showering and chlorhexidine preparation, using hair clippers instead of a razor, appropriate preoperative antibiotic selection, normothermia, and glycemic control.
There is abundant literature supporting the use of prophylactic antibiotics in gynecology. The incidence of febrile morbidity may be reduced from 40% to 15% and the incidence of pelvic infection decreased from 25% to 5%.
The current guidelines for antimicrobial prophylaxis for vaginal or abdominal hysterectomy include the first- or second-generation cephalosporins of cefazolin, cefotetan, cefoxitin, or ampicillin-sulbactam.
Among women with a β-lactam allergy, the recommended combinations are (1) clindamycin or vancomycin plus an aminoglycoside, or (2) aztreonam, or (3) a fluoroquinolone, metronidazole, and aminoglycoside, or (4) a fluoroquinolone alone.
Comparative studies have documented that single-dose therapy is as effective as 24 hours of antibiotics. No advantage exists to continuing prophylactic antibiotics beyond the immediate operative period.
Vaginal surgery continues to carry the lowest risks of SSI and should remain the preferred surgical approach when feasible. However, when minimally invasive approaches to hysterectomy replace laparotomy, the risk of SSI can be reduced by up to 16-fold.
Multiple studies have documented a two- to threefold increase in the SSI rate directly related to perioperative shaving; if the hair is mechanically in the way, it should be clipped just before the operation.
The use of chlorhexidine gluconate with 70% isopropyl alcohol as a skin preparation demonstrated a 40% reduction in SSIs in clean contaminated (type II) wound types compared with a 10% povidone-iodine solution.
The risk of an SSI is significantly increased in the setting of smoking, and patients should be encouraged to stop as patients in a smoking cessation program had perioperative complication rates of 21% versus 41% in controls.
Hypothermia has been shown to increase the incidence of wound infections, postoperative myocardial events, and perioperative blood loss; impair drug metabolism; and prolong postoperative recovery. Preventing intraoperative hypothermia improves surgical outcomes.
Glucose levels greater than 180 mg/dL among patients with and without diabetes increase the risk of SSI by twofold. Perioperative blood glucose levels should be maintained at less than 200 mg/dL for all patients.
Category 1A evidence has demonstrated that strict glucose control (80 to 130 mg/dL) in both patients with diabetes and those without does not improve SSI rates over glucose levels less than 200 mg/dL. Strict control may have detrimental effects on postoperative outcomes.
Approximately 25% of all SSIs are caused by Staphylococcus aureus.
Approximately 40% of deaths after gynecologic surgery are related to pulmonary emboli. Although the initial venous injury most often occurs at the time of the operation, approximately 15% of symptomatic emboli do not present until the first week after discharge from the hospital.
Using the Caprini score, women in the very-low-risk group have less than a 3% risk of venous thromboembolism (VTE), women in the moderate group have a 10% to 30% risk, and women in the high-risk groups have a more than 30% risk of a VTE.
Low-molecular-weight heparin (LMWH) is superior to standard unfractionated heparin because it has a longer half-life, almost 100% bioavailability, dose-independent clearance, and a more consistent anticoagulation effect from dose to dose.
A meta-analysis of studies evaluating high-risk procedures found perioperative and postoperative LMWH administration to be equally effective.
In general, warfarin should be held for at least 5 days before surgery and the international normalized ratio should be less than 1.5 before incision.
Therapeutic dose aspirin should be held for 7 days before surgery. Once-daily dosing of baby aspirin (81 mg/day) can usually be continued.
Factor Xa inhibitors should be held for 2 to 3 days before surgery, depending on the individual drug’s half-life. Direct thrombin inhibitors should be held for 2 to 4 days before surgery, depending on renal function.
Patients with bleeding disorders usually present early in their lives with bleeding. It is estimated that approximately 1% to 2% of patients in the United States have some type of bleeding diathesis, the most common of which is von Willebrand disease.
Patients on chronic steroid therapy should receive their usual preoperative dose of steroids on the day of surgery. Any further administration of steroids should be done using a risk-assessment model. If there is a clinical concern of adrenal insufficiency, perioperative stress-dose steroid administration appears to carry minimal risk compared with the risk of adrenal crisis.
Pulmonary function tests of lung volumes and flow rates are only indicated to evaluate women with a history or physical findings suggestive of restrictive or obstructive pulmonary disease.
Predisposing factors that increase the incidence of atelectasis include morbid obesity, smoking, pulmonary disease, and advanced age. Increased pain, the supine position, abdominal distention, impaired function of the diaphragm, and sedation also contribute to decreased lung volumes and reduced dynamic measurements of pulmonary function postoperatively.
The excessive mortality rate associated with a noncardiac operative procedure within 3 months of an acute myocardial infarct is 27% to 37%. After a 6-month interval, the chance of a reinfarction is 4% to 6% with elective operations.
The routine use of beta-blockers perioperatively to reduce the risk of nonfatal myocardial infarction is no longer practiced because of the increased risk of death, nonfatal stroke, hypotension, and bradycardia. As a result, the common practice of perioperative beta-blockade has given way to its selective use.
The administration of prophylactic antibiotics solely to prevent endocarditis is no longer recommended for patients who undergo genitourinary or gastrointestinal tract procedures.
Preoperative evaluation can involve both the art and science of clinical medicine. Optimal preparation for the operation facilitates a successful result and protects the patient and the physician.
The task of obtaining preoperative information serves two goals. The first is to ensure that the procedure is appropriate for the patient’s diagnosis, relying heavily on the physician-patient relationship. The second goal, just as crucial as the first, is ensuring that the patient is safe for the procedure and that comorbidities are appropriately addressed. Some comorbidities will require further consultation with other specialists, and it is important for the gynecologic surgeon to recognize when consultation is needed.
The gynecologic surgeon, as leader of the surgical team, has a responsibility to prepare the patient, her family, and the surgical team for the surgical procedure. Even in emergency situations, preoperative preparation should be detailed and complete. Most surgical procedures are major events in a patient’s life and can be accompanied by anxiety and apprehension in anticipation of surgery. It is not uncommon for patients to experience ambivalence when deciding to have an operation, elective or emergent. In all cases it is important for the surgeon to outline the natural history of the gynecologic disease and options for management. The risks, benefits, and alternatives must be discussed. The impact of a surgical intervention on normal body function, sexuality, and cosmesis should also be addressed. If the patient is ambivalent about the need for a surgical procedure, a second opinion may be warranted and should be offered. Some third-party payer programs may require patients to obtain a second opinion before elective gynecologic surgery.
It is the surgeon’s responsibility to protect the patient’s privacy and dignity throughout the perioperative period. The surgeon must appreciate that the preoperative period may be one of great psychological stress for the patient and her support team. Emotional responses may include vulnerability, helplessness, and grief associated with loss of a reproductive organ. The surgeon-patient relationship extends beyond the legal obligations. An important aspect of this relationship is that the surgeon and patient partner in shared decision making. Trust is established via mutual respect and open communication.
Preoperative consultation with the surgeon is a crucial first step in successful surgery. Ideally, the surgeon, patient, and her selected support team meet for a confidential consultation. A thorough and detailed history and physical examination should be performed during the surgical consultation. A number of studies have demonstrated that the most significant risk factors for postoperative morbidity are preoperative conditions. Known or unsuspected medical illnesses may affect the operation, anesthesia, and postoperative course and may preclude the procedure altogether. It is also important to evaluate the impact of the gynecologic diagnosis on other organ systems, such as a pelvic mass on the ureters or menorrhagia on hemoglobin level.
This chapter outlines the preoperative preparations for gynecologic surgery and perioperative management considerations. The preparations and plans for surgery extend into the postoperative period in a continuous spectrum. Thus several topics will be introduced here and discussed further in Chapter 25 . Emphasis is placed on obtaining a complete history, performing an adequate physical examination, counseling the patient, establishing informed consent, and perioperative planning to reduce complications associated with gynecologic surgery .
A detailed complete history not only obtains information but may also help relieve the patient’s fears and anxieties . When the history is obtained in an unhurried manner, the process can be reassuring. The extent and depth of the general history should be tailored to the age and general health of the woman and the surgical procedure that is being recommended. However, even minor operations may have major complications, so it is important to be prepared for all possibilities.
Obtaining a detailed and comprehensive preoperative history includes the use of open-ended questions and directed questions to complete the preoperative picture. A standardized historical questionnaire before the initial consultation is often requested by the surgeon or even required by the surgeon’s institution. With the broadening use of electronic medical records, a patient’s collated medical history may also be available. Regardless, each surgeon develops his or her method of preparation for consultation. Review of the patient’s medical record, obtaining outside records and prior operative reports, and pertinent imaging and pathology reports can be done before the in-person consultation. This can allow for efficient evaluation, consultation, and preoperative referrals if needed.
Although this chapter does not review all the components of a complete history, it may be advantageous to group questions under the specific organ systems. Specific questions should be included to cross-check the review of symptoms. Questions should be included that address prior problems with surgery, anesthesia, or bleeding in the woman or her family. Medication allergies and current medications should be reviewed. Reconciliation of prescribed and over-the-counter (OTC) medications as well as vitamins, herbal medications, and supplements is critical because side effects and interactions with other medications can adversely affect coagulation and wound healing. Approximately 0.5% of the general population and 1.5% of women older than 55 years are receiving continuous glucocorticoids . Thus a specific question about glucocorticoid therapy for chronic medical problems should be included. The patient’s primary care physician (PCP), or subspecialty medical provider, depending on the medication, should be involved in the decision to temporarily stop certain medications before surgery. The patient’s PCP may also be able to provide guidance regarding anticoagulation bridging and stress-dose steroid dosing if either are needed.
Patients often do not recognize aspirin or oral contraceptives as medication; therefore specific questions regarding these medications are needed . General questions regarding smoking, alcohol, exercise tolerance, and recent upper respiratory infections should also be included. Specific questions should be directed toward sensitivity to iodine or latex. Latex allergy is directly responsible for 12% of the perioperative anaphylactic reactions in adult women and for 70% in children. Health care workers are particularly at risk for latex allergy. Women with spinal cord injuries, or those who have had to perform self-catheterization, are at higher risk for latex allergy.
The patient’s contraceptive history, including any recent change, must be known. Ensuring that pregnancy is excluded either through the preoperative history or a pregnancy test is critical before gynecologic surgery. Included with the contraceptive history are key questions concerning possible exposure to viruses such as hepatitis B, hepatitis C, and human immunodeficiency virus (HIV). Also, the surgeon should discuss the possibility and risks of blood transfusion and learn whether there are religious objections if a blood transfusion is needed during surgery.
The preoperative physical examination should answer three basic questions:
Has the primary gynecologic disease process changed since the initial diagnosis?
What is the effect of the primary gynecologic disease on other organ systems?
What deficiencies in other organ systems may affect the proposed surgery and hospitalization?
Observations and findings in the physical examination may prompt further laboratory and diagnostic tests. One of the most important features of the preoperative physical examination is that it should be performed in a thorough and compulsive manner. One should use the same sequence every time to help focus attention on the evaluation of each organ system and to prevent omissions. Two important axioms should be stressed. First, even in emergency situations, it is imperative to perform a thorough physical examination. This should include an evaluation of blood pressure and pulse in the recumbent and sitting positions; orthostatic hypotension and tachycardia are crude indicators of hypovolemia. Second, although it is important to perform a pelvic examination during the initial consultation, it can also be informative to perform a pelvic examination in the operating room immediately before the surgical incision. An exam while the patient is under anesthesia may provide additional information, help avoid intraoperative surprises, and guide the surgical plan.
The general purpose of preoperative laboratory testing is to identify conditions that will alter or aid in perioperative management. Screening tests are used to find unsuspected asymptomatic conditions that may affect the anticipated surgical procedure. Preoperative laboratory tests may also help establish the extent of known disease and may influence the scheduling of elective surgery. Being selective in ordering preoperative test avoids unnecessary costs associated with test results that would otherwise not affect the surgical plan . Additionally, special imaging procedures may be needed to determine the effects of pelvic disease on other organ systems.
Age-appropriate screening tests should be reviewed with each patient before gynecologic surgery. Papanicolaou (Pap) tests should be up to date before elective gynecologic surgery. Mammograms should at least be discussed with women 40 years and older, and colonoscopy should be discussed with women older than 50 years.
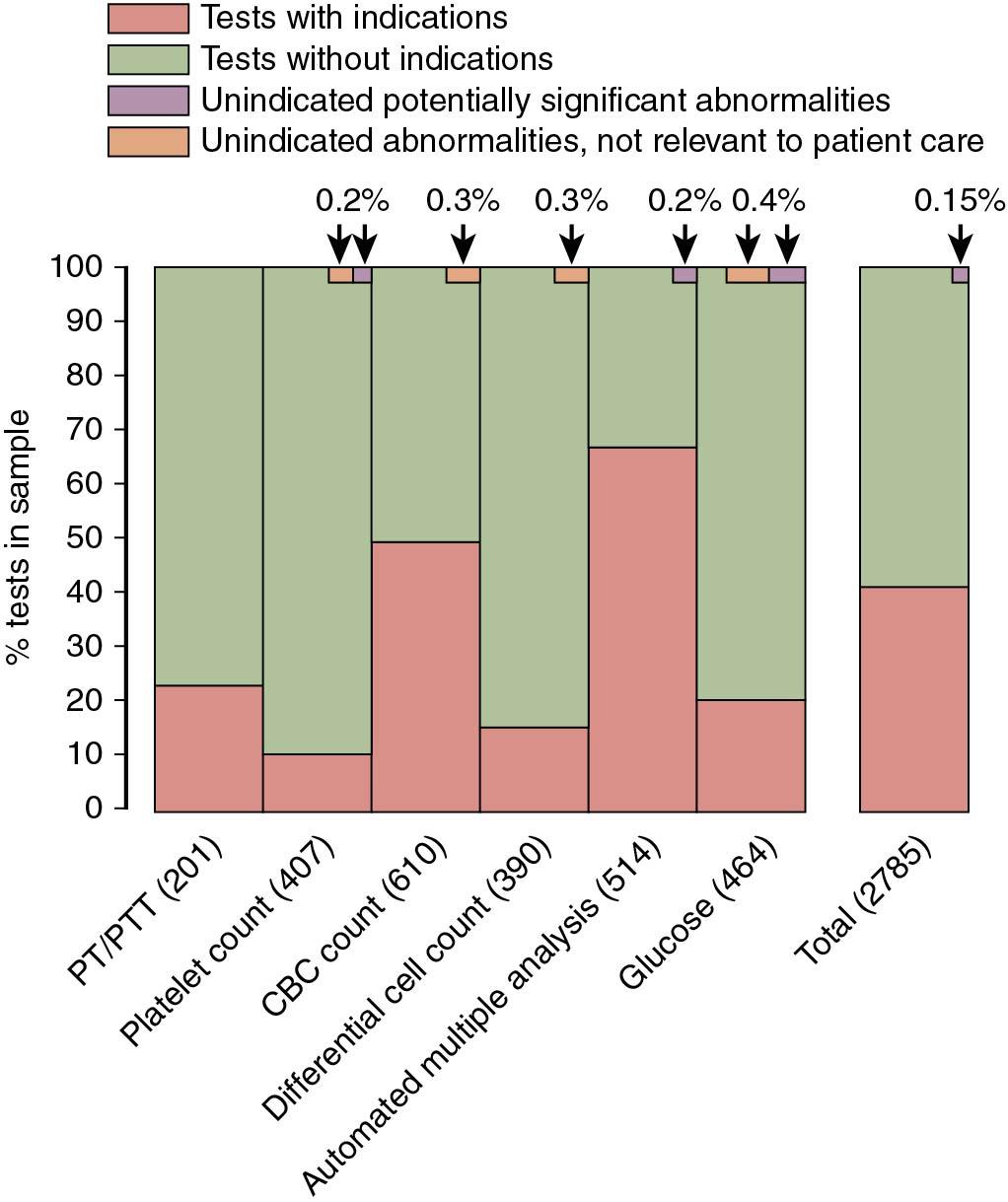
There is debate over which preoperative laboratory procedures should be standard. Attention has been drawn to the cost-benefit ratio of preoperative screening. Although the cost of each individual test is usually low, the aggregate costs can be substantial. In a classic study, Kaplan and colleagues retrospectively studied the usefulness of preoperative laboratory procedures. They estimated that 60% of routinely ordered tests, such as differential cell count, platelet count, and 12-factor automated body chemistry analyses, would not have been performed if tests had been ordered only for an indication discovered by history or physical examination. Most important, only 0.22% of these tests demonstrated an abnormality that might influence perioperative management ( Fig. 24.1 ). The final conclusion in their assessment of 2000 patients undergoing elective operations was that in the absence of specific indications, most routine preoperative laboratory tests do not significantly contribute to patient care and could be eliminated ( ). Additionally, the current American Society of Anesthesiologists (ASA) Practice Advisory for Preanesthesia Evaluation states that routine preoperative tests, defined as a test ordered in the absence of a clinical indication or purpose, should not be ordered. Preoperative tests should be ordered for indicated purposes that guide or optimize perioperative care ( ).
However, a preoperative complete blood cell count and blood type and antibody screen should be performed before most major gynecologic surgeries. In the setting of anemia, the risks and benefits of proceeding with gynecologic surgery should be considered. It is important that the blood bank have the capability of providing cross-matched blood within a reasonable period if serious intraoperative bleeding were to occur. Routine preoperative coagulation studies are not cost effective and rarely provide useful clinical information unless indicated by history and physical examination, as the patient’s menstrual history should identify women with bleeding disorders.
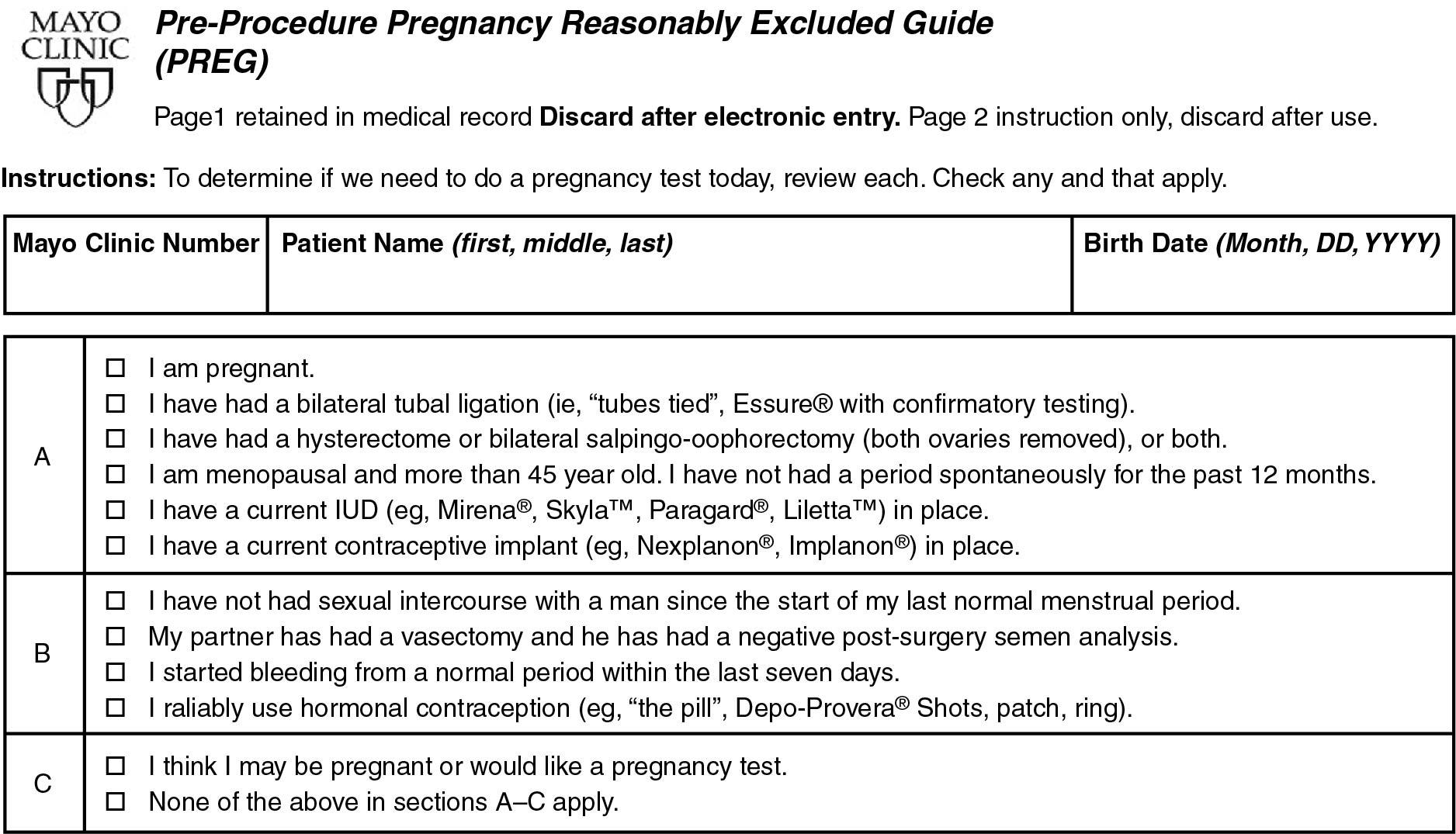
Other individualized preoperative laboratory testing should be determined based on the age of the woman, extent of the surgical procedure, and findings at the time of complete history and physical examination. It may be indicated to order limited blood screening tests for women older than 40 years or who have positive family histories or questionable histories of hepatic or renal disease. Determining the preoperative creatinine or blood urea nitrogen (BUN) level is especially important if the woman is going to be treated with antibiotics excreted by the kidneys. A pregnancy test may be appropriate, depending on contraceptive and sexual history, but a preprocedure pregnancy risk questionnaire may also be used as an effective history-based screen on the day of surgery for women 18 years and older ( Fig. 24.2 ) ( ). However, a preprocedure pregnancy test should almost always be performed if the patient is a teenager, as menstrual history is at best an imperfect indication of an early pregnancy. Serum electrolyte levels are ordered for women taking diuretics or those with a history of renal disease or heart disease. Also, serum electrolyte levels should be evaluated in women with vomiting, diarrhea, ileus, bowel obstruction, or any condition that affects electrolyte balance. Ideally, abnormal results from any laboratory test ordered preoperatively should result in some change in perioperative management.
Routine chest radiographs on all patients often do not affect perioperative management in elective gynecologic surgery. A history and physical examination are sufficient for screening, and chest radiographs should be obtained in patients with positive findings. A meta-analysis of studies of routine preoperative chest radiographs demonstrated that false-positive results leading to invasive procedures and associated morbidity are more common than the discovery of new findings leading to a change in management . However, chest films should be ordered for women who are current or former smokers, women with cardiac or pulmonary symptoms, immigrants who have not had a recent chest film, and women older than 70 years ( ), although there appears to be institutional variability regarding the absolute age cutoff.
A baseline preoperative electrocardiogram (ECG) has been found to be cost effective in asymptomatic women 60 years and older without a history of cardiac disease or significant risk factors. An ECG may also be indicated in younger women with a history of smoking and those with diabetes or renal disease, depending on the severity.
Based on the complete history, physical examination, and preoperative testing, the gynecologic surgeon should determine whether consultation with other specialists is necessary. This decision should take into account the severity of comorbidities and the complexity of the proposed operation.
One of the primary responsibilities of the gynecologic surgeon is to educate the patient and her support team about the anticipated surgical procedure, hospitalization, and recovery. Informed consent is an important principle to ensure that the patient’s right to self-determination is respected. The ethical concept of the process of informed consent includes two components, comprehension and free consent . Throughout the educational process, questions from the patient or her support team should be welcomed. Educating the patient can also address anxiety. Written information, when available, can be helpful. Psychological preparation of the patient’s support team is equally important, and arrangements for appropriate communication with the patient’s family or support team during the operation should be made.
Few concepts bring more ambivalence and concern to the physician than the doctrine of informed consent. In the present medicolegal climate, the absence of informed consent is cited as a major problem in many lawsuits. Some of these issues are discussed further in Chapter 6 . It is important to differentiate between the concepts of consent and informed consent. Consent involves a simple yes-no decision, but informed consent is an educational process that also includes shared decision making between surgeon and patient . To obtain informed consent, the surgeon must explain the following to the patient in understandable terms: the nature and extent of the disease process; the nature and extent of the contemplated operation; the anticipated benefits and results of the surgery, including a conservative estimate of successful outcome; the risks and potential complications of the operative procedure; alternative methods of therapy; and any potential changes in sexual, reproductive, and other functions. The surgeon should also discuss with the patient what the operation will not accomplish. Questions from the patient should be encouraged and addressed. Any details specific to the situation should be clarified in the consent note in addition to stating that the procedure, alternative treatments, and risks have been discussed and questions have been answered. The possibility of unanticipated pathologic conditions should be discussed with the woman and permission obtained on the written consent form for the most extensive operative procedure that may be necessary.
One of the greatest dilemmas in the doctrine of informed consent is the extent and depth of discussions concerning potential complications of an operation. Attorneys who specialize in defending gynecologic surgeons in medical malpractice litigation strongly advise discussing the risks of all major complications, including death from surgery and rare, serious complications, such as urinary tract fistulas after hysterectomy. Studies have shown that approximately 70% of patients do not read the consent form before signing it. Ideally, to protect the surgeon, another member of the health care delivery team should witness the final discussion of the informed consent process. The surgeon should document critical highlights of this discussion in the patient’s medical record.
The gynecologic surgeon must not only educate his or her patient but must be prepared to discuss other information that the patient has received, including information from the lay press and Internet. During the preoperative educational process, so much information may be given that it causes confusion. Studies have noted that the more information given, the less information is actually retained, much less correctly retained. A study by Sandberg and colleagues has noted that during the preoperative evaluation, information given by anesthesiologists and other health care providers vastly exceeds the short-term capacity of patients ( ). Thus it is extremely helpful to provide written preoperative instructions and important information.
Most procedures and orders are accomplished on an outpatient basis because most patients undergo same-day admission before elective surgery. Preoperative orders should be standardized to avoid omissions, and electronic order sets are standard at most institutions. Orders individualized to a patient should be written in specific detail to avoid confusion by nursing and other hospital personnel.
Before presentation to the hospital, the patient should be provided with a list of specific instructions for the 24 hours before surgery. If an enhanced recovery pathway is being used, the patient can usually eat solid food up until midnight and clear liquids until 30 minutes before presenting to the hospital . To avoid hypoglycemia, most enhanced recovery after surgery protocols allow patients to eat solid food up to 6 hours before surgery. Clear liquids are emptied from the stomach within minutes; however, fatty foods delay gastric emptying. Incomplete preparation of the upper gastrointestinal (GI) tract increases the risk of aspiration. Studies have documented the safety of allowing inpatients and outpatients to ingest clear liquids up until 2 hours before elective surgery, and this is reflected in current ASA guidelines ( ). The extent of preoperative anxiety does not influence gastric fluid volume or acidity.
Among patients with no or limited comorbidities, the consultation with their anesthesiologist may occur in the preoperative area on the day of surgery. During this time, the anesthesiologist reviews and obtains any additional medical information, evaluates the patient’s airway, determines the ASA risk score for the patient, and writes any preoperative medication orders. Among patients with complex medical histories or comorbidities, prior complications with anesthesia, family history of anesthesia complications, or planned high complexity surgery, a preoperative evaluation with an anesthesiologist in an outpatient clinic a day or more before surgery is warranted. The goal for this evaluation is to ensure all preoperative assessments needed to optimize anesthesia safety have been performed.
Surgeons and anesthesiologists often have to determine whether to continue or interrupt medications during the perioperative period. If the medication is prescribed for a chronic medical illness, it is likely best to continue the drug throughout the perioperative period. However, it is essential to determine whether the drug will adversely affect the course of the anesthesia or surgery and whether it will interact with other drugs to be given during the procedure. It is acceptable for the patient to take oral medications the morning of surgery . The 30 to 60 mL of water needed to swallow the oral medication is negligible compared with gastric fluid volumes.
Anesthesiologists classify surgical procedures according to the patient’s risk of mortality. In 1961, Dripps first published guidelines to determine the risk of death related to major operative procedures. This physical status scale ( Table 24.1 ) has been adopted by the ASA and has been revalidated many times over the years. With minor modifications, these anesthetic risk classes are still widely used. An emergency operation doubles the mortality risks for classes 1, 2, and 3; produces a slightly increased risk in class 4; and does not change the risk in class 5 ( ).
| ASA Physical Status Class | Description |
|---|---|
| 1 | A normal healthy patient |
| 2 | A patient with mild systemic disease |
| 3 | A patient with severe systemic disease |
| 4 | A patient with severe systemic disease that is a constant threat to life |
| 5 | A moribund patient who is not expected to survive without the operation |
Enhanced recovery refers to a bundled process with the aim of attenuating pathophysiologic changes and the stress response occurring with surgery . These processes replace traditional but untested practices of perioperative care with the primary goal of hastening recovery. This challenge to traditional surgical paradigms—such as mechanical bowel preparation, the overnight fasting rule, delayed postoperative feeding, hypervolemia, and intravenous opioids—was first described in Europe in the 1990s ( ). There has been widespread uptake of formalized evidence-based enhanced recovery after surgery (ERAS) protocols internationally, particularly in colorectal surgery. Adoption of ERAS has resulted in an average reduction in length of stay of 2.5 days ( ; ) and a decrease in complications by as much as 50% . Similarities between gynecologic oncology procedures and those performed in surgical specialties such as colorectal surgery suggest that patients with gynecologic cancer may obtain comparable benefits. Data also suggest women undergoing benign gynecologic surgery, including minimally invasive surgery (MIS), benefit from perioperative management on an ERAS pathway.
In one investigation of patients undergoing gynecologic surgery, 241 patients (81 complex cytoreductive, 84 staging, and 76 vaginal surgery cases) were managed with an ERAS protocol and compared with 235 historical controls matched by procedure ( ). The protocol included omission of preoperative fasting ( ), use of carbohydrate loading ( ; ), omission of mechanical bowel preparation ( ), use of preemptive analgesia, nausea and vomiting prophylaxis, and maintenance of perioperative euvolemia ( ). Laparotomy wounds were injected with bupivacaine because epidural analgesia was not used for patients undergoing laparotomy in this series ( ). Intrathecal analgesia was used in more than 40% of vaginal cases in this series. Nasogastric tubes ( ), surgical drains ( ), and intravenous patient-controlled analgesia was avoided or omitted, whereas early feeding ( ; ; ), laxative use, and early mobilization were encouraged ( Table 24.2 ). The ERAS pathway achieved the greatest benefit in patients undergoing complex cytoreduction for ovarian cancer, of whom 57% underwent colonic or small bowel resection. Patient-controlled anesthesia use decreased from 99% to 33%, and total opioid use decreased by 80% in the first 48 hours with no increase in pain scores. Hospital stay was reduced by 4 days with 30-day cost savings of more than $7600 per patient (18.8% reduction). In benign vaginal cases, mean pain scores significantly improved and hospital stay was significantly reduced by 1 day with the use of intrathecal analgesia. Ninety-five percent of patients rated satisfaction with perioperative care as excellent or very good. Other investigations in patients undergoing gynecologic surgery have shown that ERAS is safe and confers significant benefits in hospital length of stay, pain control, and overall recovery ( ; ; ; ; ; ; ).
| P REOPERATIVE | |
| Diet | Evening before surgery: carbohydrate-loading drink; may eat until midnight May ingest fluids up to 4 hours before procedure Eliminate use of mechanical bowel preparation; rectal enemas still performed |
| I NTRAOPERATIVE | |
| Analgesia before OR entry | Celecoxib 400 mg PO once Acetaminophen 1000 mg PO once Gabapentin 600 mg PO once |
| Postoperative nausea and vomiting prophylaxis | Before incision (± 30 min): dexamethasone 4 mg IV once + droperidol 0.625 mg IV once Before incision closure (± 30 min): granisetron 0.1 mg IV once |
| Fluid balance | Goal: maintain intraoperative euvolemia Decrease crystalloid administration Increase colloid administration if needed |
| Analgesia | Opioids IV at discretion of anesthesiologist supplemented with ketamine or ketorolac After incision closure: injection of bupivacaine at incision site |
| Anesthesia in complex vaginal surgery | Subarachnoid block containing bupivacaine and hydromorphone (40-100 μg) Sedation versus “light” general anesthetic at the discretion of the anesthesiologist Ketorolac 15 mg at the end of the procedure for patients able to tolerate it No wound infiltration with bupivacaine in this cohort |
| P OSTOPERATIVE | |
| Activity | Evening of surgery: out of bed greater than 2 hours, including 1 or more walks and sitting in chair Day after surgery and until discharge: out of bed greater than 8 hours, including 4 or more walks and sitting in chair Patient up in chair for all meals |
| Diet | No nasogastric tube (NGT); if NGT used intraoperatively, remove at extubation Patient encouraged to start low-residue diet 4 hours after procedure Day of surgery: 1 box of liquid nutritional supplement. Encourage oral intake of at least 800 mL of fluid, but no more than 2000 mL by midnight. Day after surgery until discharge: 2 boxes of liquid nutritional supplement. Encourage daily oral intake of 1500-2500 mL of fluids. Osmotic diarrhetics: Senna and docusate sodium; magnesium oxide; magnesium hydroxide prn |
| Analgesia | Goal: no IV patient-controlled analgesia (PCA) Oral opioids Oxycodone 5-10 mg PO every 4 hours as needed for pain rated 4 or greater or greater than patient stated comfort goal (5 mg for pain rated 4-6 or 10 mg for pain rated 7-10). For patients who received intrathecal analgesia start 24 hours after intrathecal dose given. Scheduled acetaminophen * Acetaminophen 1000 mg PO every 6 hours for patients with no or mild hepatic disease; acetaminophen 1000 mg PO twice daily for patients with moderate hepatic disease; maximum acetaminophen should not exceed 4000 mg per 24 hours from all sources. Scheduled NSAIDs Ketorolac 15 mg IV every 6 hours for 4 doses (start no sooner than 6 hours after last intraoperative dose); then, ibuprofen 800 mg PO every 6 hours (start 6 hours after last Ketorolac dose administered) If patient unable to take NSAIDs Tramadol 100 mg PO four times a day (start at 6 a.m. day after surgery) for patients less than 65 years of age and no history of renal impairment or hepatic disease; tramadol 100 mg PO twice daily (start at 6 a.m. day after surgery) for patients 65 years of age or older or creatinine clearance less than 30 mL/min or history of hepatic disease. Breakthrough pain (pain greater than 7 more than 1 hour after receiving oxycodone) Hydromorphone 0.4 mg IV once if patient did not receive intrathecal medications; may repeat once after 20 minutes if first dose ineffective. IV PCA Hydromorphone PCA started only if continued pain despite two doses of IV hydromorphone |
| Fluid balance | Operating room fluids discontinued upon arrival to floor Fluids at 40 mL/hour until 8:00 a.m. on day after surgery, then discontinued Peripheral lock IV when patient had 600 mL PO intake or at 8:00 a.m. on day after surgery, whichever came first. |
* Doses for patients greater than 80 kg and less than 65 years of age; doses adjusted as appropriate for patients less than 80 kg and/or 65 years of age or older.
The popularity of thoracic epidural anesthesia (TEA) after major open gynecologic surgery is due to its effectiveness in controlling pain and the quicker return of bowel function seen in patients with epidural anesthetics ( ). However, the role of TEA in an ERAS care plan is less clear because it can compete at times with some of the ERAS goals such as early ambulation and voiding. The use of TEA has been associated with more interventions to treat hypotension, longer length of hospital stay, and more complications in one series of early-stage endometrial cancer patients ( ). The estimated length of stay in most ERAS pathways for abdominal hysterectomy is approximately 1 to 2 days, and MIS hysterectomies are most often performed as outpatient procedures. TEA in these settings not only represents poor use of resources but also will likely interfere with the expected expedient discharge from the hospital. Further study is needed to determine whether TEA or other local or regional analgesic approaches in radical abdominal procedures such as ovarian cancer debulking improve the return of bowel function or shorten hospital stays.
If GI symptoms are present before gynecologic surgery, preoperative endoscopy or imaging studies of the GI tract should be considered to better understand the cause of these symptoms. The effect of nausea, vomiting, or diarrhea on serum electrolyte levels and on the nutritional status of the patient also needs to be evaluated. The evaluation should be individualized to determine whether a primary gynecologic process is causing the GI symptoms.
If a bowel preparation is necessary, a single day of an oral solution can be used. Magnesium citrate, sodium phosphate (Fleet phospho-soda), and polyethylene glycol (PEG; GoLYTELY) are the three most commonly used agents. Oliveria and colleagues reported a large randomized trial comparing sodium phosphate and PEG-based oral lavage solutions. The efficacy of the two preparations was similar. However, there was superior subjective patient tolerance to the 90-mL dose of sodium phosphate ( ). Care must be taken in selecting patients who are to receive oral sodium phosphate as a bowel preparation because it may lead to hypokalemia, has been associated with acute phosphate nephropathy, and is contraindicated in women with hepatic, renal, or heart disease. As a result, the U.S. Food and Drug Administration (FDA) issued a warning in late 2008 regarding the use of all oral sodium phosphate preparations when used as a bowel cleanser. Special care must be taken in patients older than 55 or younger than 18, patients taking medications that can affect kidney function, and patients who are dehydrated.
Depending on the surgical procedure being performed, operative site marking may be required. Most institutions mandate site marking to be performed in the setting of surgical procedures that involve or remove one or both organs or structures that are paired. This is controversial in gynecologic surgery because the preoperative determination of adnexal laterality is not always reliable. If site marking is done, it should performed in the preoperative area while the patient is awake and nonsedated. The patient should participate in Universal Protocol and confirm which organ(s) will undergo surgery . Universal Protocol and site marking reduce the risks of wrong site, wrong procedure, and wrong person operations ( ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here