Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vast improvements have been made in the diagnosis and therapy of fetal anomalies as a result of advances in imaging and surgical technology. Nowhere is this more applicable than in the fetal spine. Ultrasonography is the primary imaging modality for fetal evaluation and helps distinguish normal from abnormal spine development and provides valuable information about spinal anomalies. Magnetic resonance imaging (MRI) is complementary to ultrasonography, as it has the advantage of better detection and depiction of associated central nervous system (CNS) and non-CNS anomalies that may have a significant impact on postnatal neurologic function and quality of life.
The major lesion of the CNS currently amenable to fetal diagnosis and intervention, and a driving force behind the use of highly detailed prenatal imaging, is open spinal dysraphism, commonly referred to as myelomeningocele (MMC) . The osseous detail and real-time evaluation of lower extremity configuration, position, and motion detectable with ultrasonography, combined with soft tissue and parenchymal assessments with MRI, provide the maternal-fetal-medicine specialist and pediatric neurosurgeon with highly detailed anatomic information. Because fetal surgery is not without risk to the mother and the fetus, obtaining accurate information is essential for determining surgical appropriateness and presurgical planning. When significant congenital anomalies are present outside of the CNS, information about associated spinal abnormalities is valuable for counseling and parental decision making regarding the management of the pregnancy, labor, and delivery or interruption of the pregnancy.
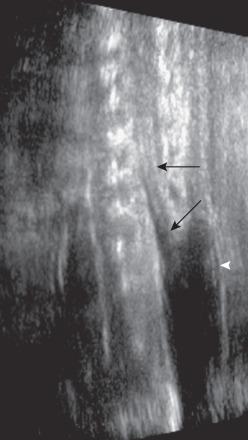
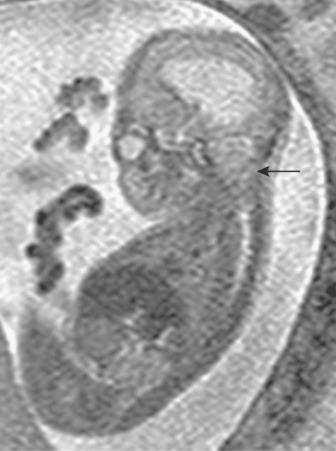
The accuracy of identifying spinal anomalies during nontargeted screening ultrasonography varies, depending on the skill and experience of the operator. The accuracy of a referral center performing detailed targeting studies for a suspected neural tube defect (elevated maternal serum α-fetoprotein) is close to 100%. A detailed protocol should be performed. Axial and longitudinal views of the spine should be obtained. Spine ossification progresses from 10 to 22 weeks' gestation. By 16 weeks' gestation, neural arch ossification is complete to L5. By 19 weeks, S1 is typically ossified, and by 22 weeks, S2 as well. Everted pedicles are best visualized in the transverse plane. An overlying sac may be imaged in transverse and longitudinal planes, with higher-frequency transducers showing cord tethering and placode contents ( Fig. 42.1 ).
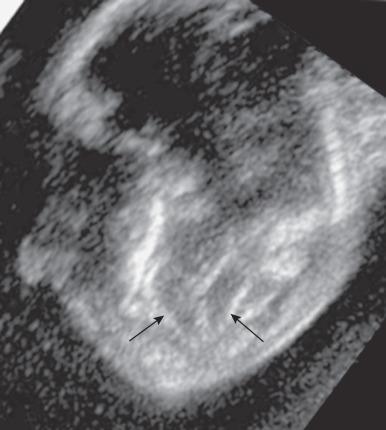
Because fetuses with open neural tube defects typically have Chiari II malformations, the fetal brain should be scanned initially. A small cisterna magna with rounded, small cerebellum is termed the banana sign and is 99% sensitive in the diagnosis of a Chiari II malformation ( e-Fig. 42.2 ). The frontal bones may be concave and is termed the lemon sign. This sign is less specific, however, being present in 1% to 2% of normal fetuses, and may resolve by the third trimester. Ventriculomegaly may be present.
Fetal MRI is typically performed on 1.5 Tesla (T) magnets, although some centers are now performing fetal MRI at 3.0 T. A surface coil (torso, cardiac, or body phased-array) is used to maximize image quality. A standard localizer sequence generally facilitates quick identification of fetal position. This is used to guide the initial imaging plane, which should be appropriately aligned with the fetal anatomy in question. Subsequent imaging sequences are prescribed in orthogonal planes with respect to the fetal spine, each adjusted from the preceding image set, to account for changes in fetal position.
Ultrafast sequences are used to minimize image degradation by maternal and fetal movements. T2-weighted images provide most of the diagnostic information for the examination: single-shot fast spin echo (SSFSE) or half-Fourier acquisition single-shot turbo spin echo (HASTE) sequences at 2- to 4-mm slice thickness. Fast T1-weighted gradient echo imaging is frequently attempted but shows satisfactory contrast resolution and signal-to-noise ratio only after approximately 26 weeks' gestation. Extremely rapid gradient echo, echo planar imaging, or susceptibility weighted imaging, with their high sensitivity to paramagnetic susceptibility effect, may be used to identify osseous and vascular structures, hemorrhage, and mineralization. Steady-state free precession imaging, particularly at 3T, can improve visualization of spinal segments. Diffusion-weighted imaging can assess for acute ischemia.
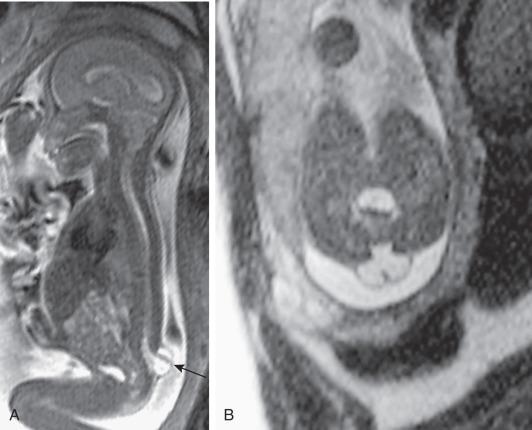
Abnormalities in formation of the primitive neural tube (neurulation) may result from defects in disjunction, the process by which the neural tube separates from the overlying ectoderm (see also Chapter 43 ). MMC occurs in the third week of gestation, when a localized failure of disjunction occurs. This failure may occur anywhere along the length of the spinal cord, but it is most common in the lumbar region. The resulting lesion is an open spinal canal with a flat neural placode instead of a cylindrical spinal cord. Prenatally, ultrasonography and MRI reveals the failure of neurulation in as a posterior osteocutaneous defect. In the presence of elevation of the neural placode, secondary to expansion of the subarachnoid space, the lesion is referred to as MMC ( Fig. 42.3 ). This is distinguished from myeloschisis, also known as myelocele , where an open neural tube defect exists, but the subarachnoid space is not expanded, and the neural placode remains within the confines of the dysraphic spinal canal ( Fig. 42.4 ).
The neurologic deficits sustained by the fetus are postulated to occur in stages, a “two-hit” hypothesis. The first “hit” is the original defect in neurulation that creates the dysraphism and any associated myelodysplasia. The second “hit” is the secondary chemical or physical trauma (or both) to the neural tissue as a result of its exposure to the intrauterine environment.
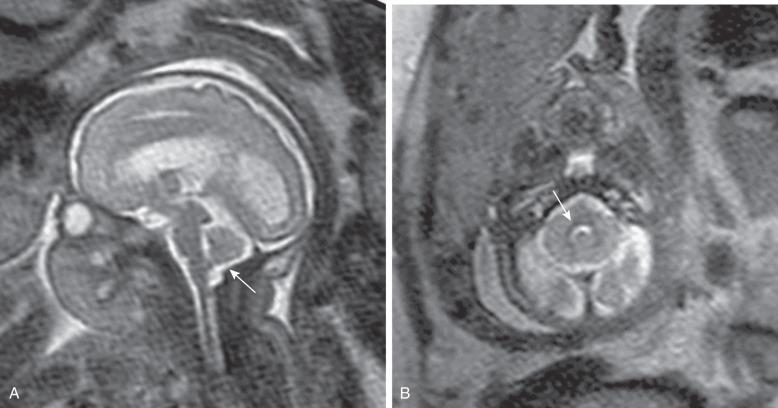
A unified theory regarding the pathogenesis of the associated Chiari II malformation suggests that the open spinal canal and associated free drainage of cerebrospinal fluid (CSF) promote collapse of the primitive ventricular system and cause lack of expansion of the rhombencephalic vesicle, from which the posterior fossa develops. This lack of distension leads to an abnormally small posterior fossa and subsequent hindbrain herniation. However, the Chiari II malformation is a pancerebral anomaly, affecting broad areas of the brain. Abnormalities include herniation of the medulla, cerebellar tonsils, and vermis through the foramen magnum; a small posterior fossa; “beaking” of the tectum of the midbrain; an enlarged massa intermedia of the thalami; partial or complete callosal dysgenesis; and structural changes in the skull ( Fig. 42.5 ). Migrational abnormalities, particularly subependymal gray matter heterotopia, are commonly seen. The cause of hydrocephalus in patients with MMC is debated. Current theories include mechanical obstruction secondary to anatomic changes associated with the Chiari II malformation and dysfunctional CSF absorption. Clinically, hydrocephalus may not be present at birth but may become apparent after early postnatal closure of the defect.
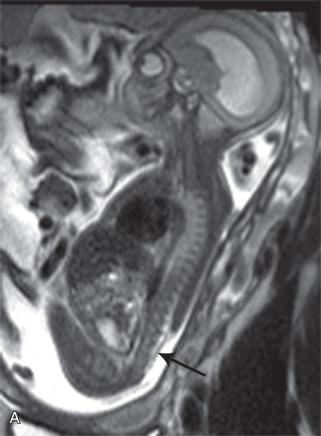
Prenatal repair of MMC is now standard of care in the United States. While the initial intent was to preserve distal neurologic function by covering the exposed spinal cord, and some improvement in distal sensorimotor function is expected, the primary benefit of prenatal repair is the reduction in hindbrain herniation ( Fig. 42.6 ) and substantially decreased need for ventricular shunting.
Ultrasound examination of fetuses with MMC at 18 weeks' gestational age frequently shows lower limb movements that correlate with the movements of unaffected fetuses, indicating that loss of motor function in these patients likely occurs later in gestation. Another argument for in utero repair of MMC came from the lesser degrees of neurologic deficits in many of the forms of closed spinal dysraphism in which the neural elements remain covered by skin (e.g., lipomyelomeningocele). The Management of Myelomeningocele Study (MOMS) trial found that fetuses who underwent in utero MMC repair demonstrated superior standardized test scores for motor skills and that twice as many children were walking independently at 30 months of age compared with those randomized to postnatal surgery. MMC is generally not a fatal disease in utero or postnatally, and most prenatally diagnosed infants survive to lead productive lives. Fetal surgery is associated with premature delivery and its attendant complications, including fetal/neonatal loss. Maternal complications may range from uterine rupture and hemorrhage to deep venous thrombosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here