Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Posterior reversible encephalopathy syndrome (PRES) is a clinico-radiologic disorder characterized by rapidly progressive neurologic symptoms and a characteristic pattern of vasogenic edema on neuroimaging.
Neurologic symptoms are usually associated with an increase in blood pressure above baseline.
Malignant hypertension, preeclampsia/eclampsia, medications (especially calcineurin inhibitors), thrombotic microangiopathy syndromes, and sepsis are all associated with the development of PRES.
Pathogenesis involves the breakdown of the blood-brain barrier, either from severe hypertension that exceeds the capacity of cerebral autoregulation or from direct endothelial damage.
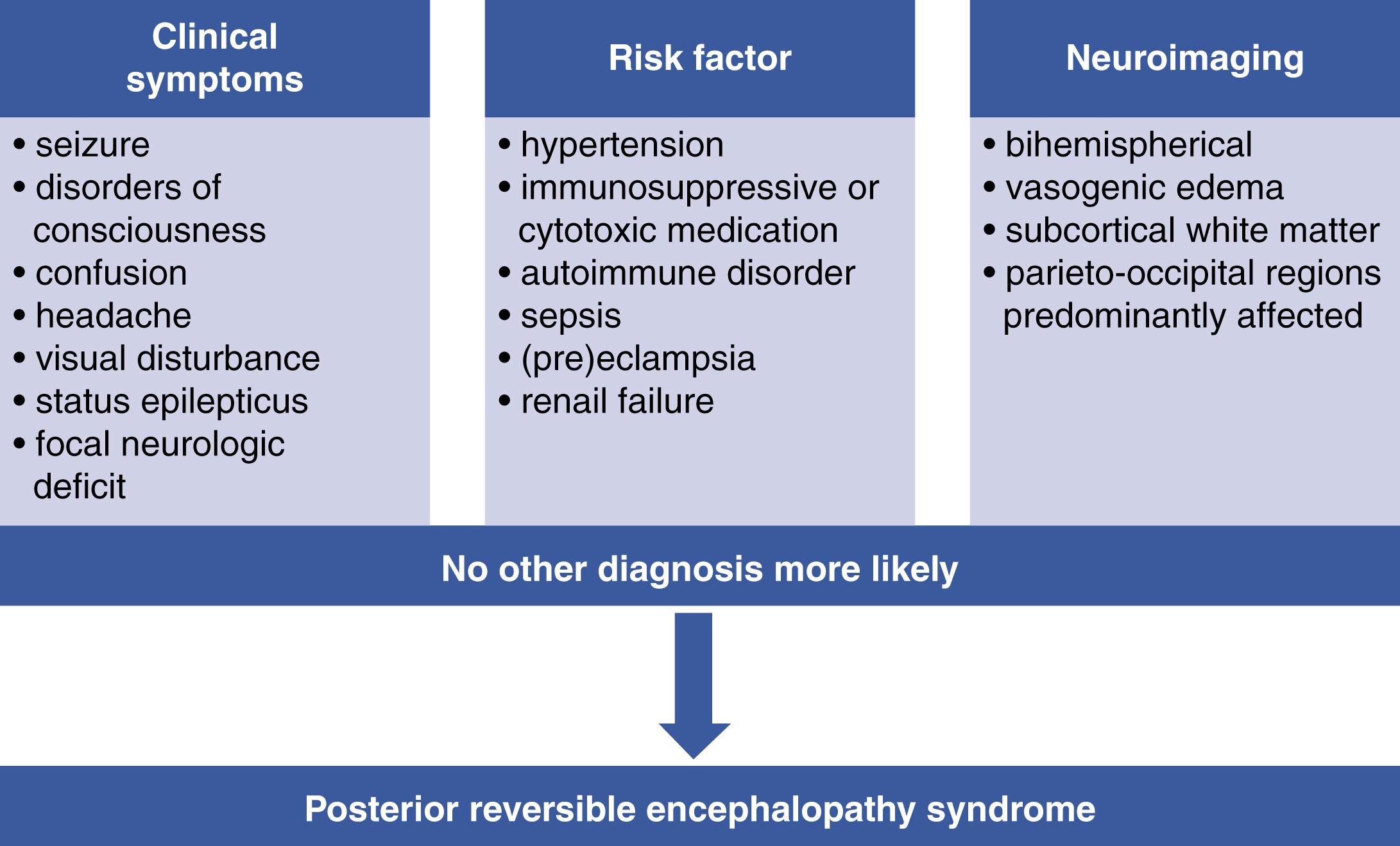
The posterior reversible encephalopathy syndrome (PRES) is a clinico-radiologic disorder that has been increasingly recognized since its first description in 1996. It is defined by subacute onset of neurologic symptoms, in combination with a characteristic pattern of vasogenic edema on imaging. The clinical manifestations are usually of acute or subacute onset and include headache, visual disturbance, confusion, disorders of consciousness, or epileptic seizures. Depending on the lesion site, focal neurologic deficits of variable extent may occur. Arterial hypertension and/or blood pressure fluctuations are widespread in the development of PRES and can be observed at the time of the neurologic manifestation in a substantial proportion of patients. Neuroimaging usually shows bihemispherical vasogenic edema with predominance of the parieto-occipital regions. , However, PRES-typical lesions may affect any area of the central nervous system. , Clinical and radiologic signs are often reversible within days or weeks of the onset of PRES. , In the case of malignant PRES complicated by cerebral ischemia or intracerebral hemorrhage, persistent neurologic damage is possible. ,
The clinical features of PRES are protean and may occur in numerous other neurologic conditions. Therefore, the combination of clinical features, radiologic findings, and a potential causative factor is important for the timely diagnosis of PRES. Unfortunately, there are no uniformly accepted diagnostic criteria, and variable definitions have been used in the literature. Frequently used diagnostic criteria include the following: (1) acute clinical presentation, (2) the presence of a known risk factor for PRES, and (3) magnetic resonance imaging (MRI) findings consistent with PRES. , In addition, reversibility of clinical and imaging findings helps confirm the diagnosis (see Fig. 38.1 ).
Although formally described in 1996, the syndrome now identified as PRES has been recognized for millennia. Eclampsia—clinically and radiologically indistinguishable from PRES and now recognized as one of its subtypes—was described in writings from the Hippocratic era , and may also have been referred to in ancient Egyptian and Vedic medical texts. , With the advent of techniques that enabled accurate measurement of blood pressure, similarities were noted between eclampsia and other disorders where acute neurologic symptoms were associated with elevated blood pressure. In 1914, Vollhard and Fahr used the term “pseudo-uremia” to denote a syndrome of acute neurologic decline in patients with kidney failure where neurologic symptoms appeared to be associated with elevated blood pressure rather than the buildup of uremic toxins. Oppenheimer and Fishberg extended this concept, and in 1928 coined the term “hypertensive encephalopathy” to describe a syndrome of confusion, seizures, and focal neurologic signs in a patient with kidney failure and abrupt fluctuations in blood pressure, where neurologic symptoms were associated with blood pressure increases. Subsequent studies used hypertensive encephalopathy rather nonspecifically to denote any acute neurologic worsening associated with elevated blood pressure that improves with blood pressure control.
Hinchey et al.’s now classic paper identified the characteristic pattern of vasogenic edema that distinguishes PRES from other conditions (such as primary intracerebral hemorrhage, subarachnoid hemorrhage, and acute ischemic stroke) where acute neurologic symptoms can be associated with elevated blood pressure, and established the association of these imaging findings with eclampsia, immunosuppressive therapy after organ transplantation, and kidney failure associated hypertension. Subsequent studies identified a similar constellation of neurologic symptoms and imaging findings in association with sepsis, thrombotic microangiopathies, and administration of multiple targeted therapies used for the treatment of cancer and autoimmune disease. These studies have established a wide spectrum of medical conditions associated with PRES.
Due to the lack of prospective studies and the growing list of associated medical conditions, the true incidence of PRES is unknown. PRES can affect children and adults, , and large retrospective cohort studies show a higher incidence overall in women. , , The many medical conditions associated with PRES can be broadly categorized into (1) conditions associated with abrupt increases in blood pressure, (2) toxicities from medications that may cause both hypertension and direct endothelial damage, (3) thrombotic microangiopathy (TMA) syndromes, (4) preeclampsia/eclampsia, and (5) sepsis ( Box 38.1 ). These broad categorizations significantly overlap (for example, eclampsia and medications can induce a TMA, and all three can be associated with hypertension). PRES is associated with dysregulation of the immune system; however, it is unclear if this association reflects underlying pathophysiologic mechanisms (such as excessive inflammation), toxicities from medications commonly used to suppress immune function, or systemic manifestations (such as hypertension and kidney dysfunction) that often occur in the context of autoimmune disease. , ,
Associated with abrupt hypertension/cerebral hyperperfusion
Uncontrolled essential hypertension
Renovascular hypertension/glomerulonephritis
Cushing disease
Pheochromocytoma
Guillain-Barré syndrome/peripheral autonomic instability
Paroxysmal sympathetic hyperactivity
Acute brain injury (e.g., traumatic brain injury, primary intracranial hemorrhage)
Autoimmune encephalitis
Iatrogenic (vasopressor infusions/triple-H therapy)
Eclampsia
Medication toxicities
Stimulant medications
Calcineurin inhibitors
Chemotherapeutic agents
Immunomodulators
Thrombotic microangiopathy syndromes
Sepsis
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here